Joseph D. Tobias, MD1-3, David P. Martin, MD1,2, Tarun Bhalla, MD1,2
1Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, Columbus, Ohio
2Department of Anesthesiology & Pain Medicine;3Department of Pediatrics
The Ohio State University College of Medicine, Columbus, Ohio (USA)
Correspondence:Joseph D. Tobias, MD, Chairman, Department of Anesthesiology & Pain Medicine, Nationwide Children’s Hospital, 700 Children’s Drive, Columbus, Ohio 43205 (USA); Phone: (614) 722-4200; FAX: (614) 722-4203; E-mail: Joseph.Tobias@Nationwidechildrens.org
ABSTRACT
Attaining peripheral venous access is one of the most commonly performed procedures during the perioperative care of infants and children. Difficulties in obtaining venous access can delay or in rare cases, result in the need to cancel surgical procedures. In emergent situations, vascular access and airway management are key components of a successful resuscitation. Although used initially to facilitate central venous access, ultrasound is being used more commonly to facilitate peripheral venous and arterial access. The following article reviews the applications of ultrasound for routine and difficult peripheral vascular (venous and arterial) cannulation in the pediatric population.
Key words: Ultrasonography; Ultrasound; Catheterization, Peripheral; Vascular Access Devices; Peripheral Arterial Catheterization; Peripheral Venous Catheterization; Pediatric
Citation: Tobias JD, Martin DP, Bhalla T. Ultrasound-guided peripheral venous and arterial cannulation in the pediatric population. Anaesth Pain & Intensive Care 2015;19(3):311-316
INTRODUCTION
Attaining peripheral venous access is one of the most commonly performed procedures during the perioperative care of infants and children. While generally easy and straight-forward, difficulties in obtaining venous access can delay or in rare cases, result in the need to cancel surgical procedures. In emergent situations, vascular access represents the second most critical technical component of perioperative care following airway management.Various factors including obesity, prolonged hospitalizations,multiple previous attempts, prematurity, and co-morbid conditions can increase difficulties with peripheral vascular access.
Alternative routes when routine peripheral venous access fails may include intra-arterial, intramuscular (IM), and intraosseous.1-6 The intra-arterial route is acceptable for a limited number of medications given concerns regarding vascular or tissue damage. The IM route results in delays in uptake and onset and is also only feasible for a limited number of medications.5-7 When access to the circulation is required within seconds, the intraosseous route is recommended and can be used for the administration of resuscitation medications and fluid.1-4,8 We would recommend ready access to the equipment for the establishment of IO access in every anesthetizing location (Figure 1).
Figure 1: Commercially available intraosseous needle for emergent or urgent vascular access. The black top or hub is used to provide the force needed to penetrate the cortex of the bone. It is then removed to allow for the administration of fluids and medications through the needle.
In non-emergent situations, ultrasound imaging can be used to facilitate vascular access in patients of all ages. Although now considered the standard of care for obtaining central venous access, ultrasound is being used more commonly to facilitate peripheral venous and arterial cannulation. This practice has been facilitated by advancements in the design of ultrasound equipment with improvements in both the quality of the image and the portability of the equipment.The following manuscript reviews the applications of ultrasound for placement of peripheral venous and arterial access in the pediatric population.
PERIPHERAL VENOUS CANNULATION
Excessive delays from the inhalational induction of anesthesia to the establishment of peripheral venous access may predispose the patient to morbidity or even mortality related to gastric insufflation, vomiting with aspiration, atelectasis, hypoxemia, hypercapnia, hypothermia, and hemodynamic instability. The inability to obtain venous access may at times result in the need to cancel elective surgical procedures. In the problematic patient, ultrasound may be used to guide vascular access resulting in decreased in preparation time, the ability to place large bore venous cannulas for the rapid administration of blood products, and a decrease in the need for central venous access.9
Although still somewhat novel when compared to the use of ultrasound for central venous access, the successful use of these techniques for difficult venous cannulation has been demonstrated in both the adult and pediatric patient.10-14 The technique is being used in various clinical situations and locations including the operating room, the emergency department, and the inpatient pediatric ward.The efficacy of ultrasound was evaluated in a prospective, randomized trial in 60 adult patients presenting to the emergency department who manifested difficult peripheral venous access, defined as the inability to obtain intravenous access after 3 or more attempts.10 Many of the patients had co-morbid conditions that increased the difficulty of vascular access including obesity, a history of intravenous drug abuse, or chronic medical problems. Patients presenting on odd days were allocated to the ultrasound-guided group while those presenting on even days were allocated to the traditional-approach group. The success rate was greater (97% versus 33), the time to successful cannulation was less (13 versus 30 minutes), and there was a decrease in the number of percutaneous punctures (1.7 versus 3.7) in the ultrasound-guided versus the control group. This resulted in a greater patient satisfaction.
The use of ultrasound for venipuncture and placement of an intravenous cannula was evaluated in 44 children with a mean age of 9.5 months.12 After one failed attempt, the patients were randomized to ultrasound-guided or standard practice. Of note, the clinicians involved in the study received only one hour of training in ultrasound localization of peripheral veins prior to using the technique and real-time ultrasonography was not used. In the ultrasound group, vein localization was performed by the physician who marked the skin overlying the target vessel. Intravenous cannulation was then performed by a pediatric ED nurse, using the skin mark for vessel location. No difference was noted in successful venipuncture on the first attempt between the two groups (57% in both groups). Likewise, no difference was noted in first attempt cannulation rate (35% versus 29%). Despite the negative results of the study, it should be recognized that the study had limitations including limited physician training in the use of ultrasound, cannulation or venipuncture performed by the nursing staff, a small cohort of patients, and lack of real-time ultrasound use as the vein was marked and ultrasound not used during the process.
A subsequent trial in the pediatric population demonstrated more definitively the potential value of ultrasound in facilitating venous cannulation in problematic patients.14 The prospective, randomized study (ultrasound versus traditional technique) included 50 pediatric patients less than 10 years of age in an emergency department setting with two unsuccessful traditional attempts at peripheral intravenous access or a history of difficult access. The overall success rate was 80% in the ultrasound-guided group versus 64% in the traditional attempt group. Additionally, the time to cannulation was decreased (mean of 6.3 vs 14.4 minutes), there were fewer attempts (median of 1 vs 3), and fewer needle redirections (median of 2 vs 10) using ultrasound.
Technique for peripheral venous cannulation: The above-mentioned studies parallel our clinical practice for peripheral venous cannulation as we use ultrasound when superficial identification of appropriate veins is not possible or when traditional attempts have failed. Basic knowledge of the venous drainage system is useful to facilitate identification of the veins using ultrasound. The most commonly used sites are the saphenous vein immediately above the medical malleolus along the medial aspect of the legor as it crosses the medical condyle of the femur into the middle of the thigh. The deep veins of the forearm or upper arm (cephalic and basilic) can also be used. The antecubital area should be avoided in most cases as flexion during positioning may occlude the cannula.
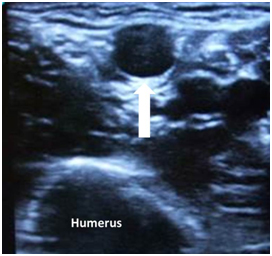
Figure 2: Ultrasound image of a deep venous blood vessel (arrow) in the upper forearm. The deep hypoechoic structure is the humerus
Figure 3: Sonographic image demonstrating that the structure is a vein as it is easily compressible (arrow) with minimal pressure from the ultrasound probe
There are several options for the technique and equipment for peripheral venous cannulation. The hypoechoic vein is identified by its easy compressibility with minimal pressure from the ultrasound probe (Figures 2 and 3). A standard intravenous angiocatheter can be used and advanced into the vein starting with the out-of-plane (transverse) view of the lumen of the vein (Figure 2). While the angiocatheter may not be totally radio-opaque using ultrasound, displacement of the tissues and the vein can be seen as the catheter approaches and then enters the vein. Once blood return is observed in the hub of the needle, the ultrasound probe can be turned to a longitudinal (in-plane) view to watch asthe cannula is advanced off the needle into the vein.When accessing the deeper veins that are identified by ultrasound, standard gauge angiocatheters (22, 20, and 18) that are longer than those used for standard peripheral access may be helpful (Figure 4).The Seldinger technique can be employed using a standard 3 French (20 gauge) or 4 French (18 gauge) central line kit. Alternatively, micropuncture kits are available which facilitate placement of either a 4 French catheter using a 22 gauge needle and 0.018” wire or a 5 French catheter using a 21 gauge needle and a 0.018” wire for vessel entry.
Figure 4: Non-safety, 18 gauge angiocatheter (BD Angiocath™ from Becton, Dickinson and Company, Franklin Lakes, New Jersey) for ultrasound-guided peripheral venous access. These catheters are available in various gauges and lengths to facilitate cannulation of deeper venous structures (1.16 inch or 30 mm length above and 1.88 inch or 48 mm length below)
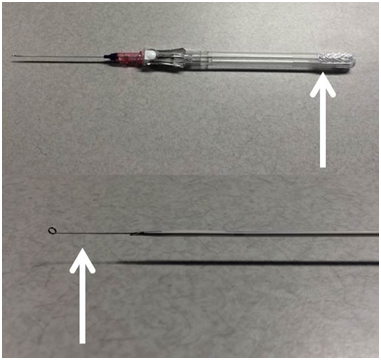
All of these kits are commercially available from the Critical Care Division of Cook Medical (Cook Incorporated, Bloomington, IN, United States). As with the standard Seldinger technique for central venous access, the vein is entered with the needle and the wire threaded through the needle when blood return is noted. Unlike central venous access when a syringe is attached to the needle to aspirate during advancement of the needle, the needle without a syringe is advanced toward the vein during this procedure. There will be free flow of blood out the end of the needle when the vessel is entered.Alternatively, a new angiocatheter with a wire that can pass through the lumen of the needle and into the vein has recently been introduced (AccuCath®, Vascular Pathways, Naples, FL, United States). Once the vein is entered and there is reflux of blood into the angiocatheter. The wire which has a J-tip or coil at the end to avoid damage to the vessel is advanced into the vein (Figure 5). The catheter is then threated over the wire into the vessel.
Figure 5: Angiocatheter with a wire that can pass through the lumen of the needle and into the vein. Once the vein is entered and there is reflux of blood into the shaft of the angiocatheter, the tab at the end of the catheter (arrow) is advanced and the wire enters the vessel. The catheter is then threaded over the wire into the vessel
ARTERIAL CANNULA PLACEMENT
In routine clinical practice, arterial cannula placement is generally performed by palpation of the artery and blind insertion of a cannula.In specific clinical scenarios (hypotension, hypoperfusion, systemic anticoagulation) when standard placement techniques are not feasible or prove unsuccessful, ultrasound may facilitate the procedure. We have also found the use of ultrasound to be helpful when contractures are present from cerebral palsy and other neurologic disorders thereby limiting standard positioning for arterial cannulation.
The initial reports of the use of ultrasound to facilitate arterial cannulation were from the adult literature.15,16 In a prospective trial of 69 adult patients requiring radial artery cannulation, the patients were randomized to the routine palpation technique (blind stick) or ultrasound guidance.15 The use of ultrasound guidance resulted in a higher success rate of cannulation (62% versus 34%) and fewer attempts (average of 1.6 versus 3.1). Subsequent work demonstrated similar efficacy with ultrasound-guided techniques in the pediatric population includinga higher rate of successful arterial cannulation anddecreased time to successful cannulation.17,18Schwemmer et al. prospectively randomized 30 children to ultrasound-guided or the traditional palpation method for cannulation of the radial artery.17 Ultrasound guidance resulted in a higher success rate (100% versus 80%) and fewer attempts (average of 1.3 versus 2.3). The need for practice with the use of ultrasound for such techniques is demonstrated by another group of investigators who reported no difference in success rate, time to cannulation or total number of attempts during arterial cannulation using ultrasound versus the standard technique.19 None of the participants had performed more than 10 ultrasound-guided radial artery cannulations.
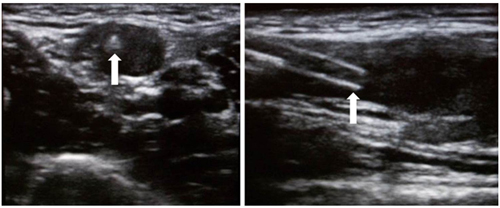
Technique for peripheral arterial cannulation: Three techniques are available for peripheral arterial cannulation including use of a standard angiocatheter which is advanced into the artery, the Seldinger technique (needle, wire, catheter), or a specialized cannula with a wire within the lumen of the needle and catheter assembly(Arrow Arterial Catheterization Kit, Teleflex Corporation, Morrisville, NC, United States). Either an out-of-plane or in-plane technique can be used. We generally start with an out-of-plane technique to identify the artery and observation of the needle or angiocatheter as it enters the lumen (Figure 6).
Figure 6: The left side of the image is an out-of-plane ultrasound view of the radial artery with the tip of the needle or angiocatheter within the vessel lumen (arrow). The transducer can then be turned for an in-plane (longitudinal) view (right side of the image). The catheter (arrow) is threaded off the needle and into the vessel lumen
Following this, the transducer can be turned in-plane to allow for real-time observation of the cannula as it is threaded off the needle and into the lumen of the artery (Figure 6). Alternatively, the use of a Seldinger technique whereby the artery is puncture with a needle followed by guide wire placement may increase the percentage of successful cannulations especially in difficult clinical scenarios. For this technique, we use either a 3 French cannula with a 22 gauge needle and a 0.018” wire in older patients (more than 15-20 kilograms) or a 2.5 French cannula with a 23 gauge needle and a 0.015” wire in neonates and infants.
SUMMARY
There are several clinical benefits that have been demonstrated with the use of ultrasound-guided techniques for vascular access. Although ultrasound was first used for central venous access, its application has expanded to includeperipheral arterial and venous cannulation. The studies which have been reviewed in this manuscript (see above) parallel our clinical practice for peripheral venous cannulation as we use ultrasound when superficial identification of appropriate veins is not possible or when traditional attempts have failed. The use of ultrasound also facilitates the placement of large bore cannulation for resuscitation or the administration of blood products. The technique may also facilitate peripheral arterial cannulation, given the size of the arteries in younger infants and neonates.20,21 The use of ultrasound may limit the risk or morbidity in patient with bleeding disorders or those receiving therapeutic anticoagulation. We have also found it particularly useful for patients with diminished peripheral pulses and in patients with contractures (cerebral palsy) which precludes placement in the distal radial site necessitating use of the radial artery more distally along the forearm.
As with any new technology, practice is necessary to become facile with ultrasound including the machine, its working parameters, and knowledge regarding the appropriate deep vascular structures. The incidence of success will also be increased by having the right machine and the correct equipment (needles, wires, dilators, and cannulae) for vascular access. Regardless of the utility of the technique, all anesthesia providers should be facile with placement of an IO needle as it remains the option of choice during resuscitation when peripheral venous access is not available.
REFERENCES
- Joshi G, Tobias JD. The use of intraosseous infusions in the operating room. J Clin Anesth 2008;20:469-73.[PubMed] doi: 10.1016/j.jclinane.2008.04.014.
- Tobias JD, Ross AK. Intraosseous infusions: A review for the anesthesiologist with a focus on pediatric use. Anesth Analg 2010;110:391-401. [PubMed] doi: 10.1213/ANE.0b013e3181c03c7f.
- Neuhaus D, Weiss M, Engelhardt T, Henze G,Giest J, Strauss J, et al. Semi-elective intraosseous infusion after failed intravenous access in pediatric anesthesia. Paediatr Anaesth 2010;20:168-71. [PubMed] doi: 10.1111/j.1460-9592.2009.03244.x.
- Neuhaus D. Intraosseous infusion in elective and emergency pediatric anesthesia: when should we use it? Curr Opin Anaesthesiol 2014;27:282-7. [PubMed] doi: 10.1097/ACO.0000000000000069.
- Joshi G, Tobias JD. Intentional use of intra-arterial medications when venous access is not available. Paediatr Anaesth 2007;17:1198-202. [PubMed]
- Mauch J, Ringer SK, Spielmann N, Weiss M. Intravenous versus intramuscular epinephrine administration during cardiopulmonary resuscitation – a pilot study in piglets. Paediatr Anaesth 2013;23:906-12. [PubMed] doi: 10.1111/pan.12149.
- Sen S, Chini EN, Brown MJ. Complications after unintentional intra-arterial injection of drugs: risks, outcomes, and management strategies. Mayo Clin Proc 2005;80:783-95. [PubMed]
- Vyskocil JJ, Kruse JA, Wilson RF. Techniques for vascular access when venous entry is impossible: route depends on urgency and the agent to be administered. J Crit Illness 1993;8:539-45. [PubMed]
- Jöhr M, Berger TM. Venous access in children: state of the art. Curr Opin Anaesthesiol 2015;28:314-20. [PubMed] doi: 10.1097/ACO.0000000000000181.
- Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med 2005;46:456-61. [PubMed]
- Costantino TG, Kirtz JF, Satz WA. Ultrasound-guided peripheral venous access vs the external jugular vein as the initial approach to the patient with difficult vascular access. J Emerg Med 2010 ;39:462-7. [PubMed] doi: 10.1016/j.jemermed.2009.02.004.
- Bair AE, Rose JS, Vance CW, Andrada-Brown E,Kuppermann N. Ultrasound-assisted peripheral venous access in young children: A randomized controlled trial and pilot feasibility study. West J Emerg Med 2008;9:219-24. [PubMed][Free full text]
- Schnadower D, Lin S, Perera P, Smerling A,Dayan P. A pilot study of ultrasound analysis before pediatric peripheral vein cannulation attempt. Acad Emerg Med 2007;14:483-5. [PubMed]
- Doniger SJ, Ishimine P, Fox JC, Kanegaye JT. Randomized controlled trial of ultrasound-guided peripheral intravenous catheter placement versus traditional techniques in difficult-access pediatric patients. Pediatr Emerg Care 2009;25:154-9. [PubMed] doi: 10.1097/PEC.0b013e31819a8946.
- Levin PD, Sheinin O, Gozal Y. Use of ultrasound guidance in the insertion of radial artery catheters. Crit Care Med 2003;31:481-4. [PubMed]
- Shiver S, Blaivas M, Lyon M. A prospective comparison of ultrasound-guided and blindly placed radial arterial catheters. Acad Emerg Med 2006;13:1275-9. [PubMed]
- Schwemmer U, Arzet HA, Trautner H, Rauch S,Roewer N, Greim CA. Ultrasound-guided arterial cannulation in infants improves success rate. Eur J Anaesthesiol 2006;23:476-80. [PubMed]
- Ishii S, Shime N, Shibasaki M, Sawa T. Ultrasound-guided radial artery cannulation in infants and small children. Pediatr Crit Care Med 2013;14:471-3. [PubMed] doi: 10.1097/PCC.0b013e31828a8657.
- Ganesh A, Kaye R, Cahill AM, Stern W,Pachikara R, Gallagher PR, et al. Evaluation of ultrasound-guided radial artery cannulation in children. Pediatr Crit Care Med 2009;10:45-8. [PubMed] doi: 10.1097/PCC.0b013e31819368ca.
- Khilnani PK. Learning curve for arterial cannulation using ultrasound: a myth or reality? Pediatr Crit Care Med 2013;14:545-6. [PubMed] doi: 10.1097/PCC.0b013e31828aa733.
- Varga EQ, Candiotti KA, Saltzman B, Gayer S, Giquel J, Castillo-Pedraza C, et al. Evaluation of distal radial artery cross-sectional internal diameter in pediatric patients using ultrasound. Paediatr Anaesth 2013;23:460-2. [PubMed] doi: 10.1111/pan.12151.







 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube