Subir Kumar Brahma, MD1, Maitreyee Mukherjee, MD2, Debalpana Chandra, MD3,
Dipasri Bhattacharya, MD4, Santi Bhattacharya5, Goutam Chowdhury, MD6
1Consultant Anesthesiologist; 2Assistant Professor; 4Professor and HoD; 6Professor
Department of Anesthesiology & Critical Care, R. G. Kar Medical College & Hospital, 1, Kshudiram Bose Sarani, Kolkata, West Bengal 700004 (India)
3Senior Resident, Department of Anesthesiology, ESI-PGIMSR & ESIC Medical College, Diamond Harbour Road, P.O. Joka, Kolkata, West Bengal 700104 (India)
5Professor, Department of Anesthesiology & Critical Care, IQ Narayana Multispeciality Hospital, Sovapur, Bijra Road, Jemua, Durgapur, West Bengal 713206 (India)
Correspondence: Dr. Maitreyee Mukherjee, 143/1 D, South Sinthi Road, Kolkata- West Bengal 700050 (India); Mobile: 09830415924; E-mail: dr_jhumpu@rediffmail.com
ABSTRACT
Background and Objectives: Large-volume administration of 0.9% saline are known to causes hyperchloremic metabolic acidosis (HMA) due to its high chloride load. Balanced or physiological fluids with inorganic ions are not associated with the same disturbance.
The purpose of this study was to see whether balanced crystalloid and colloid solutions cause less disturbances in postoperative acid base status than sodium chloride based solutions in patients undergoing elective open gastrointestinal surgery.
Methodology: Study subjects were patients aged between 30-60 years, ASA grades I and II, undergoing elective open gastrointestinal surgery, were selected as per proposed sampling design and were allotted into two groups, by the help of simple randomization process. Patients in the Group B received Hartmann’s solution and 6% hetastarch in balanced electrolyte and glucose solution and patients in the Group N received 0.9% sodium chloride solution and 6% hetastarch in 0.9% sodium chloride solution. Arterial blood samples were taken from both the groups of patients just prior to and 30 min after surgery. Baseline and final acid base status, heart rate, mean blood pressure, peripheral temperature, as well as urine output before, during and after surgery were recorded up to 48 hours. Prevalence of development of HMA was determined by appropriate statistical technique.
Results: The mean chloride level of normal saline group postoperatively was 118.66 ± 5.75 mmol/L (Normal range: 98-106 mmol/L) whereas in balanced saline group it was 103.27 ± 2.29 mmol/L, arterial pH was 7.31 ± 0.29 and 7.4 ± 0.02 respectively. Hence the changes in chloride level as well as arterial pH were significant in normal saline group versus balanced fluid group.
Conclusion: Normal saline based fluids cause significant alteration in arterial chloride and pH levels against the use of balanced fluids in gastrointestinal surgery.
Key words: Balanced crystalloid; Colloids; Hyperchloremic acidosis; Electrolytes; Gastrointestinal Surgery
Citation: Brahma SK, Mukherjee M, Chandra D, Bhattacharya D, Bhattacharya S, Chowdhury G. The effects of balanced versus saline based colloid and crystalloid solutions on acid-base and electrolyte balance in gastrointestinal surgery. Anaesth Pain & Intensive Care 2017;21(2):159-165
Received: 8 Sep 2016, Reviewed: 3 Feb 2017, Corrected: 7 May 2017, Accepted: 28 Jun 2017
INTRODUCTION
The aim of fluid therapy during intra-operative period is to replace loss and maintain fluid and electrolyte balance in the body, thus allowing normal cell and organ function.1,2 Crystalloid solution is most preferred fluid intra-operatively and it compensates third space and insensible losses during open surgical procedures. Sodium chloride 0.9% solution is often administered because it is isotonic with plasma and is initially distributed in the extracellular compartment.3
Colloid solutions maintain the circulating blood volume and stays in the intravascular compartment for longer duration. Large-volume administration of 0.9% saline is associated with the development of hyperchloremic metabolic acidosis due to the high chloride load. The intravenous (IV) administration of sodium chloride solution may also produce gastrointestinal (GI) dysfunction and postoperative nausea-vomiting along with hyperchloremic metabolic acidosis.4,5
Balanced or physiological fluids contain all the inorganic ions (calcium, potassium, or magnesium) or buffer components, such as bicarbonate or lactate, and have a smaller chloride concentration. These are not associated with the disturbance of acid-base physiology.3 When used in a plasma-adapted volume replacement strategy (balanced crystalloid plus balanced HES) it had better effects with regard to electrolyte concentration and base excess (BE) compared with a non-balanced solution ( normal saline and a non-balanced HES).6,7,8
The trial was designed to determine whether physiological or balanced crystalloid and colloid solutions can results in a superior metabolic environment and improved indices of organ perfusion in comparison to saline based fluids in 30-60 years old patients undergoing open elective GI surgery with ASA grade I and II.
We aimed to measure plasma chloride level before and after the surgery in patients belonging to both groups and assess the magnitude of hyperchloremic metabolic acidosis (HMA) by arterial blood gas analysis as the primary objective of the study. A secondary objective was to estimate postoperative health related events.
METHODOLOGY
Study was conducted in Surgical Operating Rooms and postoperative follow up was done at Post Operative Care Unit (POCU) and surgery ward from February 2013 to August 2014 on all patients undergoing open elective G.I. surgery under G.A. in Surgery OT during the period of data collection.
Patients of ASA status I and II, aged 30 years to 60 years were included in this prospective, randomized double blind comparative study. The patients and the data collector were unaware of the group allocation.
Patients with hypersensitivity to hydroxyethyl starch or with history of renal dysfunction were excluded from the study. Patients with pre-existing bleeding diathesis, pregnant and nursing females, ASA III and IV patients and patients with anticipated difficult airway were also excluded from the study.
Considering the proportion of patients developing the postoperative HMA as the outcome of interest, the sample size of the present study was calculated by the formula:
N (for one arm)=((Zα+Zβ)2.2 × P(100-P))/d2
Where Zα = 1.96 at 95% confidence limit (one tail);
Zβ = 0.84 at 80% power;
P=(p1+p2)/2 (where P = average prevalence, p1 = prevalence of HMA in control as taken and, p2 = prevalence of HMA in experimental group in the present study)
D = minimum reduction (that is called effect size) is required to achieve measureable clinical benefit.
P=(p1+p2)/2 =(67+10)/2 =38.5
((Zα+Zβ)2.2 × 38.5 × (100-P))/(30 × 30) = ((1.96+0.84)2.2 × 38.5 × 61.5)/900 = 37126.32/900 = 41.251
82 (41 study cases and 41 controls) patients were selected by systematic random sampling. Control group chosen after proper matching (to eliminate bias) received intravenous normal saline peri-operatively.
After approval from the institutional ethics committee this prospective, randomized, double blind controlled clinical trial was started. Study subjects were selected as per proposed sampling design and allotted in two groups by the help of simple randomization process.
All patients were premedicated with injection glycopyrrolate (.005 mg/kg), midazolam (.01-0.1 mg/kg), and ondansetron (0.1 mg/kg). Initially both study groups were given a 500 ml bolus of colloid (Group B balanced colloid and Group N saline based colloid) at their induction of general anesthesia. General anesthesia was induced with intravenous propofol (2-3 mg/kg), fentanyl (2µg/kg). Intravenous lignocaine (1.5 mg/kg) was used for laryngoscopic surge prevention. Atracurium (0.3-0.6 mg/kg) was used for endotracheal intubation. After tracheal intubation, anesthesia was maintained with isoflurane 0.5%, in an oxygen-nitrous oxide mixture of 1:2, and incremental doses of atracurium (0.1-0.2 mg/kg) as appropriate. Analgesia was provided with paracetamol and diclofenac slow IV infusion. Mechanical ventilation was performed. Intra-operative monitoring included end-tidal CO2, ECG, non-invasive blood pressure, pulse oximetry, nasopharyngeal temperature and urine output.
Composition of study fluids are as follows (Table 1):
Table 1: Composition of study fluids
| Variable | Balanced Fluid Group | Saline Group |
| Crystalloid | Plasma-Lyte
Sodium- 140 Potassium- 5 Chloride – 98 Calcium– 0 Magnesium – 1.5 Bicarbonate– 0 Lactate – 0 Acetate – 27 Gluconate – 23 Maleate – 0 |
0.9% NS
Sodium -154 mmol/L Chloride- 154 mmol/L |
| Colloid | Volulyte ( HES 6% ; 130/.40 )
Sodium- 137 Potassium- 4 Chloride – 110 Calcium – 0 Magnesium – 1.5 Bicarbonate – 0 Lactate – 0 Acetate – 34 Maleate – 0 Octanoate – 0 |
Voluven ( HES 6% ; 130/.40 )
Sodium- 154 Potassium- 0 Chloride – 154 Calcium – 0 Magnesium – 0 Bicarbonate – 0 Lactate – 0 Acetate – 0 Maleate – 0 Octanoate – 0 |
Initial fluid loading was followed by a crystalloid (Group B – balanced crystalloid and Group N – NS) infusion of 7 ml/kg/hour during surgery. Further IV fluids were given assessing the blood loss and hemodynamics of the patient. If patient was clinically underfilled (Mean BP < 20% of baseline or SBP < 90 mmHg or urine output < 0.5 ml/kg/hr) 250 ml of colloid infused over 10 min before considering inotrope support. Blood loss was assessed and replaced accordingly with crystalloid. Warm IV fluids were infused during the intra operative period. During the operative period, the patient’s temperature was kept nearly constant.
Arterial blood samples taken from both groups of patients just before and after surgery to determine baseline and final acid base status. Blood samples were also taken postoperatively to compare with pre-operative serum lactate level. HR, MBP, peripheral temperature, urine output were recorded before, during and after surgery upto 48 hours. Prevalence of development of HMA was determined by Graphpad.
Hyperchloremia is an electrolyte disturbance in which there is an abnormally elevated level of the chloride ion in the blood. The normal serum range for chloride is 97 to 107 mEq/L.
Acidosis is defined as arterial blood pH below 7.35
Metabolic acidosis – acidosis with a primary decrease in serum HCO3– (below 22 mEq/L).
RESULTS
41 patients had been randomly allocated to the balanced fluid group (Group B) and 41 to the Normal saline group (Group N). The groups were similar with regard to demographic patient characteristics and type and duration of surgical procedures. There were no significant differences in volumes of study fluids administered and postoperative hemodynamic indices. All 82 patients were analyzed. Descriptive statistics, such as the number of observations, mean, SD, and 95% confidence intervals, were calculated for quantitative variables, whereas qualitative variables were described with frequency tables. All statistical tests were two-sided and performed at 5% significance level. Postoperative chloride levels were analyzed with an analysis of covariance technique. For comparison of means or means of differences of secondary variables Student’s t-test was applied.
Table 2: Demographic patient characteristics, duration of operation
| Variable | Balanced Fluid Group
(n=41) |
Normal Saline Group
(n=41) |
Independent t | df | p value |
| Age (y) | 45.61 ± 7.27 | 44.46 ± 7.92 | 0.6849 | 80 | 0.4954 |
| Gender (male:female) | 26:15 | 27:14 | |||
| Body weight (kg) | 56.05 ± 5.91 | 56.73 ± 6.77 | 0.4865 | 80 | 0.6280 |
| Height (ft) | 5.454 ± .362 | 5.400 ± .39 | 0.6521 | 78 | 0.5163 |
| Duration of operation (min) | 160.32 ± 57.91 | 163.27 ± 59.85 | 0.2308 | 80 | 0.8181 |
Table 2 shows that the study subjects of both the groups were statistically similar in respect of their age, height and weight, duration of operation.
Figure 1: Time trend of mean heart rate of two groups during intra-operative period
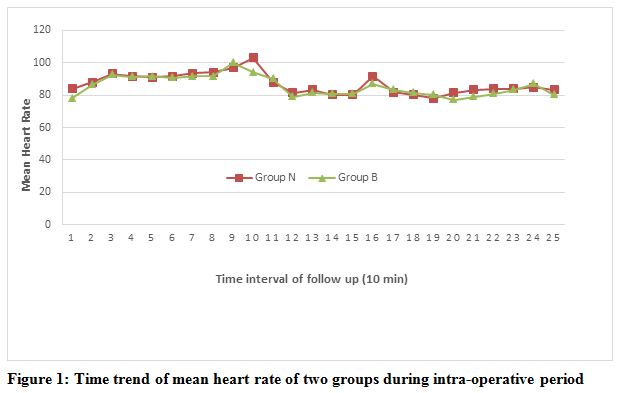
From figure 1 it is revealed that mean heart rate was comparable in the two groups.
Figure 2: Time trend of mean arterial blood pressure of two groups during intra-operative period
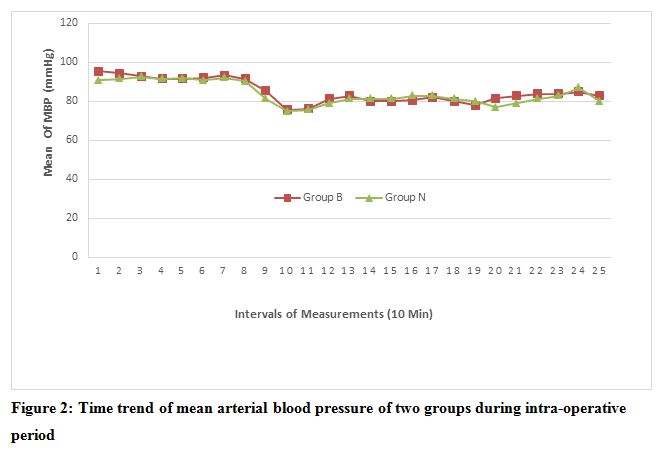
Average mean arterial blood pressure (MAP) of each phase of measurement of both the groups has been depicted in the Figure 2. Mean arterial BP was found to be comparable.
Table 3: Total volume of study fluid infused and total urine output
| Variable | Balanced Fluid Group
(n=41) |
Normal Saline Group (n=41) | Independent t | df | P value |
| Total volume of study fluid infused (ml) | 1895.12 ± 490.36 | 1802.93 ± 582.65 | 0.7820 | 80 | 0.4365 |
| Total urine output (ml) | 198.29 ± 78.82 | 190.49 ± 33.69 | 0.5827 | 80 | 0.5618 |
Total volume of fluid infused and urine output was comparable between two groups (Table 3).
Table 4: Pre- and postoperative acid-base indices
| Variable | Balanced Fluid Group | Normal Saline Group | p value |
| Preop bicarbonate (mmol/L) | 24.31 ± 1.26 | 23.78 ± 1.27 | < 0.0001 |
| Postop bicarbonate (mmol/L) | 24.42 ± 1.30 | 19.93 ± 1.54 | |
| Preop pH | 7.39 ± .026 | 7.38 ± .026 | 0.0001 |
| Postop pH | 7.40 ± .02 | 7.31 ± .029 | |
| Preop PCO2 | 40.50 ± 9 | 41 ± 9.75 | .05486 |
| Postop PCO2 | 37.50 ± 5.25 | 38.25 ± 6 |
Group normal saline has significant acidosis as well as decrease in bicarbonate level compared to other group (Table 4).
Table 5: Pre- and postoperative biochemistry measurements (mean ± SD)
| Variable | Balanced Fluid Group (mmol/L) | Normal Saline Group (mmol/L) | p value |
| Preop chloride | 103 ± 2.53 | 103.27 ± 2.29 | 0.0001 (significant) |
| Postop chloride | 107.54 ± 4.58 | 118.66 ± 5.75 | |
| Preop sodium | 139.44 ± 2.78 | 135.54 ± 3.41 | .6923 (not significant) |
| Postop sodium | 139.61 ± 3 | 141.39 ± 3.33 | |
| Preop potassium | 3.61 ± .19 | 3.50 ± .39 | 0.1376 (not significant) |
| Postop potassium | 3.58 ± .16 | 3.52 ± .2 | |
| Pre op lactate | 1 ± .7 | 1 ± .4 | .1161 (not significant) |
| Post op lactate | 1.2 ± .7 | 1 ± .4 | |
| Preop glucose | 5.4 ± 1.02 | 5.5 ± .87 |
0.6270 (not significant) |
| Postop glucose | 6.9 ± 1.7 | 6.7 ± 2.0 |
The mean increase in chloride level in the postoperative period was significantly higher in the normal saline group compared with the balanced fluid group (Table 5).
33 patients in the normal saline group (80.48%) but none in the balanced fluid group developed hyperchloremic metabolic acidosis. Demographical characteristics of these 33 patients were comparable with all other patients who participated in the study. Duration of surgery and type of surgery in this group were also comparable.
Twenty four patients (58.53%) in the saline group experienced postoperative nausea vomiting compared with eight patients (19.5%) in the balanced fluid group. Rescue antiemetic were offered to all patients who experienced PONV.
DISCUSSION
Hyperchloremic metabolic acidosis9 is a form of normal anion gap metabolic acidosis, with a decrease in plasma bicarbonate concentration, and an increase in plasma chloride concentration.
Three factors have increased recent interest in hyperchloremic acidosis: the observation that normal saline causes hyperchloremic acidosis; the renewed interest in the Stewart hypothesis; and the advent of new balanced solutions. Normal saline is neither normal nor physiological, a fact that has been acknowledged by physiologists for more than 100 years. Isolated tissues and cell cultures succumb rapidly in saline. Unprotected cells and even organs cannot function in that milieu.3,4,9
Saline induced hyperchloremic acidosis10,11,12 occurs due to dilution of bicarbonate ions by the isotonic fluids and production of excess protons by dissociation of water to maintain electro neutrality in presence of diluting fluid.
The main finding of this study was a mild metabolic acidosis (7.35 to 7.30) after a relatively brief interval (163.27 ± 59.85 min) of normal saline based IV fluid infusion, but not after balanced or physiological colloid and crystalloids infusion in patients undergoing open elective GI surgery aged 30-60 years with ASA grade I and II.
This acidosis with the saline based fluid infusion clearly had a metabolic origin, because PaCO2 was kept constant and there was no lactic acidosis. Hyperchloremia was identified as the main cause of this acidosis.
The pH values less than 7.35 do not seem to have major pathophysiologic implications in our clinical setting. This finding is quite similar to the studies conducted by Scheingraber S and Wilkes NJ.3,9
The patients receiving saline based fluid had significantly increased plasma chloride concentrations (mean 118.66 mmol/L, p-value .0001), decreased standard bicarbonate concentrations (mean 19.93 mmol/L) and increased base deficit at the end of surgery compared to those receiving balanced or physiological fluid.
The prescription of crystalloid therapy in medical and surgical care is so common that it is often viewed as routine. Despite the recognition nearly a century ago that infusion of 0.9% saline (often referred to as “normal saline”) and saline based IV fluid may cause predictable hyperchloremic metabolic acidosis, it remains one of the most commonly used intravenous solution.9
IV solutions with a balanced electrolyte formulation match the biochemical composition of human plasma more closely than sodium chloride-based solutions. Solutions containing physiologic levels of chloride and buffer—often called “balanced solutions”—are widely available, but they are used less frequently than 0.9% saline.7
One of the important finding of this study is that the infusion of normal saline based solutions for short duration in ASA I and II patients did not produce significant acid base and electrolyte abnormality. But it may occur in prolonged surgery with significant tissue handling. Acidosis in these cases was not due to hypoperfusion as serum lactate levels were normal in all cases. Studies done by various researchers support these findings.3-5
In our study no patient developed acidosis with pH below7.30.This can be explained by restrictive approach of fluid therapy. Though 0.9% NS produces hyperchloremic acidosis but it is the infusion of large volume (20-30 ml/kg/h) of NS which produces clinically significant acidosis. Scheingraber S, et al.9 in 1999 reported that infusion of 0.9% NS at the rate of 30 ml/kg/h during anesthesia and surgery definitely produce a clinically significant metabolic acidosis (pH < 7.3) with increased serum chloride.
The change in glucose was statistically not significant and was not clinically relevant in both of the groups of patients.
In our study although the incidence of PONV is much higher in patients receiving normal saline (supports the finding of Wilkes NJ3 on surgical patients), our data are inconsistent to explain the reasons why such associations occur as PONV is multifactorial.
LIMITATIONS
Short time interval. Surgical technique and the duration of surgery may differ among operating surgeons.
CONCLUSION
To conclude, this study has shown that the use of balanced solution avoids the development of hyperchloremic metabolic acidosis as compared to normal saline based crystalloid solutions in patients undergoing open elective gastrointestinal surgery under general anesthesia.
Acknowledgement: We are extremely thankful to Dr Ranabir Chanda, Assistant Professor for his constant support and help during the trial and Dr Sajib Chatterjee for correcting the manuscript.
Conflict of interest: nil
Author contribution: All authors equally contributed in conduct of study and manuscript preparation.
REFERENCES
- Kaye A, Riopelle J. Intravascular fluid and electrolyte physiology In: Miller R, ed. Miller’s Anesthesia, vol. 54, 7th Ed. Philadelphia: Churchill Livingstone, 2009; 1705–7.
- Doherty M, Buggy DJ. Intraoperative fluids: how much is too much? Br J Anaesth. 2012 Jul;109(1):69-79. doi: 10.1093/bja/aes171 [PubMed] [Free full text]
- Wilkes NJ, Woolf R, Mutch M, Mallett SV, Peachey T, Stephens R, et al. The effects of balanced versus saline-based hetastarch and crystalloid solutions on acid– base and electrolyte status and gastric mucosal perfusion in elderly surgical patients. Anesth Analg 2001;93:811–6. [PubMed]
- Mcfarlane C, Lee A. A comparison of Plasmalyte 148 and 0.9% saline for intra-operative fluid replacement. Anaesthesia. 1994 Sep;49(9):779-81. [PubMed] [Free full text]
- Prough OS, Bidani A. Hyperchloremic metabolic acidosis is a predictable consequence of intraoperative infusion of 0.9% saline. Anesthesiology. 1999 May;90(5):1247-9. [PubMed] [Free full text]
- Boldt J, Schollhorn T, Schulte G, Pabsdorf M. Volume replacement with a new balanced hydroxyethylstarch preparation (HES 130/0.42) in patients undergoing major abdominal surgery. Eur J Anaesth 2006;23:1–9. [PubMed]
- Grocott MP, Mythen MG, Gan TJ. Perioperative fluid management and clinical outcomes in adults. Anesth Analg. 2005 Apr;100(4):1093-106. [PubMed]
- Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einay S, Matot I. Effect of intraoperative fluid management on outcome after intra-abdominal surgery. Anesthesiology. 2005 Jul;103(1):25–32. [PubMed] [Free full text]
- Scheingraber S, Rehm M, Sehmisch C, Finsterer U. Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology. 1999 May;90(5):1265–70. [PubMed] [Free full text]
- Miller LR, Waters JH, Provost C. Mechanism of hyperchloremic metabolic acidosis. Anesthesiology. 1996 Feb;84(2):482-3. [PubMed] [Free full text]
- Mathes DD, Morell RC, Rohr MS. Dilutional acidosis: is it a real clinical entity? Anesthesiology. 1997 Feb;86(2):501-3. [PubMed] [Free full text]
- Russo MA. Dilutional acidosis: a nonentity? Anesthesiology. 1997 Oct;87(4):1010-1. [PubMed] [Free full text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube