Nazia Nazir, MD1, Shruti Jain, MD1, Mohit Mathur MD2, Suveer Sharma MD3
1Associate Professor, 3Professor; Department of Aaesthesiology,
2Assistant Professor, Department of Surgery,
School of Medical Sciences and Research, Sharda University, Greater Noida, U.P. (India)
Corresponding author: Dr. Nazia Nazir, Flat No: 502, Old Staff Quarter, Sharda University, Knowledge Park-III, Greater Noida, U.P. 201306 (India); Phone: +91-9560102957; E-mail: nazunazir@gmail.com
Keywords: Positive pressure; Congenital diaphragmatic hernia; Extubation
Citation: Nazir N, Jain S, Mathur M, Sharma S. Technique of extubation in congenital diaphragmatic hernia – an interesting case. Anaesth, Pain & Intensive Care 2017;21(1):117-118
In a mechanically ventilated patient, extubation may be done with a tracheal suction catheter technique (TSC) or after giving positive pressure breath (PPB).1 In TSC technique, endotracheal tube (ETT) is first suctioned and then ETT along with suction catheter is removed. While in PPB technique, ETT is removed after giving PPB with 100% oxygen with a rebreathing bag. We describe a pediatric patient with congenital diaphragmatic hernia (CDH) in which method of extubation made difference in outcome of the patient.
One day old infant weighing 2.4 kg presented in the emergency department of the hospital with complaints of increased crying and difficulty in feeding since birth. The mother had no antenatal checkups during her pregnancy and baby was delivered at term by cesarean section.
On examination, child was conscious, pink in colour with no peripheral cyanosis. Pulse rate was 140/min, respiratory rate 78/min, blood pressure (BP) was 62/40 mmHg and oxygen saturation (SpO2) was 94% on room air. There was absent air entry on the right base of lung, apex beat was shifted to mid axillary line and abdomen was scaphoid in shape. The chest x-ray showed subnormal lung expansion with herniated bowel and liver in right hemi-thorax. Diagnosis of right-sided CDH was made. Patient was shifted to Neonatal Intensive Care Unit where oxygen supplementation, maintenance fluid and dopamine infusion were started.
Next day infant was taken up for surgery, after premedication with fentanyl 5 µg and glycopyrrolate 0.02 mg IV, anesthesia was induced with sevoflurane in oxygen. Patient was intubated with 3.5 mm uncuffed ETT and maintained with atracurium (bolus dose of 1 mg IV and maintenance dose 0.01mg/kg IV), O2 and air in 1.5% sevoflurane with assisted ventilation using Jackson Rees circuit.
In the lateral position after a right sub–costal incision, right lobe of liver and transverse colon were identified, reduced and defect in right hemi-diaphragm closed with right thoracic cavity drained by a suction catheter used as chest tube. Controlled ventilation was continued in the post–operative period with pressure controlled synchronise intermittent mandatory ventilation (PC-SIMV) mode (Figure 1A).
Extubation was attempted on 5th day with TSC technique. But, infant became hypoxic, so was reintubated and ventilated with similar settings. X-ray showed a collapsed lung (Figure 1B) Extubation was tried again with PPB technique after 5 hrs of ventilation after confirming the well expanded lung. Subsequently, infant was able to maintain saturation with O2 supplementation. X-ray revealed a well expanded lung. (Figure 1C)
In TSC technique, though secretions from chest or pharynx are removed by suction, catheter may not be able to remove all secretions. Moreover, negative pressure generated by the suction catheter facilitates leakage of secretions into distal airway,2 favoring pulmonary aspiration and consequent atelectasis.3 In PPB technique, PPB of near total lung volume using a resuscitation bag fully expands the lung. ETT is then removed at the end of inspiration which causes the first post extubation respiratory event to be a cough which clears the airway of all secretions4 and prevents atelectasis of lung.
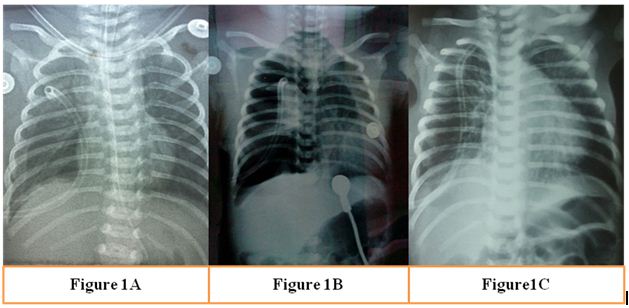
Figure 1A: Immediate post-operative chest x-ray; 1B: Extubation by trailing suction technique; 1C: Extubation by positive pressure breath technique
Studies have shown that outcome of patients is better with PPB extubation technique.5 But, TSC technique is more commonly practised by respiratory therapists, nurses and anesthetists.6 TSC technique of extubation may seem appropriate in routine cases but the importance of PPB is realised during extubation of atelectasis prone lung. Increased awareness as well as application of this manoeuvre may reduce peri-extubation problems in CDH patients.
REFERENCES:
- Suresh NS, Cheesman M. A survey of the current practice of tracheal extubation in intensive care units in England and Wales: trailing suction catheter technique vs. positive pressure breath technique. Anaesthesia 2006; 61:92-3.
- Hodd J, Doyle A, Carter J, Albarran J, Young P. Increasing positive end expiratory pressure at extubation reduces subglottic secretion aspiration in a bench-top model. Nurs Crit Care 2010; 15:257-61. [PubMed] doi: 10.1111/j.1478-5153.2010.00422.x
- Dave MH, Frotzler A, Madjpour C, Koepfer N, Weiss M. Massive aspiration past the tracheal tube cuff caused by closed suction system. J Intensive Care Med 2011; 26:326-9. [PubMed] [Free full text] doi: 10.1177/0885066610392516
- Andreu MF, Salvati IG, Donnianni MC, Iban˜ez B, Cotignola M, Bezzi M. Effect of Applying Positive Pressure With or Without Endotracheal Suctioning During Extubation: A Laboratory Study. Respiratory Care. 2014; 59:905-10. [PubMed][Free full text] doi: 10.4187/respcare.03121.
- Miller KA, Harkin CP, Bailey PL. Post operative tracheal extubation. Anesth Analg 1995; 80:149-72. [PubMed]
- Rassam S, Sandbythomas M, Vaughan RS, Hall JE. Airway management before, during and after extubation: a survey of practice in the United Kingdom and Ireland. Anaesthesia 2005; 60:995-1001. [PubMed][Free full text] DOI: 10.1111/j.1365-2044.2005.04235.x




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube