Basanth Kumar Rayani1, Harini Narayanan2, Mohammad Salman Saifuddin2, Abhijit S. Nair2
1Chief Anaesthesiologist; 2Consultant Anaesthesiologist,
Department of Anaesthesia and Pain Medicine, Basavatarakam Indo-American Cancer Hospital and Research centre, Hyderabad- 500034 (India)
Correspondence: Dr Abhijit S. Nair, Department of Anaesthesia and Pain Medicine, Basavatarakam Indo-American Cancer Hospital and Research centre , Hyderabad-500034 (India); Phone: +91-9963180495; E-mail: abhijitnair95@gmail.com
ABSTRACT
Rate induced left bundle branch block (LBBB) is a rare peri-operative phenomenon. We encountered rate related LBBB in a 72 year old patient who had undergone a craniotomy.
Acute coronary event was ruled out by doing serial troponin-I levels and absence of new onset regional wall motion abnormalities on echocardiogram. The electrocardiographic changes reverted to normal after controlling the rate with β blockers. Further cardiac evaluation was advised but the patient and family opted for a conservative medical management considering his age and co-morbidities.
Key words: Bundle-Branch Block, Coronary Artery Disease, Electrocardiography, Postoperative Period
Citation: Rayani BK, Narayanan H, Saifuddin MS, Nair AS. Postoperative rate induced left bundle branch block after craniotomy. Anaesth Pain & Intensive Care 2016;20(3):334-337
Received: 28 April 2016; Reviewed: 30 April & 23 August 2016; Accepted: 15 September 2016
INTRODUCTION
New onset left bundle branch block (LBBB) is an ominous electrocardiographic (ECG) change which warrants further evaluation. The reason could be acute coronary event, coronary vasospasm, underlying structural heart disease or idiopathic.
The management depends on the cause of LBBB. If LBBB develops postoperatively after a non-cardiac surgery, a cardiologist has to be involved early.
CASE REPORT
A 72 years old male weighing 68 kg, having a left parieto-occipital 4×3.4 cm lesion with moderate perifocal edema was posted for craniotomy and excision of tumour. He was a known hypertensive for last 10 years on tab amlodipine 5 mg once daily. He was diagnosed with type II diabetes mellitus with blood sugar under control with oral hypoglycemic agents. Other laboratory tests were unremarkable. 12 lead electrocardiogram was within normal limits (Figure 1).
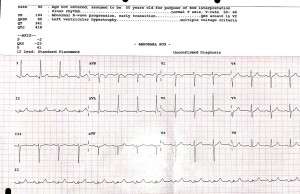
Figure 1: Preoperative 12 lead ECG – normal sinus rhythm. Left axis deviation and left ventricular hypertrophy by voltage criteria noted on ECG
His resting two dimensional echocardiogram (2D echo) revealed good LV/RV function with ejection fraction of 55%. Dobutamine stress echo (DSE) was done for risk stratification which was negative for inducible ischemia. The cardiologist cleared the patient for surgery under high risk in view of age,
comorbidities and major surgery. After obtaining a high risk consent for major surgery and after explaining possibilities of ventilatory support, major cardiovascular events, seizures and neural deficit; the patient was taken to operating room after confirming 6 hours of fasting. Anesthesia was induced with 2 mg midazolam, 100 µg fentanyl and 150 mg propofol. Airway was secured with 8 mm cuffed endotracheal tube after achieving neuromuscular blockade with 7 mg vecuronium. We monitored oxygen saturation with pulse oximeter, ECG with lead II, V5, V6; end tidal carbon dioxide; arterial BP with a left radial artery cannula. We cannulated the right subclavian vein with a 7 French double lumen central venous catheter to monitor central venous pressure and for possible vasopressor use. Surgery lasted for 4 hours during which a blood loss of 400 ml occurred. Postoperative medications were: mannitol 20 gm 8 hourly, phenytoin sodium 100 mg 8 hourly and dexamethasone 4 mg 8 hourly, along with inj ceftriaxone 2 gm twice daily and pantoprazole 40 mg once daily. After ventilating for 2 hours in surgical intensive care unit, an uneventful tracheal extubation was done.
There was no postoperative neural deficit on examination. 12 hours later, an abnormal rhythm with broad QRS complex was noted on cardioscope with heart rate of 140/min. 12 lead ECG was taken that revealed a new onset left bundle branch block not present in preoperative ECG (Figure 2)
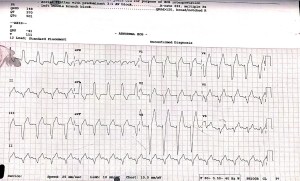
Figure 2: 12 lead ECG showing LBBB morphology
On enquiring the patient didn’t complain of chest pain or shortness of breath although he experienced palpitations. Cardiologist was asked to review, who did a screening 2D echo, which revealed LVEF of 54%, paradoxical septal motion, concentric left ventricular hypertrophy with no regional wall motion abnormality. Troponin I was ordered immediately and 6 hours later, which was found to be < 0.01 ng/ml on both occasions suggesting no acute coronary event. Cardiologist advised rate control with tab metoprolol 25 mg twice daily, aspirin 150 mg once daily, atorvastatin 40 mg
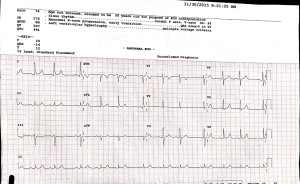
Figure 3: 12 lead ECG after starting metoprolol: normal sinus rhythm with no ST-T changes
once daily and inj enoxaparine 40 mg twice daily. After discussing with the surgeon, we decided to administer 40 mg enoxaparine subcutaneously only as acute coronary event was ruled out. The heart rate reduced from 140 to 84/min after metoprolol administration, which also reverted the LBBB morphology (Figure 3).
The ECG changes appeared again after 8 hours which reverted after another dose of tab metoprolol 25 mg. After this episode his heart rate was under control with no further episodes of palpitations till discharge.
DISCUSSION
Exercise induced LBBB is a rare event observed during 0.5-1 % of exercise stress tests. Rate induced LBBB are of two types. The first one is exercise induced which is called as acceleration induced LBBB which manifests when the heart rate increases to a particular number. The other one is deceleration induced where LBBB is seen when the heart rate drops to a particular number.1 The possible causes of such LBBB could be structural heart disease (cardiomyopathy, congenital heart disease, valvular heart disease), slow flow through coronaries, coronary vasospasm. The condition is possible even in presence of normal coronaries. However, another hypothesis is that the changes could be due to coronary microcirculation ischemia which cannot be detected n routine coronary angiography. Observational studies have shown greater possibilities of death and major cardiovascular events in patients developing LBBB during exercise or induced by rate. However, patients with normal coronaries presenting with exercise induced LBBB have shown to do well compared to patients having documented abnormality in the cardiovascular system.2
Further evaluation involves 2D echo, cardiac enzymes, coronary angiogram (CAG). 2D echo usually reveals paradoxical motion of interventricular septum. This paradoxical septal motion is responsible for the chest discomfort experienced by the patient. 3 The presence of regional wall motion abnormality can be seen on 2D echo. Troponins are useful in identifying an acute coronary event which warrants antiplatelets, statins and a CAG to quantify coronary artery disease. Definitive management can be planned if CAG is positive for coronary artery disease (CAD) i.e. revascularization, percutaneous or surgical. These patients can be absolutely asymptomatic during the rate related ECG change. However, a CAG might still be useful to rule out CAD, to access state of flow across the coronaries or to rule out coronary vasospasm also known as Prinzmetal’s angina.4
Management depends on the cause of LBBB. A proven CAD is managed by using β blockers, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, antiplatelets, statins and revascularization in indicated patients. In low flow states or in Prinzmetal’s angina, diltiazem is used. Anderson et al used non-pharmacological method to treat a patient with exercise induced LBBB having normal coronaries on CAG. They treated the rhythm abnormality with exercise training. The patient initially had chest discomfort with LBBB at a heart rate of 108/min, which with exercise training was later experienced at 150/min.5
Our patient had a DSE done preoperatively which was negative for inducible ischemia at a maximum heart rate of 150 /min. However, there was no LBBB noted at that time but was noted and documented in the postoperative period. We presume it could be due to surgical stress or coronary microcirculatory changes. The family didn’t evaluate the patient further owing to his age and associated co-morbidities and opted for conservative medical management.
Conflict of interest: Nil declared by the authors
Author contribution: BKR: Concept & design of manuscript; HN: Manuscript preparation; MSS: Manuscript preparation & bibliography; ASN: Manuscript preparation / review
REFERENCES
- Alhaji M. Intermittent left bundle branch block caused by coronary vasospasm. Avicenna J Med. 2013;3(2):50-52. doi: 10.4103/2231-0770.114129. [PubMed] [Free full text]
- Tanaka H, Hiraishi M, Miyoshi T, Tsuji T, Kaneko A, Ryo K, et al. Exercise-induced left bundle branch block and subsequent mechanical left ventricular dyssynchrony–resolved with pharmacological therapy. Cardiovasc Ultrasound. 2011;9:4. [PMC free article] [PubMed]
- Said SA, Bultje-Peters M, Nijhuis RL. Exercise-induced left bundle branch block: an infrequent phenomenon: Report of two cases.World J Cardiol. 2013 Sep;5(9):359-363. doi: 10.4330/wjc.v5.i9.359 [PubMed] [Free full text]
- Neiger JS, Trohman RG. Differential diagnosis of tachycardia with a typical left bundle branch block morphology.World J Cardiol. 2011 May 26;3(5):127-134. doi: 10.4330/wjc.v3.i5.127 [PubMed] [Free full text]
- Anderson NS, Ramirez A, Slim A, Malik J. Exercise Induced Left Bundle Branch Block Treated with Cardiac Rehabilitation: A Case Report and a Review of the Literature.Case Rep Vasc Med. 2014;2014:204805. [Free full text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube