Shiv Kumar Singh1, Ritesh Roy2, Gaurav Agarwal2, Chandrasekhar Pradhan2
1Consultant Anesthesiologist, Royal Liverpool University Hospitals, Prescot Street, Liverpool, UK L7 8XP.
2Consultant Anesthesiologist, CARE Hospitals, Bhubaneswar, Odisha, India.
Correspondence: Ritesh Roy, Consultant Anesthesiologist, Plot No. 582, Jagannath Complex, Flat No. 102, Sahid Nagar, Bhubnaeswar-751007, Odisha, (India); E-mail: drriteshroy@yahoo.com; Phone: 9437101886; Mobile: 91 9437101886
ABSTRACT
Adductor canal block (ACB) till now has been administered mostly by anesthesiologists who have access to ultrasound machines. It can be done blindly but the success rate is poor and variable. In this article, we describe peripheral nerve stimulation (PNS) guided ACB. Use of PNS will not only widen the acceptance of this block but also improve the success rate of analgesia for surgeries around the knee. We also describe the anatomical basis of this block and our experince with PNS guided ACB.
Key words: Adductor canal; Adductor canal block; Ultrasound; Peripheral nerve stimulation;
Citation: Singh SK, Roy R, Agarwal G, Pradhan C. Peripheral nerve stimulator (PNS) guided adductor canal block: A novel approach to regional analgesia technique. Anaesth Pain & Intensive Care 2017;21(3):340-343
Received – 4 May 2017; Reviewed – 17 May, 26 Jun, 5 Jul 2017; Corrected – 20 Jul 2017; Accepted – 5 Sep 2017
INTRODUCTION
Adductor canal block (ACB) has recently gained popularity in day case surgery and as part of enhanced recovery for procedures around the knee. This popularity is due to the fact that ACB does not produce motor blockade and hence allows for early ambulation and discharge from the hospital. Van der Wal and colleagues first described the approach to adductor canal way back in 1993; they described it as “subsartorial approach” to saphenous nerve.1 In 2009, Horn et al described the anatomical basis to the ultrasound-guided approach for saphenous nerve blockade2 and in the same year, Manickam et al described the feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal.3 Lund et al in 2011 described the use of continuous adductor canal block for post-op analgesia for knee surgeries.4
APPLIED ANATOMY OF THE ADDUCTOR CANAL
The adductor canal was first described by John Hunter in 1786. Adductor canal is a fibromuscular canal that contains the superficial femoral vessels and saphenous nerve along with a variable amount of fibrous tissue.5 This aponeurotic tunnel is located in the middle third of the thigh and runs from the apex of the femoral triangle (Scarpa’s triangle) to an opening in adductor magnus through which the femoral vessels reach the popliteal fossa. The adductor canal is conical or pyramidal in shape and triangular in cross-section. The boundaries are represented anterolaterally by vastus medialis (VM), posteriorly by adductor longus (AL) and adductor magnus (AM) muscles and anteromedially by a strong aponeurosis that extends between the adductors across the vessels to vastus medialis, the vasto-adductor membrane (VAM). The sartorius muscle along with its fascia lies anteriorly. The adductor canal contains branches from the femoral nerve, namely, Saphenous nerve (SN) (sensory), and the nerve to vastus medialis (NVM) (muscular branch). In the distal part of the canal, branches from the obturator nerve can also be found (Figure 1 and 2) The SN and NVM contribute to the innervations of the anteromedial knee joint and are the important targets of adductor canal block. It is these muscular branches in the distal part of the adductor canal that can be stimulated using PNS and local anesthetic (LA) can be deposited for peri-operative analgesia.6
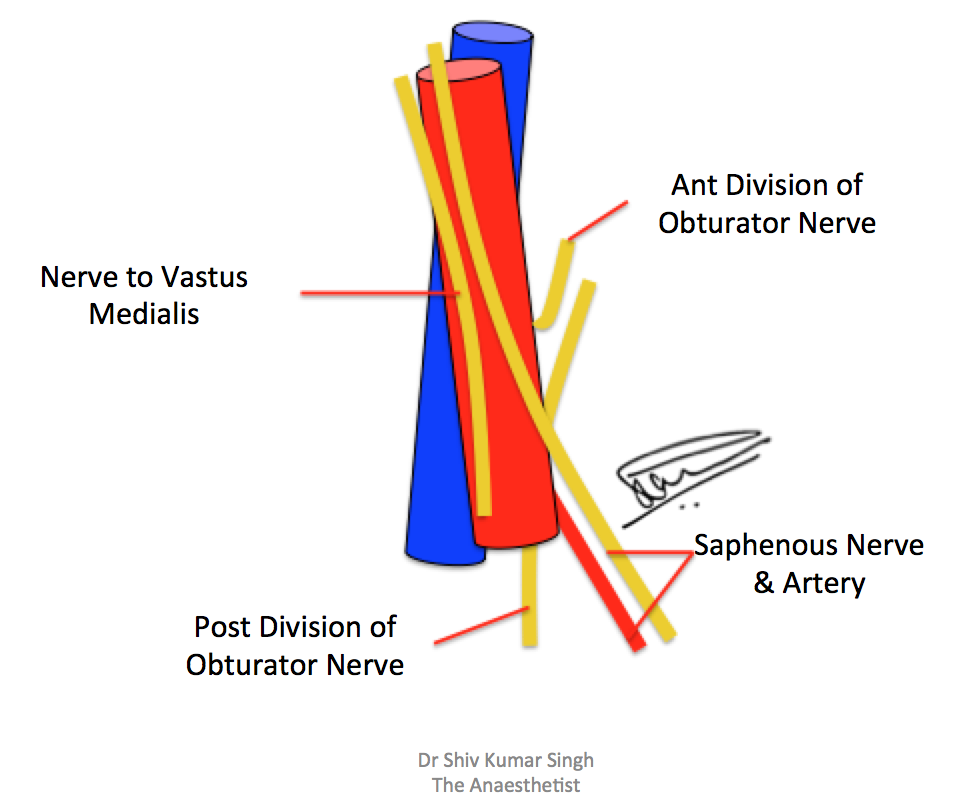
Figure 1: The contents of the adductor canal; the vessels and the nerves
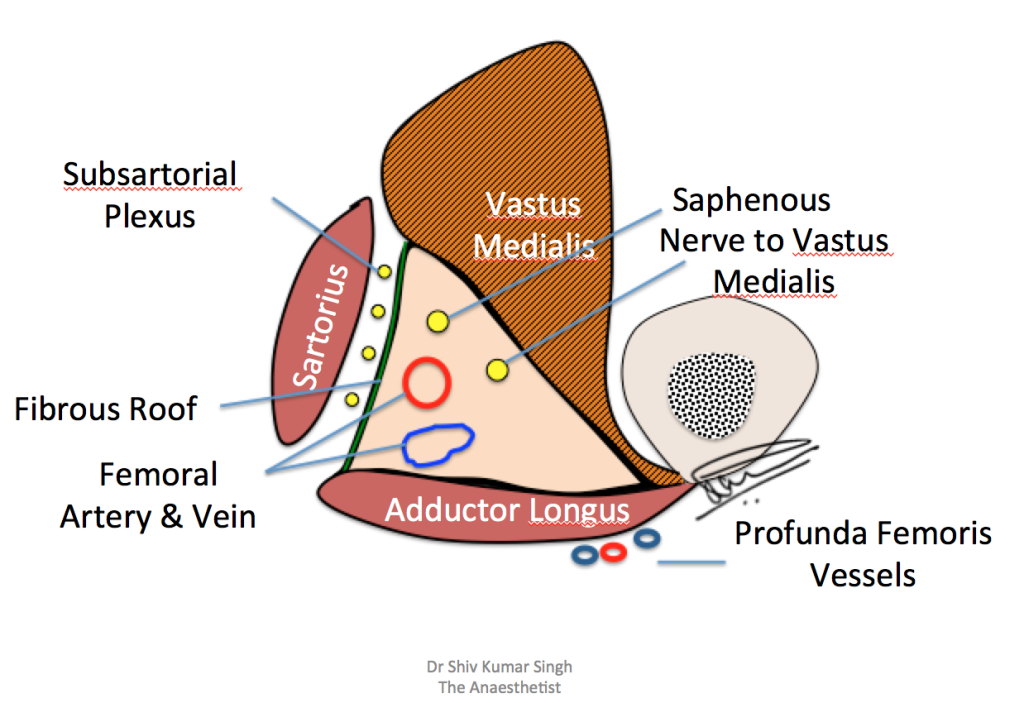
Figure 2: The boundaries of the adductor canal and the contents
It is a common misconception that the only nerve in the adductor canal is the saphenous nerve which is purely sensory. There is ample evidence from cadaveric studies that proves that vastus medialis is supplied by two branches, lateral and medial branches, both of which arise from the femoral nerve (Figure 3). The medial branch continues distally and divides into spray of branches. It has also been shown that the medial branch itself can arise separately from the femoral nerve and it then continues as the saphenous nerve.7 In few case reports, the medial branch has been observed to join the saphenous nerve and supply the distal part of the muscle.8
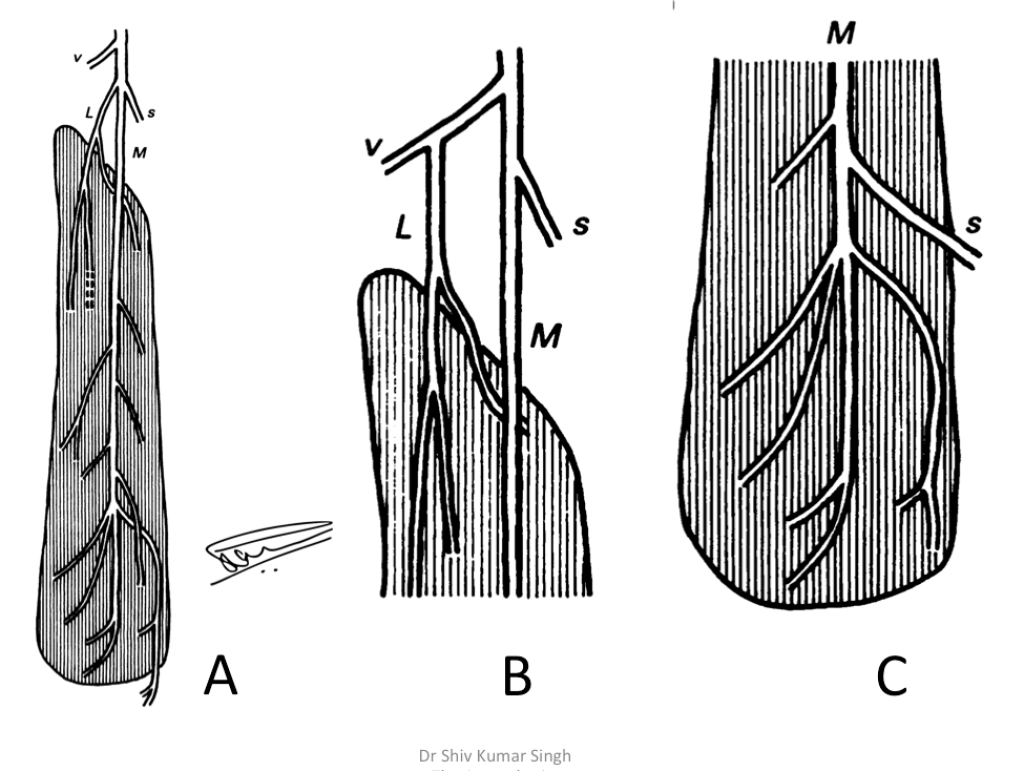
Figure 3: Schematic view of the nerve supply to the human vastus medialis (A). L,
lateral branch; M, medial branch; s, saphenous nerve; v, nerve to vastus intermedius. Interrupted line shows the terminal nerve that passes through the muscle to supply vastus intermedius. In B, variant in which the lateral branch arises from the nerve to vastus intermedius. In C, variant in which the main trunk continues as the saphenous nerve (Modified from reference 7)
ADDUCTOR CANAL BLOCK (ACB)
The ACB provides analgesia by blocking not only the saphenous nerve and nerve to vastus medialis but also the articular branches of obturator nerve. The femoral nerve block provides superior analgesia but is associated with increased number of falls due to quadriceps weakness.9 The advantage of ACB is largely the preservation of motor strength of the quadriceps muscles.10 In the meta-analysis conducted by Jiang et al, they have shown that ACB decreases the analgesic consumption in knee surgeries and was associated with early ambulation and retention of quadriceps strength.[11 In the current literature, ACB has been described using ultrasound (US) guidance. This introduces limitation for many anesthesiologists in the developing countries as the access to US is very limited. To reap the benefits of ACB and for wider acceptance of this block, a novel approach is described by the authors. This method utilizes PNS of the motor nerves that are found in the distal part of the adductor canal, namely the nerve to vastus medialis. Use of PNS for this block overcomes the limitation of US guided technique and makes it universally accessible.
DESCRIPTION OF THE PNS GUIDED ACB
The landmark for needle insertion is approximately 4 finger breadth (7 -8 cm) above the adductor tubercle on the medical condyle of the femur in the groove between sartorius and the vastus medialis muscle [Figure 4]. The groove is also known as the Jobert’s fossa.

Figure 4: The landmarks for the block
At the site chosen for needle insertion there is the saphenous nerve and the intramuscular and extramauscular branches of NVM which are stimulated by PNS. Blockade of these two nerves are important for analgesia of anteromedial aspect of knee.6,7
The fossa is in the popliteal region bounded above by the adductor magnus and below by the gracilis and sartorius; best seen when the knee is bent and the thigh strongly rotated outward. The procedure is done in operating room with all the safety procedures. IV access is secured and minimum standard monitoring applied. The patient lies supine with the leg slightly externally rotated.
Following aseptic procedure, a 5 cm 22G Stimuplex® (B Braun) needle is attached to the negative electrode of the PNS. The extension tubing is primed and attached to a syringe filled with LA solution. The initial current strength is set at 1 -1.5 mA. The block is best done by standing on the opposite side to the block site, for example for the right side block, it is better to stand on the left side of the patient. The left hand of the operator holds the sartorius and the gracalis muscles between the thumb and the middle finger such that the thumb lies in the Jobert’s fossa (Figure 5). The needle is inserted in the groove between the vastus medialis and sartorius and is directed perpendicular to the skin with slight posterior angulation till the contraction of vastus medialis muscle is elicited. The current is then reduced to 0.5 mA. The presence of vastus medialis contraction at 0.3 – 0.5 mA is considered as the end point and the LA solution is injected.
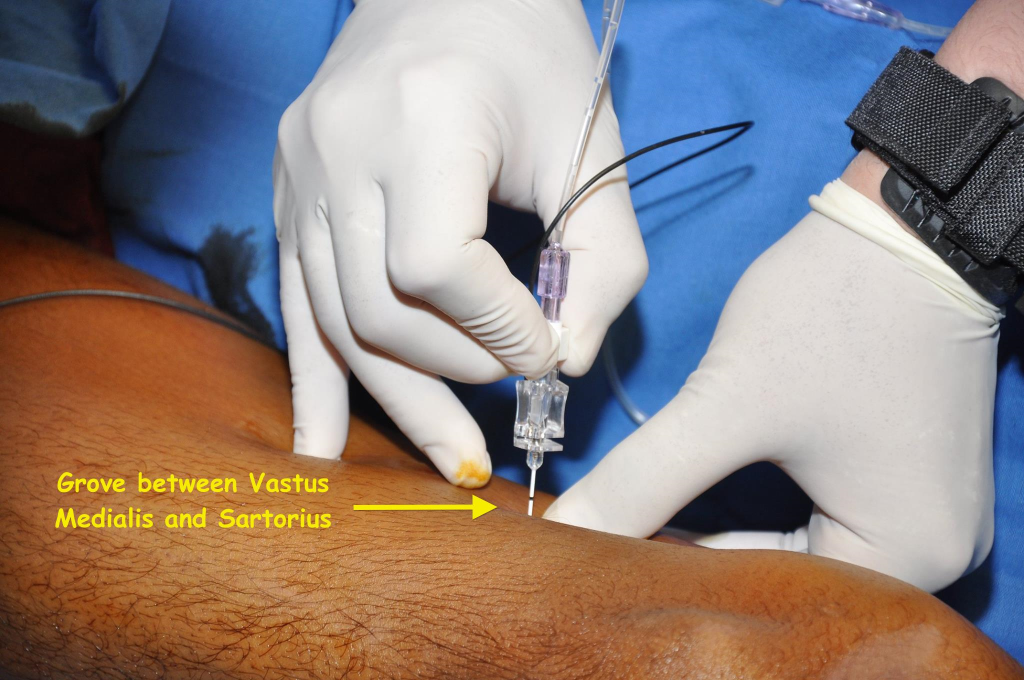
Figure 5: The left thumb in the Jobert’s fossa and the needle insertion in the grove between VM and sartorius
OUR EXPERIENCE
One of the author’s (SKS), who described the block way back in 2011, has demonstrated the PNS guided ACB at various live workshops in India. The technique is now being used by many anesthesiologists with good results.
Three of the authors (RR, GA and CP) have used the above technique in approximately 300 procedures around the knee, these include; ACL (ant cruciate ligament) repair, meniscectomies and total knee replacements (TKR). These cases were done over the last two years. We used 20 ml of ropivacaine 0.2% in these cases and observed excellent postoperative analgesia.
The technique, PNS guided ACB, described by us can be universally applied by those who do not have access to US machines specifically in the developing countries.
A randomized controlled trial (RCT) to test the efficacy and applicability of this block is underway by the authors (RR, GA and CP), whose results will be published on the completion of the study.
LIMITATIONS
Even though this is a safe block that can be done even by those who are new to regional anesthesia, there are concerns relating to intravascular injection of LA. This area does contain small vessels that can collapse due to the pressure applied and hence it is prudent to always aspirate before injection, aspirate after every 5ml injection of LA. It is also important that access to injectable lipid emulsion is easily available in case of LA toxicity. In approximately 300 cases done, we have not faced any such complications till date.
CONCLUSIONS
In this article, we describe a novel approach to the adductor canal that will allow wider acceptance of this technique for peri-operative analgesia. The relevant technical aspects of the PNS guided adductor canal block and applied anatomy has been described in this article. However, future large scale, randomized controlled trials are needed to confirm our findings.
Conflict of interest: None
Author contribution:
SKS: Concept and manuscript editing
RR: Concept and conduction of the study work, manuscript editing
GA + CS: Conduction of the study work and manuscript editing
REFERENCES
1. Van der Wal M, Lang SA, Yip RW. Trans-sartorial approach for saphenous nerve block. Can J Anaesth.1993;40(6):542-546. [PubMed]
2. Horn JL, Pitsch T, Salinas F, Benninger B.Anatomic basis to the ultrasound-guided approach for saphenous nerve blockade. Reg Anesth Pain Med. 2009 Sep-Oct;34(5):486-9. doi: 10.1097/AAP.0b013e3181ae11af. [PubMed]
3. Manickam B, Perlas A, Duggan E, Brull R, Chan VW, Ramlogan R. Feasibility and efficacy of ultrasound-guided block of the saphenous nerve in the adductor canal. Reg Anesth Pain Med. 2009;34(6):578-580. [PubMed]
4. Lund J, Jenstrup MT, Jaeger P, Sørensen AM, Dahl JB. Continuos adductor canal blockade for adjuvant postoperative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand. 2011 Jan;55(1):14-9. doi: 10.1111/j.1399-6576.2010.02333.x [PubMed]
5. de Souza RR, de Carvalho CA, König B Jr. Topographical anatomy of adductor canal: form, limits and constitution of its walls. Rev Paul Med. 1978 Jul-Aug;92(1-2):6-9.. [PubMed]
6. Burckett-St Laurant D, Peng P, Girón Arango L, Niazi AU, Chan VW, Agur A, et al. The nerves of the adductor canal and the innervations of the knee: An anatomic study. Reg Anesth Pain Med. 2016 May-Jun;41(3):321-7. doi: 10.1097/AAP.0000000000000389. [PubMed]
7. Thiranagama R. Nerve supply of human vastus medialis. J. Anat. (1990);170:193-198. [PubMed] [Free full text]
8. Verma R, Mishra S, Mahajan A. Variant branching pattern and supply of the posterior division of femoral nerve: report of a rare case. OA Anatomy 2013 Dec 01;1(4):32. [Free full text]
9. Sharma S, Iorio R, Specht LM, Davies-Lepie S, Healy WL. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res. 2010 Jan;468(1):135-40. doi: 10.1007/s11999-009-1025-1. [PubMed] [Free full text]
10. Kapoor R, Adhikary SD, Siefring C, McQuillan PM. The saphenous nerve and its relationship to the nerve to vastus medialis in and around the adductor canal: An anatomical study. Acta Anaesthesiol Scand. 2012 Mar;56(3):365-7. doi: 10.1111/j.1399-6576.2011.02645.x. [PubMed]
11. Jiang X, Wang Q, Wu C, et al. Analgesic efficacy of adductor canal block in Total knee arthroplasty: A meta-analysis and systematic Review. Orthopedic Surgery. 2016; 8:294-300. [PubMed] [Free full text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube