R. V. Ranjan, DA, DNB*, Manikandan Sivasubramanian, MD**, T. R. Ramachandran, MD***, Baranidharan Selvamani, MBBS****
*Associate Professor; **Assistant professor, ***Professor, ****Resident PG
Department of Anesthesiology, Pondicherry Institute of Medical Sciences, Puducherry-605014 (India)
Correspondence: Dr R. V. Ranjan, House No. 11, Type D-II quarters, JIPMER campus, Puducherry-605006, (India); Phone: 09600823772, 0413 2271243; E-mail: ranjanrv2005@gmail.com
ABSTRACT
The anesthetic management of a patient with severe left ventricular dysfunction undergoing non cardiac surgery is a challenging task, as left ventricular systolic dysfunction (LVSD) is commonly complicated by progressive congestive heart failure and malignant arrhythmias. When the cause for LVSD is post valve replacement, additional complications like intraoperative thrombosis, bleeding and infective endocarditis need to be addressed peri-operatively. In such situations, the anesthesiologist must have the knowledge of hemodynamic changes, diagnostic and treatment modalities, as well as various drugs used during anesthesia. We report a case of post mitral valve replaced patient with severe LVSD posted for surgery of fracture of femur and facial fractures managed successfully during anesthesia.
Key words: LV dysfunction; post mitral valve replacement; anticoagulation
Citation:Ranjan RV, Sivasubramanian M, Ramachandran TR, Selvamani B. Perioperative management of polytrauma in a post MVR patient with severe left ventricular systolic dysfunction. Anaesth Pain & Intensive Care 2014;18(4):455-57
INTRODUCTION
Perioperative management of patients with severe left ventricular systolic dysfunction (LVSD) can pose a great challenge. Various etiological factors have been implicated in this condition, most common of these being ischemic heart disease, dilated cardiomyopathy and idiopathic cardiomyopathy. A large amount of literature exists about perioperative management of LVSD in these conditions.(1) LVSD due to valvular heart disease is not as common. The important but difficult goal in these patients is to maintain sinus rhythm and prevent myocardial depression (2) despite pre-existing atrial fibrillation and anti-coagulation therapy due to valvular heart disease. Here we report successful management of a case of post mitral valve replacement (MVR) patient with severe LVSD (ejection fraction = 20%) who reported for femur shaft nailing and open reduction and internal fixation (ORIF) of facial fractures.
CASE REPORT
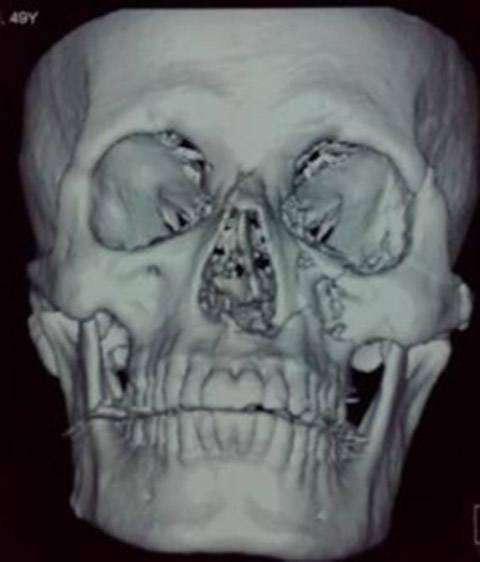
A 50-year-old male was admitted with history of road traffic accident. He was a known case of rheumatic heart disease (RHD) since the age of 30 years and had undergone a successful mitral valve replacement surgery 11 years back. He had sustained fracture of the shaft of right femur and left zygoma, floor of the orbit and left maxilla (Fig 1). He was scheduled for intramedullary nailing of right femur with ORIF of facial fractures. He had no other co-morbidity. His past history revealed that prior to the valve replacement; he was in NYHA class IV breathlessness which improved to class III after valve replacement. Prior to the trauma, his effort tolerance was poor; he was only able to walk 300-500 meters on level ground before developing symptoms of palpitations, fatigue, chest pain or breathlessness. He was receiving oral warfarin 3 mg, digoxin 0.25 mg and enalapril 2.5 mg once daily.
Fig 1: 3D reconstruction of skull showing facial fracture
Fig 2: Chest x-ray PA view showing cardiomegaly, sternotomy sutures
Physical examination revealed an irregularly irregular pulse, 90 beats/min and blood pressure of 120/70 mmHg. His JVP was raised and rest of the systemic examination did not reveal any abnormality. Patient’s ECG showed atrial fibrillation with a heart rate of 100/min. Chest x-ray revealed cardiomegaly, mitral valve prosthesis, and sternotomy sutures (Fig 2). His echocardiogram showed poor biventricular function (EF 20%, global hypokinesia), PA pressure of 75 mmHg, mild tricuspid regurgitation, no paravalvular leak and absence of vegetations and no LA clots. Renal and liver functions were within normal limits. Warfarin was stopped and he was put on low molecular weight heparin (LMWH) 0.6 ml twice a day. On the fourth day his INR was stabilized at 1.2, and he was scheduled for surgery. On the day of the surgery, morning dose of LMWF was skipped and he was shifted to operating rooms. Two units of packed red blood cells, fresh frozen plasma, platelets and protamine were reserved for emergency use in case of undue blood loss during the surgery. Patient received ampicillin 1.5 g and gentamicin 80 mg IV as infective endocarditis prophylaxis 30 min prior to skin incision. Apart from the standard monitoring, invasive blood pressure monitoring and central venous pressure monitoring were also instituted. In view of the surgery involving orofacial tissues, trans-oesophageal echocardiography (TEE) monitoring was not used. Injection Dobutamine 5 µg/kg/min and inj. noradrenaline 0.05 µg/kg/min were started before inducing the patient. Patient was then induced with midazolam 2 mg, fentanyl 250 µg, thiopentone sodium 100 mg and vecuronium 8 mg. Nasotracheal intubation with 7.5 mm Portex® endotracheal tube was done. Anesthesia was maintained with the help of 50% oxygen in air, sevoflurane (1-2%) and intermittent boluses of vecuronium 1 mg and 25 µg of Fentanyl. The operative blood loss was 500 ml which was replaced with one unit of packed red blood cells and crystalloids. Total duration of the surgery was 7 hours and hemodynamics were well maintained throughout the procedure. At the end of the procedure patient was shifted to PACU and ventilated for two hours. Once his core body temperature returned to normal and ABGs showed acceptable PaO2 and PaCO2, neuromuscular block was reversed with neostigmine and glycopyrrolate and he was extubated. He was restarted on LMWH 0.6 mg in the evening, and the next morning, warfarin was also started. By 4th day the INR was 2.2, LMWH was stopped and warfarin continued. An echocardiogram done at the time of discharge revealed normally functioning valves with no clot or vegetation. He was discharged from the hospital after two weeks.
DISCUSSION
Our present case had three major problems; severe biventricular systolic dysfunction (EF 20%), prosthetic mitral valve and prolonged surgical procedure (7 hrs) with associated hemodynamic and intravascular volume changes. The goals for anesthetic management were prevention of thrombosis, prevention of infective endocarditis, adequate analgesia, avoidance of drug induced myocardial depression, maintenance of normovolemia and prevention of increased ventricular afterload.3
In surgical patients with prosthetic heart valve, a risk of thrombosis has to be balanced against the risk of hemorrhage. There are no large randomized studies that compare different perioperative anticoagulant regimens for patients with mechanical heart valves undergoing surgery. Because of the high risk of hemorrhage, the INR should be within the normal range before the procedure which can be accomplished by stopping warfarin. To minimize the risk of thrombosis in patients with prosthetic heart valves, both the European Society of Cardiology and the ‘Fourth American College of Chest Physicians Consensus on Antithrombotic Therapy’ have recommended perioperative heparinization.4
Perioperative management
In case of elective surgery, it is essential to have adequate medical control of heart failure for at least a duration of one week. But in emergency/semi-emergency cases there would be no time to optimize the heart failure. In such cases, any arrhythmia should be appropriately treated. If the patient is already in atrial fibrillation (AF), rate control is very important and this is achieved with drugs and by correcting the electrolyte imbalance; hypokalemia and hypomagnesemia are corrected.5 The degree of biventricular impairment and valvular dysfunction is assessed by echocardiography. Whenever feasible and possible, consideration should be given to the use of regional or local anesthesia. Regional anesthesia used alone or in combination with general anesthesia has the advantage of reducing the afterload which can improve cardiac output.6 However, hypotension must be prevented to avoid myocardial hypoperfusion. Treatment of arterial pressure changes should be considered if >10% decrease in systolic pressures occurs. Vasodilators and/or vasopressors are to be used to maintain hemodynamic stability.
Invasive hemodynamic monitoring using direct arterial pressure and central venous pressure is indicated in unstable patients, prolonged surgical procedure, especially in emergency situation. Intraoperative TEE is recommended to evaluate dynamic changes in cardiac performance and the response to inotropes and fluid loading. In our case, it could not be used in view of maxillofacial surgery. During anesthesia, avoidance of tachycardia is an additional goal. Inotropic support if required during and after surgery can be provided by the use of a variety of agents including dobutamine, dopamine, phosphodiesterase inhibitors, and levosimendin. It may be necessary to counteract some of the peripheral vasodilator effects of general anesthetic agents to assist coronary perfusion. This is achieved with the cautious use of norepinephrine which increases systemic vascular resistance and maintains mean arterial pressure.3 Hence small doses of dobutamine and noradrenaline were used in this case to improve biventricular function and to prevent further increase in pulmonary pressure and support the circulation, in view of the compromised cardiac status of this patient.
Extubation should be as smooth as intubation. It should be attempted only when the patient is hemodynamically stable, the core body temperature has returned to normal and electrolytes and ABG are within normal limits.
To conclude, the main purpose of presenting this case is to emphasize the need for special attention towards maintaining stable rhythm and anticoagulation in patients with LVSD due to valvular heart disease. This is in addition to other factors like a thorough preoperative assessment, optimizing the cardiac status, proper anesthetic plan, intraoperative and postoperative monitoring and prompt recognition and management of complications.
REFERENCES
- Davies MR, Cousins J. Cardiomyopathy and anaesthesia, continuing Education in Anaesthesia, Critical Care & Pain 2009; 9:189-193.
- Groban L, Butterworth J. Peri-operative management of chronic heart failure. Anaesth Analg. 2006 Sep; 103(3):557-75.[PubMed][Free Full Text]
- Prashan HT, Thiagarajah S, Elizabeth AMF. Anaesthetic considerations in patients with cardiomyopathies. MEJ Anaesth 2009 Oct; 20 (3): 347-54. [PubMed]
- Lee AF, Joshua AB, Kenneth AB, Hugh C, Elliot LC, Kirsten EF et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Non-cardiac Surgery: Executive Summary. Circulation 2007; 116:1971-1996 [Free Full Text]
- Ceremuzynski L, Gebalska J, Wolk R, Makowska E. Hypomagnesemia in heart failure with ventricular arrhythmias. Beneficial effects of magnesium supplementation. Journal of Internal Medicine 2000; 247(1):78-86. [PubMed][Free Full Text]
- El-Dawlatly A, Al-Dohayan A, Fadin A. Epidural anaesthesia for laparoscopic cholecystectomy in a patient with dilated cardiomyopathy: Case Report and Review of Literature. Internet Journal of Anaesthesiology 2007;13(1).[Free Full Text]





 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube