Rajdip Hazra*, Manjunatha S. M.*, M. D. Babrak Manuar*,
Rajarshi Basu**, Sisir Chakraborty***
*Department of Anesthesiology, Nilratan Sircar Medical College and Hospital, Kolkata (India)
**Department of Pediatric Medicine, Nilratan Sircar Medical College and Hospital, Kolkata (India)
***Department of Medicine, College of Medicine and Sagore Dutta Hospital, Kolkata (India)
Correspondence: Dr. Rajdip Hazra, Room No. 15, Doctors Hostel, 35 Dixon Lane (Near Prachi Cinema,Opposite NRS Hospital), Kolkata-700014, West Bengal (India); E-mail: Phone: +91 80 13436607
ABSTRACT
Background: Clonidine, a selective alpha-2 adrenergic agonist, and dexmedetomidine, a new generation highly selective alpha-2 adrenoreceptor agonist, are well known to inhibit catecholamine release. The present study compares the effects of intravenously administered clonidine versus dexmedetomidine to attenuate hemodynamic responses to pneumoperitoneum during laparoscopic cholecystectomy under general anesthesia.
Methodology: 60 patients of ASA physical status I and II, aged between 18 to 50 years, of either sex. scheduled for elective laparoscopic cholecystectomy were randomized into 3 groups (Group C, D and K) in a double-blind fashion, to receive either clonidine 1 µg/kg in normal saline, dexmedetomidine 1 µg/kg in normal saline or normal saline IV respectively. Total volume of the study drug was adjusted to 50 ml and administered over a period of 15 minutes before induction.
Result: Following pneumoperitoneum, significant rise in heart rate and arterial pressure was observed in group K. Patients in group D showed best control of arterial pressure. No significant episodes of hypotension were found in any group.
Conclusion: Administration of clonidine or dexmedetomidine attenuates hemodynamic response to pneumoperitoneum, dexmedetomidine being more effective in this regard.
Keywords: Clonidine; Dexmedetomidine; Laparoscopic cholecystectomy; Hemodynamic response; Pneumoperitoneum
Citation: Hazra R, Manjunatha SM, Manuar MDB, Basu R, Chakraborty S. Comparison of the effects of intravenously administered dexmedetomidine with clonidine on hemodynamic responses during laparoscopic cholecystectomy. Anaesth Pain & Intensive Care 2014;18(1):25-30
INTRODUCTION
Laparoscopy has now become the standard technique of choice for cholecystectomy. The hallmark of laparoscopy is the creation of pneumoperitoneum with carbon dioxide (CO2). The pneumoperitoneum results in pathophysiological changes characterized by increase in arterial pressure and systemic and pulmonary vascular resistance (SVR and PVR) early after the beginning of intra-abdominal insufflation with little change in heart rate (HR).1-3 A 10% to 30% reduction in cardiac output has been reported in most studies.1-3 Severe increases in arterial pressure can be a risk factor for adverse cardiologic events in patients with pre-existing essential hypertension, ischemic cardiac disease, or increased intra-cranial or intra-ocular pressure.4
Problems encountered during laparoscopic surgeries may result from the combined effects of pneumoperitoneum and patient positioning.5 Hypercapnia and pneumoperitoneum cause stimulation of the sympathetic nervous system causing catecholamine and vasopressin release.6 Different pharmacological agents like α2 adrenergic agonists1, beta-blockers7 and opioids8 are often used to attenuate circulatory response due to pneumoperitoneum.
Clonidine is a selective α2 adrenergic agonist that causes a fall in the heart rate and blood pressure with decreased systemic vascular resistance and cardiac output.9 Dexmedetomidine is a highly selective, potent and specific α2 agonist with a shorter duration of action.10
The present study was designed in a prospective, randomized, double-blind fashion to compare the efficacy of intravenously administered clonidine versus dexmedetomidine in attenuation of hemodynamic responses during laparoscopic cholecystectomy. The secondary objective was to study the side effects associated with these drugs.
METHODOLOGY
After getting approval from the institutional ethical committee and written informed consent from patients, this study was conducted in a tertiary care medical college hospital in eastern India. 60 ASA physical status I and II patients aged between 18 to 50 years of both sexes scheduled for elective laparoscopic cholecystectomy were enrolled in the study. Power calculations suggested that a minimum of 16 subjects per group was required to detect 10% difference in arterial pressure between groups (taking type I or α error of 5%, type II or β error of 20% and Standard Deviation=10). To be on a safer side, 20 patients were included in each group (n=20).
Patients with any degree of heart block, pre-existing hypertension, cardiovascular, hepatic or renal disease, allergies to the drugs used, or acute cholecystitis as well as pregnant ladies and lactating mothers were excluded from the study. Patients concomitantly taking clonidine, methyl-dopa, beta blocking drugs, benzodiazepines, MAO inhibitors, patients in whom surgery could not be completed laparoscopically and open cholecystectomy had to be performed were also excluded from the study. Patients who showed exaggerated hypertensive responses (taken as systolic BP > 160 mmHg or diastolic BP > 100 mmHg) during surgery were administered nitroglycerine infusion.
Patients were admitted one day prior to the scheduled surgery and examined, interviewed and written consent taken. No hypnotic medication was given on the evening before surgery. Patients were premedicated with glycopyrrolate 0.02 mg/kg in the preoperative room. Upon arrival in the operating room, monitors were attached and baseline parameters, e.g. heart rate, NIBP, oxygen saturation and ECG, were recorded.
Immediately before induction, patients were randomly divided into three equal groups (n=20) using sealed envelopes chosen by the patients. The groups were;
- Control group (group K) – received 50 ml of normal saline.
- Clonidine group (group C) – received clonidine 1 µg/kg in normal saline.
- Dexmedetomidine group (group D) – received dexmedetomidine 1 µg/kg in normal saline.
Total volume of the study drug was adjusted to 50 ml and administered over a period of 15 min before induction. The preparation, labeling and administration of the study drugs was performed by an anesthesiologist who was not directly involved in this study.
After pre-oxygenation for 3 minutes, anesthesia was induced with a standard anesthetic protocol using midazolam 0.05 mg/kg, fentanyl 1 µg/kg, thiopentone sodium 3-5 mg/kg, and tracheal intubation was facilitated by vecuronium bromide 0.1 mg/kg intravenously. Anesthesia was maintained by N2O:O2 (60:40) with controlled ventilation. After 1 hour of surgery, each patient received 1 gm paracetamol infused over 30 minutes intravenously. Throughout the laparoscopic surgery, carbon dioxide pneumoperitoneum was established and maintained to a pressure of 14 mm Hg and ETCO2 was maintained between 25-45 mm Hg. The surgical techniques were identical in all the three groups. During surgery, Ringer’s lactate solution was administered in maintenance dose as per Holiday Segar formula.
At the end of operation, neuromuscular blockade was antagonized with injection of neostigmine 0.05 mg/kg and glycopyrrolate 0.02 mg/kg intravenously and patient was extubated when respiration was deemed sufficient and they were able to obey commands.
Arterial pressures and heart rates were measured upon arrival in the OT (baseline), before induction, 3 minutes after endotracheal intubation, before pneumoperitonium (P0); at 10 (P10), 20 (P20) and 30 (P30) minutes after pneumoperitoneum and then every 20 minutes till the end of surgery, ten minutes after release of CO2 and ten minutes after extubation. The anesthesiologist who measured the arterial pressures and heart rates was unaware of the study.
STATSTICAL ANALYSIS
Data was expressed as mean and standard deviation. The homogeneity in 3 groups of mean and SD was analyzed using SPSS version 16.0 software. Comparisons amongst the same group were done using Student- T test while inter-group comparisons were done using one way analysis of variance (ANOVA). Categorical data were compared using Chi-square test. A p value of less than or equal to 0.05 was considered as statistically ‘significant’.
RESULTS
There were no significant differences between the three groups with regard to demographic data such as age, sex, weight, ASA grade and duration of surgery (Table 1). Preoperative vital parameters were compared among the three groups of patients and no significant difference was found (Base line values of table 2, 3, 4 and 5). Mean intra-abdominal pressure was maintained to 14 mm Hg throughout the laparoscopic surgery. No patient was excluded from study. However, 4 out of 20 patients (20%) in group K required intra-operative NTG drip for control of hypertension. It was not required in group C or D patients, because they remained hemodynamically stable.
Table 1. Demographic profile (Mean ± SD)
| Demographic profile | Group C | Group D | Group K | P value | Significance |
| Age (years) | 37.7±9.59 | 37.3±9.41 | 35.4±10.34 | 0.7309 | NS |
| Sex (F : M) | 18 : 2 | 18 : 2 | 17 : 3 | 0.8505 | NS |
| Weight (Kg) | 60.65±6.21 | 61.05±6.86 | 60.15±7.97 | 0.92157 | NS |
| ASA Grade (I : II) | 16 : 4 | 15 : 5 | 16 : 4 | 0.90616 | NS |
| Duration of surgery (min) | 47.95±9.20 | 45.70±12.59 | 48.50±10.74 | 0.69354 | NS |
NS = Not significant
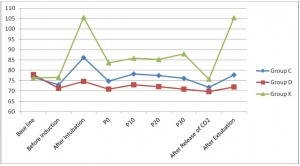
Upon statistical comparison of heart rate in three groups of patients, significant variation was observed throughout the intraoperative period except for the baseline and before induction values where no significant difference was observed (Figure 1, table 2). In group K, heart rate was significantly higher after intubation and after extubation (105.55±10.20 and 105.45±8.99 respectively). Mean heart rate was lowest for group D. 3 out of 20 patients (15%) in group D required intravenous atropine due to bradycardia.
Figure 1. Changes in heart rate in three groups
Table 2. Changes in heart rate in three groups (Mean ± SD)
| Heart Rate (bpm) | Group C | Group D | Group K | P value | Significance |
| Base line | 76.60±6.76 | 77.85±6.84 | 76.30±7.75 | 0.76746 | NS |
| Before Induction | 72.95±6.68 | 71.40±6.71 | 76.55±8.05 | 0.07499 | NS |
| After Intubation | 86.10±7.21 | 74.65±7.03 | 105.55±10.20 | <0.00001 | HS |
| P 0 | 74.80±10.25 | 70.95±8.51 | 83.60±11.03 | 0.00062 | HS |
| P 10 | 78.15±11.01 | 73±9.24 | 85.80±9.62 | 0.00068 | HS |
| P 20 | 77.40±6.08 | 72.05±10.67 | 85.20±6.97 | 0.00002 | HS |
| P 30 | 76.10±5.66 | 70.83±8.42 | 87.95±6.07 | <0.00001 | HS |
| After Release of CO2 | 71.75±5.70 | 69.70±5.14 | 75.60±5.62 | 0.00452 | HS |
| After Extubation | 77.75±8.03 | 71.95±8.68 | 105.45±8.99 | <0.00001 | HS |
P0, P10, P20, P30 = before & 10, 20, 30 minutes after pneumoperitoneum, respectively;
NS = Not significant, HS = Highly significant
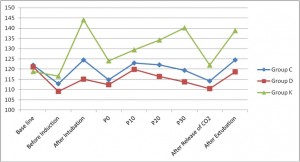
Systolic arterial pressure was significantly higher in group K (specially after intubation, at P30 and after extubation) except the baseline value (Figure 2, table 3). No significant episode of hypotension was found in any of the groups post pneumoperitoneum.
Figure 2. Changes in systolic arterial pressure in three groups
Table 3. Changes in systolic arterial pressure in three groups (Mean ± SD)
| SAP (mm Hg) | Group C | Group D | Group K | P value | Significance |
| Base line | 121.95±7.75 | 121.05±8.12 | 118.80±8.82 | 0.46557 | NS |
| Before Induction | 112.80±6.49 | 109.15±6.89 | 116.50±8.62 | 0.01048 | S |
| After Intubation | 124.50±9.36 | 115.10±6.20 | 144.05±7.13 | <0.00001 | HS |
| P 0 | 114.80±6.68 | 112.35±7.82 | 124.10±7.35 | 0.0033 | HS |
| P 10 | 122.95±7.82 | 119.85±8.37 | 129.35±7.03 | 0.00102 | HS |
| P 20 | 122.10±7.91 | 116.35±10.41 | 134.20±10.82 | <0.00001 | HS |
| P 30 | 119.35±7.74 | 113.72±10.27 | 140.20±9.49 | <0.00001 | HS |
| After Release of CO2 | 114.15±8.13 | 110.40±9.91 | 121.95±8.83 | 0.00055 | HS |
| After Extubation | 124.55±7.34 | 118.60±10.57 | 138.75±10.46 | <0.00001 | HS |
P0, P10, P20, P30 = before & 10, 20, 30 minutes after pneumoperitoneum, respectively;
NS = Not significant, HS = Highly significant, S = Significant, SAP = Systolic arterial pressure
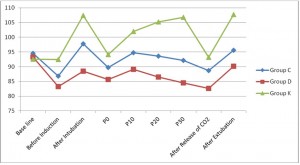
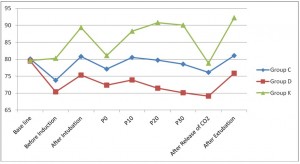
Mean and diastolic arterial pressure was significantly higher in group K (specially after intubation, at P20, P30 and after extubation). It was significantly lower in group D (Figure 3 and 4, table 4 and 5).
Figure 3. Changes in mean arterial pressure in three groups
Table 4. Changes in mean arterial pressure in three groups (Mean ± SD)
| MAP (mm Hg) | Group C | Group D | Group K | P value | Significance |
| Base line | 94.50±9.54 | 93.25±8.03 | 92.60±9.63 | 0.79895 | NS |
| Before Induction | 86.85±8.83 | 83.25±7.87 | 92.45±9.57 | 0.00617 | HS |
| After Intubation | 97.75±11.10 | 88.50±6.85 | 107.40±8.18 | <0.00001 | HS |
| P 0 | 89.75±6.07 | 85.70±6.84 | 94.15±8.36 | 0.00194 | HS |
| P 10 | 94.70±6.49 | 89.15±6.66 | 101.95±6.70 | <0.00001 | HS |
| P 20 | 93.60±6.31 | 86.45±7.52 | 105.20±9.68 | <0.00001 | HS |
| P 30 | 92.10±6.56 | 84.50±7.59 | 106.75±8.90 | <0.00001 | HS |
| After Release of CO2 | 88.65±7.33 | 82.65±8.55 | 93.20±6.57 | 0.00021 | HS |
| After Extubation | 95.60±6.68 | 90.10±8.93 | 107.75±7.99 | <0.00001 | HS |
P0, P10, P20, P30 = before & 10, 20, 30 minutes after pneumoperitoneum, respectively;
NS = Not significant, HS = Highly significant, MAP = Mean arterial pressure
Figure 4. Changes in diastolic arterial pressure in three groups
Table 5. Changes in diastolic arterial pressure in three groups (Mean ± SD)
| DAP (mm Hg) | Group C | Group D | Group K | P value | Significance |
| Base line | 80.10±10.86 | 79.45±9.01 | 79.60±10.37 | 0.9776 | NS |
| Before Induction | 73.80±10.72 | 70.35±9.61 | 80.25±10.67 | 0.0127 | S |
| After Intubation | 80.85±6.23 | 75.35±8.86 | 89.35±9.15 | 0.00001 | HS |
| P 0 | 77.10±6.28 | 72.40±8.11 | 81.10±9.60 | 0.00525 | HS |
| P 10 | 80.55±6.44 | 73.85±8.25 | 88.25±7.21 | <0.00001 | HS |
| P 20 | 79.70±6.10 | 71.50±9.03 | 90.75±10.35 | <0.00001 | HS |
| P 30 | 78.60±6.42 | 70.11±8.54 | 90.05±10.36 | <0.00001 | HS |
| After Release of CO2 | 76.15±7.20 | 69.15±9.33 | 78.80±8.13 | 0.00153 | HS |
| After Extubation | 81.05±7.01 | 75.85±9.49 | 92.25±9.39 | <0.00001 | HS |
P0, P10, P20, P30 = before & 10, 20, 30 minutes after pneumoperitoneum, respectively;
NS = Not significant, HS = Highly significant, S = Significant, DAP = Diastolic arterial pressure
DISCUSSION
Hemodynamic changes with pneumoperitoneum were first recognized in 194711. Increased intra-abdominal pressure due to insufflation of gas may compress venous capacitance vessels causing an initial increase followed by a sustained decrease in preload as venous return decreases, while arterial compression may increase after-load and systemic vascular resistance6. At intra-abdominal pressure of 15 mm Hg, Joris et al4 found a 35% increase in mean arterial pressure, a 65% increase in systemic vascular resistance, a 90% increase in pulmonary vascular resistance, while there was a 20% decrease in cardiac output. Ishizaki et al12 tried to determine the safe range of intra-abdominal pressures during laparoscopic surgery. At 16 mm Hg of intra-abdominal pressure, significant fall in cardiac output was observed. However, at 12 mm Hg of intra-abdominal pressure, hemodynamic alterations were not observed. During laparoscopy, the current recommendation is to monitor intra-abdominal pressure and to keep it as low as possible. In this present study, mean intra-abdominal pressure was maintained at 14 mm Hg throughout the duration of surgery.
Hemodynamic perturbations during pneumoperitoneum can be harmful especially in elderly and hemodynamically compromised patients23. Joris JL et al13 opined that vasopressin and catecholamines, more particularly norepinephrine, probably mediate the increase in systemic vascular resistance in pneumoperitoneum. To date, many different techniques and pharmacological agents have been used to reduce the detrimental effects of pneumoperitoneum. Techniques like reduction in intra-abdominal pressure during pneumoperitoneum and gasless laparoscopy using abdominal elevators have been tried24. Pharmacological agents like β-blockers, opioids, increasing concentration of inhalational anesthetic agents, nitroglycerine and α2-adrenergic agonists have been tried1, 7, 8.
The α2-agonists, including clonidine and dexmedetomidine, decrease central sympathetic outflow by acting like a brake and modify intraoperative cardiovascular and endocrine responses favourably to surgical stimuli, laryngoscopy and laparoscopy14. Both clonidine and dexmedetomidine have been shown to reduce sympathetic nervous system activity and plasma catecholamine concentrations.
Clonidine, with an elimination half life of 6 to 10 hours, is a centrally acting selective partial α2-agonist (α2: α1 = 220 : 1). It is known to induce sedation, decrease anesthetic drug requirement and improve perioperative hemodynamics by attenuating blood pressure and heart rate responses to surgical stimulation, and protecting against perioperative myocardial ischemia9. It provides sympathoadrenal stability and suppresses renin angiotensin activity. There are studies indicating benefits of using clonidine for maintenance of hemodynamic stability in laparoscopic cholecystectomy. Malek et al15 used 150 μg of clonidine as intravenous infusion and intramuscularly while Sung et al16 and Yu et al17 used 150 μg of oral clonidine as premedication for maintenance of hemodynamic stability during pneumoperitoneum. Yu et al even recommended its routine use as premedication in laparoscopic surgeries. Das et al18 also used 150 μg of oral clonidine 90 minutes prior to surgery to prevent hemodynamic response to pneumoperitoneum in laparoscopic cholecystectomy. Kalra et al9 used clonidine 1 µg/kg intravenously over a period of 15 minutes before pneumoperitoneum and clonidine group patients showed significantly better hemodynamic control than control group. Similar findings were obtained in the present study. However, higher doses of clonidine resulted in significant bradycardia and hypotension25.
Dexmedetomidine, with an elimination half life of 2 to 3 hours is a highly selective, potent and specific α2-agonist (α2: α1 = 1620 : 1), and is 7 to 10 times more selective for α2 receptors compared to clonidine with a shorter duration of action. It is considered full agonist at α2 receptors as compared to clonidine, which is considered as a partial agonist. Similar to clonidine, dexmedetomidine also attenuates the hemodynamic response to tracheal intubation, decreases plasma catecholamine concentration during anesthesia and decreases perioperative requirements of inhaled anesthetics10. Jaakola et al19 found decreased BP and heart rate during intubations following the administration of 0.6 μg/kg bolus of dexmedetomidine preoperatively. Lawrence et al20 found decreased hemodynamic response to tracheal intubation or extubation following a single high dose of dexmedetomidine (2 μg/kg). Ghodki et al21 used dexmedetomidine 1 µg/kg intravenously over 15 minutes before induction followed by maintenance infusion of 0.2 µg/kg/h and observed favorable vasopressor response during laryngoscopy, with minimal change in BP with pneumoperitoneum. In the present study, a single dexmedetomidine bolus of 1 µg/kg was used before induction and similar hemodynamic control was noted.
α2-agonists have also been reported to increase the risk of hypotension and bradycardia, specially in young healthy volunteers during rapid bolus administration20, 22. In this study, 3 patients of group D required intravenous atropine administration due to bradycardia.
CONCLUSION
Administration of clonidine or dexmedetomidine before commencement of pneumoperitoneum effectively attenuates hemodynamic response to pneumoperitoneum. However, dexmedetomidine blunts the hemodynamic response to pneumoperitoneum more effectively with a greater chance of developing hypotension and bradycardia.
REFERENCES
1. Joris J. Anesthetic management of laparoscopy. In – Miller’s Anesthesia 5th ed. New York: Churchill Livingstone; 1994. p. 2011–2029.
2. Wabha RW, Beique F, Kleiman SJ. Cardiopulmonary function and laparoscopic cholecystectomy. Can J Anaesth 1995;42:51-63. [PubMed]
3. Sharma KC, Brandstetter RD, Brensilver JM, Jung LD. Cardiopulmonary physiology and pathophysiology as a consequence of laparoscopic surgery. Chest 1996;110:810-5. [PubMed]
4. Joris JL, Noirot DP, Legrand MJ, Jacquet NJ, Lamy ML. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg 1993;75:1067–1071. [PubMed]
5. Glick DB. The Autonomic Nervous System; In – Miller’s Anesthesia 7th ed. New York: Churchill Livingstone; 2010 page number.
6. O’ leary E, Hubbard K, Tormey W et al. Laparoscopic cholecystectomy: haemodynamic and neuroendocrine responses after pneumoperitonium and changes in position. Br J Anaesth 1996;76:640-644. [PubMed] [Free Full Text]
7. Koivusalo AM, Scheinin M, Tikkanen I, et al. Effects of esmolol on haemodynamic response to CO2 pneumoperitoneum for laparoscopic surgery. Acta Anaesthesiol Scand 1998;42:510-7. [PubMed]
8. Lentschener C, Axler O, Fernandez H, et al. Haemodynamic changes and vasopressn release are not consistently associated with carbon dioxide pneumoperitoneum in humans. Acta Anaesthesiol Scand 2001;45:527-35. [PubMed]
9. Kalra NK, Verma A, Agarwal A, Pandey HD. Comparative study of intravenously administered clonidine and magnesium sulfate on hemodynamic responses during laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol 2011;27:344-48. [PubMed] [Free Full Text]
10. Stoelting RK, Hiller SC. Pharmacology and physiology in Anaesthetic Practice: 4th ed.
11. Booker WM, French DM, Molano PA. Further studies on the acute effects of intra abdominal pressure. Am J Physiol 1947;149:292-8. [PubMed]
12. Ishizaki Y, Bandae Y, Shimomura K, Abe H, Ohtomo Y, Idezuki Y. Safe intra abdominal pressure of carbon dioxide pneumoperitoneum during laparoscopic surgery. Surgery 1993;114:549-54. [PubMed]
13. Jean L Joris, Jean-Daniel Chiche, Jean-Luc M. Canivet, Nicolas J. jacquet, jean Jacques Y. Legros, maurice L. Lamy. Hemodynamic changes induced by laparoscopy and their endocrine correlates: effects of clonidine. JACC 1998;32(5):1389-96. [PubMed]
14. Dexter F, Chestnut DH. Analysis of statistical tests to compare visual analog scale measurements among groups. Anesthesiology 1995;82:896-902. [PubMed] [Free Full Text]
15. Malek J, Knor J, Kurzova A, Lopourova M. Adverse hemodynamic changes during laparoscopic cholecystectomy and their possible suppression with clonidine premedication. Comparison with intravenous and intramuscular premedication. Rozhl Chir 1999;78:286-91. [PubMed]
16. Sung CS, Lin SH, Chan KH, Chang WK, Chow LH, Lee TY. Effect of oral clonidine premedication on perioperative hemodynamic response and postoperative analgesic requirement for patients undergoing laparoscopic cholecystectomy. Acta Anaesthesiol Sin 2000;38:23-9. [PubMed]
17. Yu HP, Hseu SS, Yien HW, Teng YH, Chan KH. Oral clonidine premedication preserves heart rate variability for patients undergoing larparoscopic cholecystectomy. Acta Anaesthesiol Scand 2003;47:185-90. [PubMed]
18. Mrinmoy Das, Manjushree Ray, Gauri Mukherjee. Hemodynamic changes during laparoscopic cholecystectomy: effect of oral clonidine premedication. Indian J Anaesth 2007;51:205-10. [Free Full text]
19. Jaakola ML, Melkkila-Ali T, Kanto J, Kallio A, Scheinin H, Scheinin M. Dexmedetomidine reduces intraocular pressure, intubation responses and anesthetic requirements in patients undergoing ophthalmic surgery. Br J Anaesth 1992; 68: 570-5. [PubMed] [Free Full Text]
20. Lawrence CJ, De Lange S. Effects of a single pre-operative dexmedetomidine dose on isoflurane requirements and perioperative hemodynamic stability. Anaesthesia 1997;52:736-44. [PubMed]
21. Ghodki PS, Thombre SK, Sardesai SP, Harnagle KD. Dexmedetomidine as an anesthetic adjuvant in laparoscopic surgery: An observational study using entropy monitoring. J Anaesthesiol Clin Pharmacol 2012;28:334-8. [PubMed] [Free Full Text]
22. Yildiz M, Tavlan A, Tuncer S, Reisli R, Yosunkaya A, Otelcioglu S. Effect of dexmedetomidine on hemodynamic response to laryngoscopy and intubation; Perioperative hemodynamics and anaesthetic requirements. Drugs R D 2006;7:43–52. [PubMed]
23. Dhoste K, Lacoste L, Karayan J, et al. Haemodynamic and ventilatory changes during laparoscopic cholecystectomy in elderly ASA III patients. Can J Anaesth 1996;43:783-8. [PubMed]
24. Lindgren L, Koivusalo AM, Kellokumpu I. Conventional pneumoperitoneum compared with abdominal wall lift for laparoscopic cholecystectomy. Br J Anaesth 1995;75:567-72.[PubMed] [Free Full Text]
25. Ray M,Bhattacharjee DP, Hajra B, Pal R, Chatterjee N. Effect of clonidine and magnesium sulphate on anaesthetic consumption, haemodynamics and postoperative recovery: A comparative study. Indian J Anaesth 2010;54:137-41. [PubMed] [Free Full Text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube