Sukhyanti Kerai, MD, Anju R. Bhalotra, MD, Saipriya Tewari, MD, Anil Misra, MD
Department of Anesthesiology & Critical Care, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi, (India)
Correspondence: Dr. Sukhyanti Kerai, Department of Anesthesiology & Critical Care, Maulana Azad Medical College / Lok Nayak Hospital, Bahadur Shah Zaffar Marg, New Delhi-110002, (India); Cell: +91-9968527122; E-mail: drsukhi25@gmail.com
ABSTRACT
A 17 year old boy, post tracheoplasty, presented to emergency in respiratory distress with presence of stridor at rest. Flexible bronchoscopy revealed granulations at tracheal graft site causing airway stenosis. The presence of graft perculded use of invasive surgical approaches due to risk of damage.The anesthetic management options in this case carried inherent risks of causing total airway obstruction and impairing surgical access. We decided to perform the electrocauterization of tracheal granulations using subglottic jet ventilation while placing the catheter above the stenotic trachea.
Key words: Tracheal granulations; Airway obstruction; Anesthesia; Jet ventilation
Citation: Kerai S, Bhalotra AR, Tewari S, Misra A. Near total airway obstruction due to tracheal granulations: an anesthesiologist’s nightmare. Anaesth Pain & Intensive Care 2016;20(4):480-483
Received: 17 Apr 2016; Reviewed: 11, 15 Jun 2016; Corrected: 17 Jun 2016; accepted: 17 Jun 2016
INTRODUCTION
Critical tracheal obstruction is a rare life threatening condition. The optimal management of such condition remains controversial with no consensus to an ideal approach. We report a case of tracheal granulations leading to critical tracheal obstruction where the airway management was further complicated by the presence of a tracheal graft in the anterior tracheal wall.
CASE REPORT
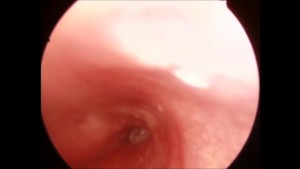
A 17 year old boy presented to emergency with gradually progressive respiratory difficulty for the last 20-25 days with complaints of stridor at rest, tachypnea and tachycardia. He was a follow-up case of tracheoplasty done 4 months ago for tracheal stenosis. A tentative diagnosis of tracheal restenosis or tracheal narrowing due to granulation tissue or infection at the suture line was made and the patient was immediately shifted to the operating room (OR) for urgent evaluation and intervention to relieve his life threatening stridor. The OR was appropriately prepared and the difficult airway cart which included a pediatric fiberoptic bronchoscope, Manujet III Jet ventilator (VBM Medizintechnik GmbH, Germany) and rigid bronchoscopes (Karl Storz endoscopy- America, Inc., Culver City, CA. sizes 4.0, 5.0, 6.0 and 6.5). The patient was nebulized with L-adrenaline (1 ml of 1:1000 solution in 5 ml of normal saline) and inj. dexamethasone 8 mg was administered IV. After discussion with the surgeons it was decided to avoid transtracheal approaches in order to preserve the tracheal graft. A quick look through the flexible fiberscope by the senior anesthesiologist, using spray as you go (SAYGO) technique with the patient awake confirmed tracheal granulations obstructing the upper part of trachea (Figure 1). The lumen was assessed visually by surgeons, appeared to be only 10-15% of the normal. The fiberscope was not advanced upto or below the granulation tissue due to fear of complete airway obstruction. The surgeons planned to cauterize granulation tissue under general anesthesia.
Figure 1: Tracheal granulations obstructing lumen of upper part of trachea
As we were not sure about the lower extent of the granulations and there was doubt about passage of 3.5-4 mm ETT, we decided not to instrument the airway and to proceed with an open technique of ventilation using manual jet ventilation (MJV). As rescue plan a smaller sized rigid bronchoscope was kept ready to bypass the tracheal obstruction, failing of which we would have resorted to the option of performing tracheostomy though the graft using a drill or opening up the lateral suture line between the graft and normal trachea. General anesthesia was induced cautiously with slow intravenous midazolam 1 mg, fentanyl 50 µg and propofol 80 mg taking care to maintain spontaneous respiration at all times. The surgeons then introduced a suspension laryngoscope and placed jet ventilation catheter [Jet-Katheter (oral) 40cm long, VBM Medizinintechnik GmbH] below the vocal cords but above the granulations (Figure 2).
Figure 2: Jet catheter placed above the granulation tissues

Anesthesia was maintained using manual controlled infusion of propofol which was initiated at the rate of 100mcg/kg/min and was stepped up to 300 µg/kg/min. Jet ventilation was initiated at 1 bar pressure and increased slowly to 3 bar pressure based on the degree of chest expansion. Manual low frequency jet ventilation was continued at a rate of 20-25 breaths per minute using Manujet III, ensuring adequate time for exhalation. During the procedure, the adequacy of jet ventilation was continuously assessed by observation of chest movements and by oxygen saturation readings. The patency of the airway and any surgical obstruction were also assessed by watching the endoscopic image on a television. Although no neuromuscular blocker was administered, a good working field was provided by intermittent boluses of 20-30 mg propofol and local anesthetic instillation. Granulations were electrocauterised and excised meticulously by the surgeons. SpO2 remained > 95% at all times and intraoperative arterial blood gas analysis done towards conclusion of surgery showed a PaCO2 of 48 mmHg. Jet ventilation was conducted uneventfully and there was no hemodynamic compromise. During use of cautery jet ventilation was interrupted to minimize chances of airway fire. The procedure lasted for about 30 min. The luminal diameter of trachea after complete removal of granulation tissues appeared less than normal possibly because of previous tracheoplasty (Figure 3).
Figure 3: Tracheal lumen after cauterization of granulation tissue

At the end of the procedure, the jet catheter was removed and a Proseal-LMA size 3 was inserted and the patient was allowed to breathe spontaneously and awaken up. Postoperatively the patient was shifted to high dependency unit, where he was kept propped-up with continuous oxygen supplementation and steroid coverage for 24 hours. Later the patient was planned to undergo serial tracheal dilatations.
DISCUSSION
The patients with advanced airway obstruction and stridor at rest comprise some of the most feared and complicated cases for anesthesiologists. The optimal airway management for such patients is controversial and best management technique should be selected depending on the urgency of the situation, site and extent of airway obstruction and available equipments and expertise. The urgent nature of the present case precluded any diagnostic work up. However, the history and clinical features provided an important guide to the location and severity of obstruction. The presence of biphasic stridor at rest led to conclude that the reduction in airway diameter was at least 50% at the subglottic or cervical part of the trachea. The history of tracheoplasty done few months back led us to suspect that the cause of obstruction may be granulation tissues, tracheal re-stenosis or infection at the site of tracheal graft. Preoperative nebulization with adrenaline was done considering the possibility of infection at recent graft site causing airway edema and obstruction. Although nebulization with adrenaline is described to be a safe approach and there are only three case reports about its adverse effects in healthy pediatric patients, it should always be used cautiously with appropriate monitoring1.
There is difference in opinions among experts regarding choice of anesthesia, induction techniques (inhalational versus intravenous) and administration of neuromuscular blockade (spontaneous versus controlled ventilation). Inhalational induction classically has been considered to be safer in such patients2; however it can be prolonged in the presence of airway obstruction and can also lead to airway irritation and coughing precipitating total airway obstruction. We opted for intravenous induction with slow titrated propofol which allowed smooth induction of anesthesia. Also the tolerance to airway instrumentation is better with propofol as compared to inhalational agents. Undoubtedly ablation of spontaneous respiration provides better surgical conditions and prevents coughing and bucking during instrumentation and decreased the requirement of propofol. In present case airway was precarious and emergent invasive airway access was also near impossible so at that point it seemed safer to maintain spontaneous respiration. Although no neuromuscular blocker was administered, a good working field was provided by intermittent boluses of propofol and local anesthetic instillation. Whatever technique is chosen, it is important to recognize that every technique has limitations and it may fail and back up plans should be ready.
Extracorporeal membrane oxygenation (ECMO) is probably the safest option if there is near total tracheal obstruction. Over the years it has been used for many types of critical airway obstructions5 and has been reported to be lifesaving after failed intubation; however, the facility of ECMO is not available in our center, as is the case with most of the healthcare institutions in our country other than cardiac surgery centers.
The MJV technique has previously been used successfully for management of endoscopic laryngeal and tracheal lesions.3 However, it has many drawbacks including hypoxemia and hypercarbia due to operator dependent ventilation, risk of aspiration of blood and debris, air trapping due to incomplete exhalation leading to barotrauma and hemodynamic instability. However, despite the limitations of use of MJV, it continues to predominate over automated jet ventilation. At our centre the automated HFJV is not available. The complications of MJV could be related to skill and experience of operator.4 If the degree of obstruction is severe and MJV method is used, slow respiratory rates should be used to permit long expiratory time. In our case the jet ventilation catheter was kept above the tracheal lesion, a ventilatory rate of 20-25/min was employed and the patency of airway was continuously monitored clinically. The procedural time and duration of MJV was around 30 min, the ABG done towards end of surgery showed mild hypercarbia. HFJV with jet catheter applied above the stenosis (ASV) has been observed to create more air entrainment and greater distal airway pressure compared catheter passed through the stenosis (TSV) or when catheter is passed via cricothyrotomy (BSV).5 We did not performed TSV as the lumen of trachea was observed to be very narrow and stenotic aperture could have been partially or completely obstructed by jet catheter and thus increasing impedance to exhalation. BSV was avoided in order to preserve tracheoplasty done previously. The barotraumas observed during jet ventilation were due to failure of coordination between the surgeon and anesthesiologist, consequence of jetting during a laryngospasm or misplaced transtracheal catheters.6 These observations suggest that barotraumas are often due to “pilot errors” rather than a failure of the technique. Therefore, the clinical monitoring of patient is the standard method to prevent barotraumas. The anesthetist must keep their eyes and hands on the thorax and listen to each outflow sound to verify the unobstructed outflow of air after each inspiration. During jet ventilation techniques laryngospasm can be prevented by ensuring an adequate level of anesthesia, analgesia and muscle relaxation.
Modern automated jet ventilators featuring a pressure monitor or alarm and automatic shutdown when airway pressure exceeds the preset limits may enhance safety of jet ventilation. The use of Ventrain®, a portable manually operated low pressure, flow regulated jet ventilator which also provides expiratory assistance based on venturi principle could be a promising modality for management of total obstructed airways.7
CONCLUSION
The optimal airway management in above case had dual challenges of providing adequate surgical field and preserving tracheal graft. Although the use of MJV is reserved for short duration, uncomplicated procedure, it seemed only rational technique in our patient after considering available resources. The use of MJV in such cases requires attention to prevent barotrauma and hypercarbia by using low recommended jet pressure to start with and gradually increase if required, allowing adequate time for expiration. Clinical monitoring to ensure unobstructed outflow of gases and to provide adequate depth of anesthesia will also be required.
Conflict of Interest: None.
Authors’ contribution: All of the authors took part in concept, manuscript writing, literature search and references.
REFERENCES
- Akca H, Tuygun N, Karacan CD. Nebulized epinephrine treatment in pediatric emergency department. Pediat Therapeut. 2014 :4:210. [PubMed] doi:10.4172/2161-0665.100210.
- Patel A, Pearce A. Progress in management of the obstructed airway. Anaesthesia. 2011 Dec ;66 Suppl 2:93-100. [PubMed] doi: 10.1111/j.1365-2044.2011.06938.x.
- Pinsonneault C, Fortier J, Donati F. Tracheal resection and reconstruction. Can J Anaesth. 1999 May;46(5):439-55. [PubMed]
- Cook TM, Alexander R. Major complications during anaesthesia for elective laryngeal surgeries in UK: a national survey of use of the use of high pressure source ventilation. Br J Anaesth. 2008 Aug;101(2):266-72. [PubMed] [Free full text] doi: 10.1093/bja/aen139
- Buczkowski PW, Fombon FN, Lin ES,Russell WC, Thompson JP. Air entrainment during high- frequency jet ventilation in a model of upper tracheal stenosis. Br J Anaesth. 2007 Dec;99 (6):891-7. [PubMed] [Free full text]
6.Jaquet Y, Monnier P, Van Melle G, Ravussin P, Spahn DR,Chollet –Rivier M. Complications of different ventilator strategies in endoscopic laryngeal surgeries: a 10 year review. Anesthesiology. 2006 Jan;104(1):52-9. [PubMed]
7.Borg PA, Hamaekers AE, Lacko M, Jansen J, Enk D. Ventrain for ventilation of lungs. Br J Anaesth. 2012;109(5):833-4.. [PubMed] [Free full text] doi: 10.1093/bja/aes366




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube