Iftikhar Ahmed, Umair Younus, Rawail Iftikhar, Kaleem Ahmad
Department of Pediatric Anesthesia & Intensive care, AFIC/NIHD, Rawalpindi.
Correspondence: Brig Iftikhar Ahmed,HoD, Department of Pediatric Cardiac Anesthesia & Intensive Care, Armed Forces Institute of Cardiology / National Institute of Heart Diseases, The Mall, Rawalpindi46000 (Pakistan); E-mail: iftikhar477@hotmail.com
ABSTRACT
Double outlet left ventricle (DOLV) is a rare but substantial congenital cardiac anomaly, presenting with varied anatomical findings. This requires a relevant surgical approach, pertinent to the type of presentation. The condition can be quite difficult to diagnose. This implies the need for scrutiny and sensitive diagnostic procedures during the pre-op period. The case presented here was in a critical state on admission and was stabilised with Sildenafil during the pre-op preparation. A surgical plan for Arterial Switch was made, keeping in mind the diagnosis suggestive of TGA, VSD with an AP Window at first. DOLV was confirmed on the operating table and Rastelli type of correction was performed with a relatively uneventful stay in the post-op ICU.
Key words: Cardiac Surgical Procedures/methods; Child; Double Outlet Right Ventricle/surgery; Double Outlet Right Ventricle/ultrasonography; Sildenafil Citrate; Rastelli Procedure; Arterial Switch Operation
Citation: Ahmed I, Younus U, Iftikhar R, Ahmad K. Double outlet left ventricle: management. Anaesth Pain & Intensive Care 2016;20 Suppl 1:S165-S167
Received: 28 September 2016; Reviewed: 29 September 2016; Corrected; 5 October 2016; Accepted: 5 October 2016
INTRODUCTION
Double Outlet left ventricle is quite a rare and indistinct congenital anomaly present in the cardiac world. There have been cases reported worldwide previously,1-7highlighting the emphasis on the diagnostic evaluation and embryological origin of the disease. Its pre-natal diagnosis warrants utmost importance provided its non-apparent presentation. This is the first case of this magnitude being reported and presented in Pakistan.
CASE REPORT
The patient was a six month old baby boy, who was referred to Novick Cardiac Alliance via Zwan Family Charity Trust in Afghanistan. The team at Armed Forces Institute of Cardiology agreed to admit the baby during a planned ongoing collaborative surgical programme.
The baby was admitted in a very frail condition. He had a normal birth with his weight recorded to be3.6 kg. The pregnancy was uneventful with no known exposure to teratogens or x-rays by the mother. On examination he had apparent dyspnea and central cyanosis. The vital signs recorded at that time were; HR- 155 bpm; SpO2 71%; RR 55/min; and BP 70/40 mmHg. Initial chest x-ray did not show any gross abnormality, and blood tests were within normal limits except a low serum sodium level at 129 mmol/l. The initial echo findings (Figure 1) suggested a differential diagnosis of D-TGA, VSD and an AP window with pulmonary hypertension
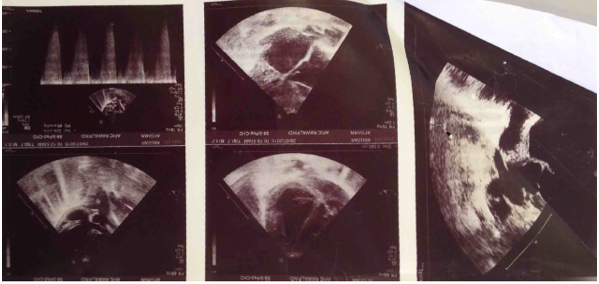
Figure 1: Preoperative echocardiography showing TGA + VSD + AP window with pulmonary hypertension
Surgery was planned and he was put on oxygen therapy and sildenafil citrate 2 mg/kg every 6 hours. On opening the heart the pre-op diagnosis of TGA, VSD and AP window was found to be incorrect and the final diagnosis of ‘double outlet left ventricle with a peri-membranous VSD was noted. The operation was performed via a median sternotomy with right atrial and right ventricular incisions. Infundibulectomy of right ventricle and the VSD was closed using a Dacron patch and the right ventricle was inserted in to the main pulmonary artery via a valved conduit composed of cor-matrix.
He was rewarmed and weaned off from bypass on epinephrine 0.03 µg/kg/min and milrinone 0.5 µg/kg/min and transferred to the PICU for further management.
The baby was admitted to the PICU on 5th October 2015 in a stable condition, though a significant level of bleeding was noted. Blood and blood products were given to reverse coagulopathy. He had generalised edema and a significant capillary leak with hepatomegaly. This was presumed to be a systemic inflammatory response syndrome (SIRS) post bypass coupled with slight malposition of the IVC cannula during bypass. A furosemide infusion was commenced on the 1st postoperative night and continued for 2 days. After achieving a negative fluid balance and resolution of symptoms this was changed to intermittent IV furosemide and finally oral furosemide prior to discharge
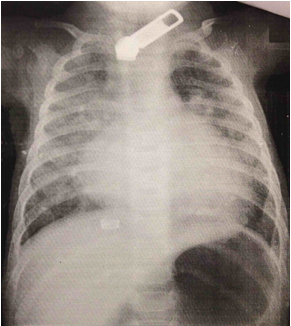
Figure 2: Preoperative chest x-ray
Chest x-ray initially showed a level of interstitial edema (Figure 2), which resolved by 2nd postop day and further x-rays were normal. He had one mediastinal chest drain in situ and had significant bleeding (10 ml/kg/hr), 4 hours postoperative ultrasound showed large right pleural effusion and a right pleural drain was inserted immediately, this drained 150 ml of blood. Epinephrine infusion up to 0.07 µg/kg/min and milrinone infusion up to 0.5 µg/kg/min were used. He remained in sinus rhythm throughout his admission. He was started on heparin when bleeding subsided and transferred to soluble aspirin 5 mg/kg daily on the 2nd postoperative day. Pain was managed with paracetamol, ibuprofen and nalbuphine IV in the initial postoperative period. Cefazolin and amikacin were given postoperatively as normal prophylaxis, vancomycin was added on day 2 in response to a raised white cell count and positive CRP result and continued for 5 days.
Postoperative echo showed a stable VSD patch and near laminar flow through the conduit. Captopril at 0.3 mg/kg thrice daily was established before discharge from PICU. The chest drains were removed on the 3rd postoperative day after yielding zero drainage for 15 hours. He was extubated successfully to oxygen through nasal cannula after 3 days. IV antibiotics were discontinued on day 5 and he had no other infection markers.
The boy was discharged to the high dependency unit on oxygen 0.5 L/min via nasal cannula; oxygen was weaned off over the following 2 days. He was feeding well and had regained a normal sleeping pattern and was discharged to the children’s ward after two days.
DISCUSSION
In comparison to double outlet right ventricle (DOLR), double outlet let ventricle (DOLV) is quite rare. It can be defined as the origin of both pulmonary artery and aorta either completely or mostly from the morphological left ventricle.
However, it presents in a wide array of anatomical variations; and Van Praagh et al5described at least 14 different types. In regards to those malformations which arise from the morphological right ventricle, which is actually left sided due to associated ventricular inversion are best termed as variants of DOLR (Kiser et al, 1968)2. There are three major anatomical findings that these variations correspond with. These include the presence or absence of a ventricular septal defect and pulmonary stenosis, distribution of conal musculature and relationship of the great arteries.
In a case presented by Sakakibara et al in 19671, there was a large subpulmonary conal defect with no pulmonary stenosis. The aorta and the pulmonary artery were normally related. In comparison, Kerr et al (1973)3 put forward a case which had a subpulmonary VSD with severe pulmonary stenosis. The aorta and pulmonary artery again were normally related.
Khanolkar in 1990 reported for the first time a case of DOLV which was associated with tricuspid atresia and cor triatriatum dexter,6 which is very rare due to the persistence of the embryonic right valve of the sinus venosus.
The advent of 2D echo provided a breakthrough in diagnosis of DOLV which was earlier only possible by virtue of cardiac catheterization or intra-operatively. Peter and Brandt et al4 in 1976 highlighted the importance of using radiologic progression (usually left anterior oblique) that profiles the ventricular septum, only then a diagnosis can be established.
Different variants of DOLV require different surgical approaches. Our case was mostly similar to one presented by Kerr in 1973 and a Rastelli type of correction was performed. The VSD was closed with a Dacron patch and a right ventricle to pulmonary artery conduit was placed.
Liljeet al 2007 performed a similar repair7 except for the Blalock Taussig repair before Rastelli’s for the I-malposition of the great arteries.
CONCLUSION
To conclude, double outlet left ventricle is recognizable with modern diagnostic tools, even though it’s quite rare. A strong suspicion as a part of the differential diagnosis in cyanotic heart disease can be helpful.
Conflict of interest: None declared by the authors
Author contribution: IA: Concept and conduct of the case report; UY: Practical insight, conduct of the case; RI: Literature search and editing; KA: Conduct of the case
REFERENCES
- Sakakibara S, Takao A, Arai T, Hashimoto A, Nogi M. Both great vessels arising from the left ventricle. Bull Heart Inst Jpn. 1967;11:66-86.
- Kiser J, Ongley P, Kirklin J, Clarkson PM, McGoon D. Surgical treatment of dextrocardia with inversion of ventricles and double-outlet right ventricle. J Thorac Cardiovasc Surg. 1968;55(1):6. [PubMed]
- Kerr AR, Barcia A, Bargeron L, Kirklin JW. Double-outlet left ventricle with ventricular septal defect and pulmonary stenosis: report of surgical repair. Am Heart J . 1971;81(5):688-93. [PubMed] doi:10.1016/0002-8703(71)90013-5
- Brandt PW, Calder AL, Barratt-Boyes BG, Neutze JM. Double outlet left ventricle: Morphology, cineangiocardiographic diagnosis and surgical treatment. Am J Cardiol. 1976;38(7):897-909. [PubMed] doi:10.1016/0002-9149(76)90803-1
- Van Praagh R, Weinberg PM, Srebro JP. Double outlet left ventricle, In: Adams FH, Emmanouilides GL, Riemen Schneider TA, eds. Heart Diseases in Infants Children and Adolescents. Baltimore: Williams and Wilkins, 461-73, 1989.
- Khanolkar U, Deshpande J, Kinare S. Double outlet left ventricle with cor triatriatum. Indian Heart J. 1990;42(5):393-5. [PubMed]
- Lilje C, Weiss F, Lacour-Gayet F, Rázek V, Ntalakoura K, Weil J, Lê TP. Images in cardiovascular medicine. Double outlet left ventricle. Circulation.2007 Jan 23;115(3):e36-7. [PubMed] [Free full text] doi: 10.1161/CIRCULATIONAHA.106.629923




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube