Akshaya N. Shetti1, Rangparia Bhumika2, Bhavika Singla3, Rachita G Mustilwar4
1Associate Professor; 2Senior Resident
Department of Anesthesiology & Critical Care, Rural Medical College, Loni, Maharashtra, (India)
3Senior Resident, Fellowship Candidate in Pediatric Anesthesia, Department of Anesthesiology, LTMMC, LTMGH, Sion, Mumbai, Maharashtra, (India); E-mail: bhavikasingla201@gmail.com
4Post Graduate Trainee, Department of Periodontology and Implantology, Rural Dental College, Loni, Maharashtra, (India); E-mail: dr.rachu@gmail.com
Correspondence: Dr Akshaya. N. Shetti, Associate Professor, Department of Anesthesiology and Critical Care, Rural Medical College, Loni, Maharashtra, (India)
E-mail: aksnsdr@gmail.com
ABSTRACT
Background: World Health Organization has estimated that 3 million cases of pesticide poisoning are registered every year. Southern states of India have high prevalence rate of organophosphorus poisoning (OPP) due to many factors, including accidental, suicidal or homicidal intentions. Various clinical and laboratory tests are used to assess severity of the poisoning, but with conflicting results. This study aimed to correlate the serum acetylcholinesterase levels with morbidity, ventilation need, ICU stay and the final outcome of the ailment.
Methodology: This retrospective study was conducted in rural tertiary care of Maharashtra, India. The patients admitted from 1st January 2016 to 31st December 2016 with definitive diagnosis of OPP requiring mechanical ventilator support were included. Parameters like age, sex, serum acetylcholinesterase levels, ventilator days, ICU stay days and outcome were collected. Patients with unknown compound poisoning, referred from other hospital or brought dead were excluded. The statistical analysis was done by using Graph Pad software. Unpaired t test was used for parametric values. Pearson’s correlation test was used for correlating the values of serum cholinesterase levels with ventilator hours and ICU stay.
Results: Out of a total of 257 patients, 32 fulfilled inclusion criteria; 25 (78%) were males of whom 10 (40%) patients died, and 7 (22%) were females of whom 2 (28.5%) could not be saved. The male to female ratio was 3.6:1.The lowest and highest recorded serum acetylcholinesterase level was 178 and 6358 U/L respectively. The average ventilator hours were 66.56 ± 44.73, age distribution was 43.28 ± 16, average number of ICU stay was found to be 10.4 ± 19.68 days.
Conclusion: The prediction of morbidity or outcome, ICU stay and ventilator days cannot be made based on the levels of serum acetylcholinesterase.
Key words: Morbidity; Mortality; Organophosphorus, Poisoning; Serum cholinesterase; Ventilation
Citation: Shetti AN, Bhumika R, Singla B, Mustilwar RG. Correlation of serum acetylcholinesterase with the ventilation need, ICU stay and outcome in organophosphorus poisoning – a retrospective study. Anaesth Pain & Intensive Care 2017;21(2):199-203
Received: 20 February 2017, Reviewed: 13 April, 20 June 2017, Corrected & Accepted: 22 June 2017
INTRODUCTION
World Health Organization estimates that almost 3 million cases of pesticide poisoning are recorded every year.1 Southern states of India have high prevalence rate of organophosphorus poisoning (OPP) due to many factors.2 Organophosphates are commercially used as pesticides. These agents inhibit the acetylcholinesterase enzyme leading to accumulation of acetylcholine. The accumulated acetylcholine has effects on both muscarinic and nicotinic receptors at the synapses within the central and peripheral nervous system.3 Morbidity and mortality of a patient depends upon the concentration, type, amount consumed and the promptness of initiation of the treatment. The underdeveloped countries have higher prevalence rate.4 Various treatment regimens have been successfully tried, but the combined pralidoxime and atropine treatment remains the cornerstone.5,6 The causes of OPP are identified, among them self-poisoning and accidental exposure are the commonest in the developing countries like India. It is most commonly seen in populations of low socioeconomic status especially in rural areas where the main occupation of the people is farming. The prevalence rate is high in rural population as the above etiological factors are commonly seen in rural agricultural belt. The poor rural healthcare services and lack of good referral practices increases the mortality rate among these patients.
Along with the clinical presentation, scoring systems and the laboratory assessment of serum acetylcholinesterase enzyme are done during the treatment. Various studies have shown conflicting results while assessing the correlation of serum acetylcholinesterase level with the severity of the illness.
This retrospective study was conducted to assess whether the level of acetylcholinesterase enzyme could be used to predict the severity of the OPP, in terms of number of days for which ventilation was needed, ICU stay and the outcome. Any adverse events noted during the course of treatment were noted. Welch two tailed t test was used to compare the acetylcholinesterase levels in those who survived and those who expired.
METHODOLOGY
This retrospective study was conducted in rural tertiary care hospital of Maharashtra, India. The patients diagnosed as OPP and who required invasive mechanical ventilation support were included in this study. Inclusion criteria were; patients of both the sexes, age more than 12 year, direct admission to our hospital, and definitive diagnosis of OPP. The exclusion criteria were; unknown poisoning, patients who were brought dead, OPP patients who were not on invasive ventilation, and patients on ventilator referred from other hospital. From 1st January 2016 to 31st December 2016, a total of 257 patients admitted with the history of consumption of poison were listed. Out of these, 229 patients were diagnosed as having OPP, out of which 32 required mechanical ventilation therapy and were shortlisted and levels of serum cholinesterase, total ventilator days, total ICU stay, and outcome of those patients was noted. The statistical analysis was done by using Graph Pad software. Unpaired t test was used for parametric values. Pearson’s correlation test was used for correlating the values of serum cholinesterase levels with ventilator hours and ICU stay.
RESULTS
A total of 1001 patients got admitted in medical ICU, out of those 257 patients had history of consumption of pesticides. Out of 257 patients 32 patients fulfilled the inclusion criteria. The lowest and highest age recorded were 19 and 80 y respectively.
Out of 32 patients 25 (78%) were males of whom 10 (40%) patients died and 7 were female (22%) of whom 2 (28.5%) patients died. The male to female ratio was 3.6:1, suggesting prevalence is high among male gender. The lowest and highest recorded serum acetylcholinesterase level was 178 and 6358 U/L respectively. The median age in our study was 43.28 ± 16 y. (Table 1). Pearson’s correlation analysis revealed a negative correlation between the serum cholinesterase levels and number of ventilator days (r = -0.144, two tailed p value is 0.02) (Figure 1).
Table 1: Demographic, laboratory and ICU parameters
| Parameters | Mean ±SD, (%) | |
| AGE | 15- 45 | 16 (50%) |
| 46 -75 | 15 (46.8%) | |
| 75- 105 | 01(3.1%) | |
| Sex | Males | 25 (78%) |
| Females | 7 (22%) | |
| Serum acetylcholinesterase (u/l) | 1782.40 ± 2142.69 | |
| Duration of ventilation (h) | 66.56 ± 44.0 | |
| ICU stay (days) | 10.40±19.37 | |
| Mortality | 12 (37.5%) | |
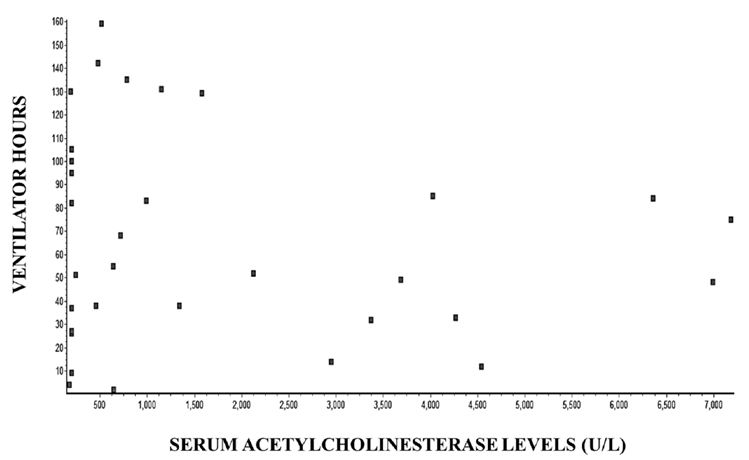
Graph 1: Correlation of serum acetylcholinesterase levels with ventilator hours
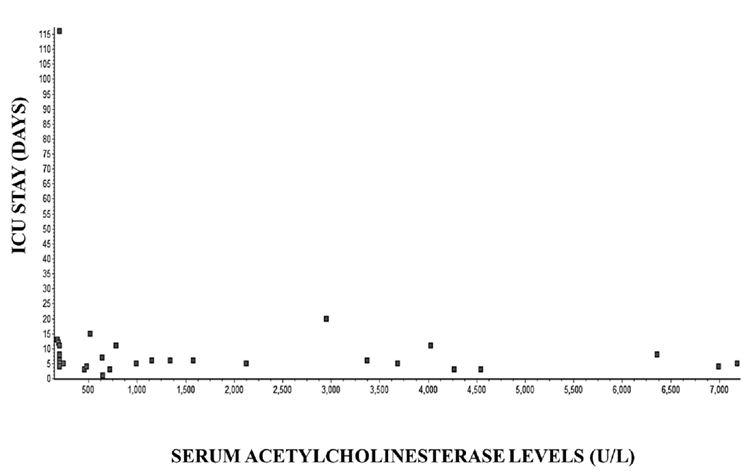
Graph 2: Correlation of serum cholinesterase levels with ICU stay
Table 2 shows the comparison of age and serum acetylcholinesterase levels between expired and survived groups. The values of serum cholinesterase levels were high (2247.05 ± 2425.04) in patients who didn’t survive in comparison with patients who survived (1008 ± 1316). There is no statistical significant difference seen between the groups.
Table 2: Comparison of age, serum acetylcholinesterase levels, ICU stay, ventilator hours in expired and survived population.
| Parameter | Expired
(mean ± SD) |
Survived
(mean ± SD) |
p value |
| Age (years) | 47.16 ±16.83 | 40.95 ±15.44 | 0.29 |
| Serum acetylcholinesterase (u/L) | 2247.05 ± 2425.04 | 1008 ±1316 | 17.0 |
| ICU stay (Days) | 15.8 ± 31.9 | 8.65 ± 7.3 | 0.34 |
| Ventilation need (hours) | 54.08 ± 41.65 | 74.05 ± 45.85 | 0.22 |
| P<0.05 is considered as significant | |||
Average ventilator hours were 66.56 ± 44.73 and average number of ICU stay was 10.4 ± 19.68 days. The least and highest days of stay in ICU were 1 and 116 respectively. Out of 32 patients 4 (12.5%) patients had to undergo tracheostomy. Out of 32 patients 12 (37.5%) patients died indicating the severity of OPP was high. A negative correlation between the serum acetylcholinesterase levels and ICU stay was observed in the study (r = -0.156, two tailed p value is 0.39) (Figure 2). Out of 32 patients tracheostomy was done in 4 (12.5%) patients and only one (3.1%) patient, developed ventilator associated pneumonia.
DISCUSSION
Various forms of poisoning cases are seen in tertiary care hospitals. In rural parts of India, especially in the agricultural belt, there has been the highest prevalence of poisoning cases. Among the poisoning cases the pesticide consumption is at the top. In our rural area it is very common to find the OPP poisoning cases due to various reasons. Among these, suicidal attempt is the commonest cause. The main reason for selecting these drugs is; these are cheap, easily available over the counter and used as a major pesticide during farming, so readily available at homes of the farmers.
The incidence of OPP was highest in patients aged less than 45 years (50%) this is in agreement with other studies.7 Surprisingly the near higher incidence of OPP is seen in the age group between 46 to 75 years (46.8%). The possible explanation is, even at this age group the people practice the agriculture and pesticides are easily accessible to them. Due to various emotional and social conflicts these people make a suicidal attempt.
In the present retrospective study, the incidence of poisoning was higher in males when compared to females (ratio 3.6:1). Similar studies showed that the males outnumbered the females.8,9 The possible cause for this may be a high incidence of alcohol consumption in rural areas among the male population. The financial burden of both the family and farming are taken care by the males and farming is the main or the only source for income. Any financial loss during the farming or after harvesting may become an emotional issue and results in attempts to suicide.
Various risk assessment scales or tests have been carried out among OPP with successful correlation.10,11 One author concluded that, serum creatinine phosphokinase, erythrocyte cholinesterase level, blood pH and total atropine consumed were correlated with severity of poisoning.12,13 This retrospective analysis revealed that the assessment of serum acetylcholinesterase levels did not predict the outcome of the OPP patient in terms of total ventilator days or total number of ICU stay, which was contrary to our findings.
The patients in survival group had a total ICU stay of 8.65 ± 7.3 days vs. 15.8 ± 31.9 days in the non-survival or expired group (p value 0.34) indicating there was no statistical significance between the two groups.
There was no statistical difference between the groups regarding duration of the mechanical ventilation (p = 0.22).
The overall mortality has been estimated to be 10 to 20%, which depends upon the mode and quantity of drug consumption, type of the compound and the duration to initiate the treatment. In our study the mortality was very high in ventilated patients, e.g. 37.5%. Our finding correlates with the findings of similar study which showed the mortality among ventilated patients to be 34.21%, indicating a high mortality rate in patients with OPP requiring mechanical ventilation.14
In our retrospective observational study, a total of 20 patients had serum acetylcholinesterase levels < 1200 U/L; Out of these 9 patients died. Serum cholinesterase levels were high (2247.05 ± 2425.04) in patients who didn’t survive in comparison to patient who survived (1008 ± 1316) (p = 17). This suggests the cholinesterase enzyme levels don’t predict the mortality rate. Similar results are observed in a study conducted by Aygun D et al. 15 The time of reaching the hospital and initiation of the treatment after the exposure to the OPP is a critical factor for the survival rate which we couldn’t study. On the contrary, low serum acetylcholinesterase levels have been implicated in failure to wean off a patient in a case report.16
Studies have shown OPP occurs mainly due to ingestion with suicidal intent.17,18 Improved medical care, provision of antidotes, sensitizing or educating the population who are vulnerable for OPP, restricting the sales of insecticides may reduce the incidence of OPP and case fatality.
LIMITATIONS
In this study, there were certain limitations; clinical severity was not recorded at the time of admission, time since exposure to initiate the treatment was not well recorded as most of the time the patients were brought to the hospital by the relatives who remained unaware of the time of exposure. The study also had a small sample size. A prospective, multicenter study with large sample size is needed to support our findings.
CONCLUSION
Based on our study results, serum acetylcholinesterase level alone is not helpful in predicting the morbidity, mortality, total ICU stay, ventilation need or the outcome. Hence it cannot be used as a predictor of morbidity or mortality among OPP patients requiring invasive ventilation.
Conflicting Interest: Nil declared by the authors
Authors’ contribution:
ANS, RB, BS, RGM, RGM – Concept, design, literature search, data acquisition & analysis, statistical analysis, manuscript preparation & editing
REFERENCES
- Narang U, Narang P, Gupta O. Organophosphorus poisoning: A social calamity. J Mahatma Gandhi Inst Med Sci 2015;20:46-51 [Free full text]
- Chintale KN, Sanjay V P, Sanjay S.C. Clinical profile of organophosphorus poisoning patients at rural tertiary health care centre. Int J Adv Med. 2016;3(2):268-274 [Free full text] DOI:http://dx.doi.org/10.18203/2349-3933.ijam20161074
- Goldfrank LR. Goldfrank’s Toxicologic Emergencies. 7th ed. New York: McGraw Hill, 2002;1346-1360.
- World Health Organization. WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification 2000- 2001. WHO/PCS/01.4. Geneva: World Health Organization, 2001. [Free full text]
- Altintop L, Aygun D, Sahin H, Doganay Z,Guven H, Bek Y, et al. In acute organophosphate poisoning the efficacy of hemoperfusion on clinical status and mortality. J Intensive Care Med 2005;20:346-350. [PubMed] [Free full text]
- Okonek S. Probable progress in the therapy of organophosphate poisoning: extracoporeal hemodialysis and hemoperfusion. ArchToxicol 1976;35:221-227. [PubMed]
- Karalliedde L, Senanayake N. Acute organophosphorus poisoning in Sri Lanka. Forensic Sci Int. 1988;36:97–100. [PubMed] [Free full text] DOI:http://dx.doi.org/10.1016/0379-0738(88)90220-4
- Kamenczak A, Jasiǹska-Kolawa K, Targosz D, Szkolnicka B, Sancewicz-Pach K. Acute pesticides poisoning in the Krakow Department of Clinical Toxicology in 1986-1995. Przegl Lek. 1997;54:671–6. [PubMed]
- Stefanos NK, David CC. Acute chemical emergencies. New Eng J Med. 2004;350:800–8. [PubMed]
- du Toit PW, Muller FO, VanTonder WM, Ungerer MJ. Experience with intensive care management of organophosphate insecticide poisoning. S Afr Med J. 1998;60:227–9. [PubMed]
- Srinivas R, Venkateswarlu V, Surender T, Eddleston M, Nick AB. Pesticide poisoning in south India: Opportunities for prevention and improved medical management.Trop Med Inter Health. 2005;10:581–8. [PubMed] [Free full text]
- Safdar A, Saeed A, Muhammad NR. Organophosphorus poisoning: Emergency management in intensive care unit. 2003;10:308–14.
- Ahmed SM, Das B, Nadeem A, Samal RK. Survival pattern in patients with acute organophosphate poisoning on mechanical ventilation: A retrospective intensive care unit-based study in a tertiary care teaching hospital.Indian J Anaesth 2014;58(1):11-17. [PubMed] [Free full text] doi: 10.4103/0019-5049.126780.
- Muley A, Shah C, Lakhani J, Bapna M, Mehta J. To identify morbidity and mortality predictors in acute organophosphate poisoning.Indian J Crit Care Med 2014;18(5):297-300. [PubMed] [Free full text] doi: 10.4103/0972-5229.132488.
- Aygun D, Doganay Z, Altintop L, Guven H, Onar M, Deniz T, et al. Serum acetylcholinesterase and prognosis of acute organophosphate poisoning.J Toxicol Clin Toxicol 2002;40:903–10. [PubMed]
- Singh J, Kapoor D, Singh M, Anand LK. Plasma cholinesterase levels in acute organophosphorus poisoning: a plausible marker for weaning? Anaesth Pain & Intensive Care 2016;20(4):477-479 [Free full text]
- Hiremath P, Rangappa P, Jacob I, Rao K. Pseudocholinesterase as a predictor of mortality and morbidity in organophosphorus poisoning.Indian J Crit Care Med 2016;20(10):601-604. [PubMed] [Free full text]
- Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning.Lancet 2008;371(9612):597-607. [PubMed] [Free full text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube