Ali Sarfraz Siddiqui*, Bushra Salim**, Safia Zafar Siddiqui***
*Assistant Professor; **Anesthesia Instructor
Department of Anesthesiology, Aga Khan University. Karachi (Pakistan)
***Associate Professor, Department of Anesthesiology, SICU & Pain Management, Civil Hospital Karachi.
Correspondence: Dr. Ali Sarfraz Siddiqui, Flat # L-7, Hassan Apartment, Block- 13-A, Gulshan-e-Iqbal, Karachi (Pakistan). Phone: 0333-2278913; E-mail: dr.alisarfraz@gmail.com
ABSTRACT
Background and objectives: Hypotension following spinal anesthesia (SA) for cesarean delivery can have important consequences for parturient and may affect neonatal outcome. The objective of this study was to compare intravenous bolus doses of phenylephrine and ephedrine to treat hypotension after SA for cesarean section and the effect of vasopressors on fetal outcome in terms of Apgar score.
Methodology: Two hundred parturient fulfilling inclusion criteria were randomly allocated into two groups of hundred each. Lumbar puncture was done in sitting position and 10 mg, 0.5% hyperbaric bupivacaine was given intra-thecally to every patient. All patients were placed supine with 15 degree left lateral tilt position. If hypotension occurred after SA (systolic blood pressure less than 90 mm Hg or decrease in systolic blood pressure more than 20% of base line whichever is lower) was treated with either 100µg phenylephrine in Group A or6 mg ephedrine in Group B boluses given intravenously.
Results: Single intravenous bolus dose of phenylephrine 100 µg was effective in treating hypotension in 92% parturient while ephedrine 6mg remained effective in 78% parturient, which was statistically significant (p= 0.0009). There was no difference in the mean Apgar scores (p = 0.76) at 1 minute and (p = 0.09) at 5 min between the two groups. Incidence of bradycardia (heart rate < 50 beats/mints.) was significantly higher in Group A as compared to Group B (p=0.038).
Conclusion: Intravenous bolus dose of phenylephrine 100 µg and ephedrine 6mg were both effective in treating hypotension after SA for elective cesarean section. Mean Apgar scores of the neonates at 1 and 5 min were comparable between the two groups.
Key words: Spinal anesthesia, cesarean section, hypotension, ephedrine and phenylephrine
Citation: Siddiqui AS, Salim B, Siddiqui SZ. Comparison of phenylephrine and ephedrine for treating hypotension after spinal anesthesia for cesarean section: A Randomized double-blind clinical trial. Anaesth Pain & Intensive Care 2015;19(1):44-49
INTRODUCTION
Maternal hypotension after regional anesthesia for cesarean delivery can have important consequences like nausea, vomiting, dizziness etc. that may affect neonatal outcome. Various methods have been used to prevent hypotension like pre-hydration, vasopressor drugs and lower leg compression but even then many parturient become hypotensive after spinal anesthesia and require treatment.1 Ephedrine is considered as the vasopressor of choice in obstetric anesthesia2 but studies showed that it is associated with less satisfying umbilical pH values than phenylephrine.3
Recent literature review showed that ephedrine and phenylephrine are both effective for the management of hypotension with no difference in neonatal Apgar scores and the incidence of fetal acidosis but phenylephrine was associated with higher neonatal umbilical arterial pH values.4,5
Primary objective of this study was to evaluate whether intravenous bolus dose of phenylephrine is more effective than ephedrine to treat hypotension after SA for elective cesarean section and the secondary objective was to see the effect of vasopressors on fetal outcome in terms of Apgar score.
METHODOLOGY
After obtaining the approval from the Institutional Ethics Committee and informed written consent, two hundred ASA physical status I and II females with singleton pregnancies, aged 18 to 35 years, height 150 to 170 cm and weight 55 to 75 kg, scheduled for elective and uncomplicated cesarean deliveries under SA were recruited in this randomized double-blind study. Women with pre-existing or pregnancy-induced hypertension, pre-eclampsia, diabetes mellitus, known cardiovascular or cerebrovascular disease, fetal abnormality, or contraindication to SA were excluded from the study. All patients were fasted for 6 to 8 hours prior to anesthesia and received aspiration prophylaxis preoperatively as intravenous ranitidine 50mg, metoclopramide 10mg and oral sodium citrate 30ml solution.
In the operating room all patients were placed supine with left uterine displacement and standard monitors like non-invasive BP (blood pressure), ECG and pulse oximeter were applied. Base line heart rate, systolic BP and diastolic BP were calculated as mean of three successive readings measured one minute apart. An 18 gauge I/V line taken and all patients were preloaded with 10 ml/kg lactated Ringer’s solution over 10 min then infusion rate was reduced to keep vein open. Lumbar puncture done in sitting position at L 3-4 interspace with 25 gauges Quincke needle. In every patient after confirming the free flow of CSF, 2ml of 0.5% hyperbaric bupivacaine with 25-µg fentanyl injected intrathecally. Patients were then immediately placed supine with 15 degree left lateral tilt position using wedge under right hip. All patients were given supplemental oxygen at 5 lit.min-1 via facemask. After SA heart rate, systolic and diastolic blood pressures were recorded at one-minute interval for first 10 min, at two min interval for next 10 min then at three minutes intervals until delivery of baby. Sensory block to T5 level was considered appropriate for surgery. After confirming the level of block to T5 by pinprick method, surgeons were asked to proceed for the surgery.
Hypotension was defined as systolic BP less than 90 mm Hg or decreases in systolic BP more than 20% of base line whichever is lower. Patients were randomly assigned to receive one of two vasopressor drugs whenever hypotension occurs. The Group-A patients received 1 ml (100µg) intravenous bolus of phenylephrine while Group-B patients received 1ml (6mg) intravenous bolus of ephedrine. In cases, where hypotension did not improve additional boluses of same vasopressor was given to keep systolic BP ≥90mmHg. All patients were randomized by computer generated number allocation using PASS software. The study drugs were prepared in similar 05 ml syringes and labeled A and B by primary anesthesiologist neither involved in patient management nor in the data collection. In case of bradycardia (heart rate < 50 beats/min), atropine 0.6 mg was given intravenously. Just after delivery of the baby, oxytocin 10 units were given over one minute followed by 20 units slow intravenous infusion.
Number of vasopressor doses, total dose of vasopressor required and use of atropine were recorded. Incidence of nausea and vomiting were also recorded. The Apgar scores of all neonates were noted at 1 min and 5 min after the delivery by a pediatrician, blinded to the group allocation. Baby caring nurse also recorded the birth weight of all the neonates.
Sample size of 100 patients in each group were selected to detect 15 to 20% difference in treating hypotension with single dose of vasopressor between groups, using a type I error of 0.05 and a power of 0.80 and this difference was based on our data from a pilot study. Categorical data such as ASA physical status and indication of cesarean section were analyzed with the chi-square test. Mean and standard deviation were computed for age, weight, height and Apgar score and analyzed by independent sample t-test, while primary outcome that is correcting hypotension was measured in proportion and percentage and analyzed by chi-square tests between the groups. A p-value ≤ 0.05 was accepted as statistically significant. All analyses were performed using SPSS version 19.0 (SPSS Ltd, Chicago, IL, USA).
RESULTS
Two hundred and ninety eight parturient scheduled for cesarean delivery, fulfilling the inclusion and exclusion criteria were enrolled in this study. Hypotension occurred in 67.11 % parturient. Ninety-eight parturient who did not develop hypotension were excluded from the study. So total of two hundred parturient were included in the study and divided into two groups of 100 patients in each group.
Demographic, clinical characteristics and indication of cesarean delivery are presented in Table 1. The two groups were comparable with respect to age, weight, ASA physical status and indication of cesarean delivery but a statistically significant difference existed in height of parturient (p= 0.033) between the groups. Sensory level of block was achieved up to T5 or above in all patients that were comparable in both groups.
Table 1: Demographics, clinical characteristics of parturient and indications of cesarean delivery
| Variables |
Group – A n =100 |
Group – B n =100 |
P-values |
| Age (years) |
26.88± 3.23 |
26.92± 4.45 |
0.94 |
| Weight (kg) |
63.10± 5.32 |
62.12± 4.16 |
0.146 |
| Height (cm) |
160.32± 3.97 |
159.38± 1.88 |
0.033 |
| ASA physical status | |||
| I | 61% | 69% |
0.23
|
| II |
39% |
31% |
|
| Indication of cesarean delivery | |||
| FTP CPD | 28% | 26% | 0.75 |
| Previous cesarean | 50% | 44% | 0.39 |
| Others |
22% |
30% |
0.19 |
ASA= American society of Anesthesiologist; FTP= Full term pregnancy;
CPD= Cephalopelvic disproportion
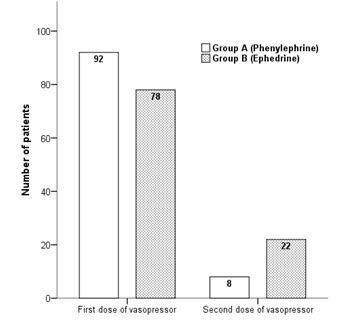
Ninety two percent parturient of Group A required single dose of 100 µg of phenylephrine while seventy eight percent parturient of Group B required 6 mg ephedrine to treat hypotension, which was statistically significant (p=0.0009). Eight percent patients in the Group A (phenylephrine) and twenty two percent patients in Group B (ephedrine) needed second dose of vasopressor to maintain systolic blood pressure as shown in Figure 1.
Figure 1: Comparison of intravenous bolus doses of vasopressors required to treat hypotension
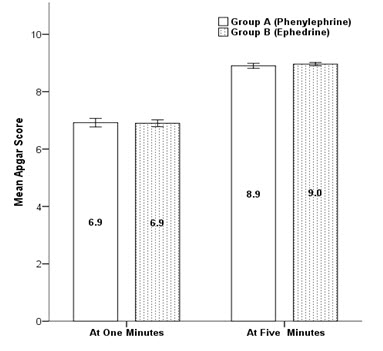
Mean Apgar scores were comparable between the groups, at 1 minute (p=0.76), and at 5 min (p= 0.09)(Figure 2).
Figure 2: Comparison of mean Apgar score between groups at 1 and 5 min
There was statistically significant difference exist in mean systolic blood pressure between group A and group B at three to seven and twelve minute time intervals, as presented in Figure 3.
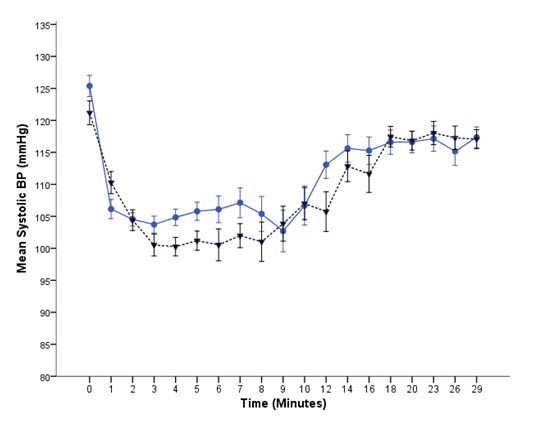
Figure 3: Comparison of mean systolic blood pressure between Group A () and Group B () with respect to time
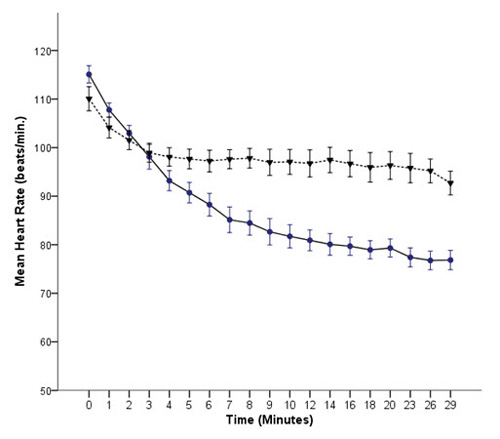
Figure 4: Comparison of mean heart rate between Group A (●) and Group B (♥) with respect to time
Complications like bradycardia, nausea and vomiting were also recorded. Incidence of bradycardia (heart rate < 50 beats/mints) was significantly higher in Group A (15%) as compared to Group B (6%) (p=0.038). Comparison of mean heart rate between Group A and Group B with respect to time is presented in Figure 4. Incidence of nausea and vomiting were relatively higher in Group A as compared to Group B but were not statistically significant (p=0.56 and p=0.72 respectively) No parturient developed oxygen desaturation, SPO2 < 95%. Mean Birth Weight (in kilogram) of neonates of Group A was 2.67± 0.19 and Group B was 2.64 ± 0.18 which were comparable.
DISCUSSION
Maternal hypotension is the most common and important physiological response to SA due to preganglionic sympathetic block with important maternal and fetal consequences. In literature overall incidence of hypotension during SA for cesarean section is 80% but in this study it was 67%. Traditionally, non-pharmacological interventions such as leg elevation, compressive leg devices, left uterine displacement and intravenous fluid preloading have been used but vasopressors are often required.6,7
Ephedrine and phenylephrine have been used for the treatment of intra-operative hypotension in many studies. Ephedrine is effective in the treatment of spinal induced hypotension during cesarean sections, but it can cause fetal acidosis.8,9 Updated meta-analysis by Lin FQ et al. showed comparable results between prophylactic ephedrine and phenylephrine to manage spinal-induced hypotension but parturient treated with phenylephrine had neonates with higher umbilical pH value than those treated with ephedrine.10
Ephedrine is a mixed α and β agonist and causes increase in cardiac output and heart rate. Ephedrine crosses placenta and causes increase in oxygen consumption and increase in glucose and lactic acid concentrations. Phenylephrine is a pure α1 adrenergic agonist, which increases systemic vascular resistance and causes reflex bradycardia but it maintain cardiac output in healthy parturient.11
Ngankee WD et al. showed that overall phenylephrine has beneficial effects on fetal oxygen supply and demand balance. It crosses the placenta to a lesser extent than ephedrine.12 Dyer et al. showed that maternal cardiac output is decreased with bolus phenylephrine in comparison to ephedrine but phenylephrine was effective in obtunding the hemodynamic changes in response to oxytocin.13 Doherty et al. compared phenylephrine infusion with the bolus regimens during cesarean section under SA and found that both regimens maintained maternal arterial blood pressures closer to baseline but the infusion regimen required a higher total dose.14
In this study intravenous bolus doses of phenylephrine and ephedrine were used and both were effective in treating hypotension after SA, however, less bolus doses of phenylephrine were required. Gunda et al. compared the effectiveness and the side effects of ephedrine and phenylephrine administered for treating hypotension during elective cesarean section under SA and found that both are effective in treating hypotension. They suggested that phenylephrine may be more appropriate vasopressor when considering maternal wellbeing.15
Meta-analysis done by Veeser et al. demonstrated a decreased risk of fetal acidosis with phenylephrine.16 Prakash et al.showed that both phenylephrine 100 µg and ephedrine 6 mg were comparable in the management of hypotension during SA for elective cesarean section. Neonates in the phenylephrine group had significantly higher umbilical arterial pH and base excess values than the ephedrine group.17
Adigun TA et al. showed that phenylephrine is safe and comparable to ephedrine.18 Cooper et al. showed that the umbilical artery pH was similar whether ephedrine or phenylephrine was used to maintain the maternal arterial pressure during intra-thecal anesthesia in high risk cases due to fetal compromise.19
Nazir et al. showed that phenylephrine and ephedrine are equally effective in treating hypotension during SA for elective cesarean section. Neonatal outcome and Apgar score were comparable in both the groups.20 In our study mean Apgar scores of the neonates at 1 minute (p = 0.76) and at 5 min (p = 0.09) were comparable between phenylephrine and ephedrine groups. Ashraf S. Habib in his review showed a lower incidence of intraoperative nausea and vomiting and higher umbilical artery pH and base excess compared with ephedrine.21
Apgar score is the most commonly applied and easily interpretable clinical method of neonatal wellbeing and in literature. A recent meta-analysis of vasopressor choice during regional anesthesia in obstetric showed phenylephrine and ephedrine are comparable in terms of neonatal Apgar score at one and five minutes after delivery.22
This study has number of limitations for instance only uncomplicated and elective cesarean deliveries were included in the study but in complicated and emergency cases response of vasopressors may be different. The umbilical artery blood gases were not analyzed because of two reasons; one is financial reason and other is well-documented evidence of the effects of vasopressor (phenylephrine and ephedrine) on umbilical artery pH. Intravenous bolus dose of phenylephrine 100 µg and ephedrine 6mg were taken based on literature and our pilot study.
CONCLUSION
Intravenous bolus doses of phenylephrine 100 µg and ephedrine 6 mg were both effective in treating hypotension after SA for elective cesarean section. Phenylephrine was comparatively more effective because less bolus doses were required to treat hypotension than ephedrine. Mean Apgar scores of the neonates at 1 and 5 min were comparable between the two groups.
Conflict of interest: None declared. The study was conducted purely on hospital resources and no external funding was involved.
REFERENCES
- Cyna AM, Andrew M, Emmett RS, Middleton P, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev 2006;18:CD002251. [PubMed] [Free full text]
- Burns SM, Cowan CM, Wilkes RG. Prevention and management of hypotension during spinal anaesthesia for elective caesarean section: A survey of practice. Anaesthesia 2001;56:777–798. [PubMed]
- Cooper DW, Carpenter M, Mowbray P, Desira WR, Ryall DM, Kokri MS. Fetal and maternal effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery. Anesthesiology 2002;97:1582–1590. [PubMed]
- Lee A, NganKee WD, Gin T. A quantitative, systematic review of randomized controlled trials of ephedrine versus phenylephrine for the management of hypotension during spinal anesthesia for cesarean delivery. Anesth Analg 2002;94:920–926. [PubMed]
- Macarthur A, Riley ET. Obstetric anesthesia controversies: Vasopressor choice for postspinal hypotension during cesarean delivery. Int Anesthesiol Clin 2007;45:115–132. [PubMed]
- Kubli M, Shennan AH, Seed PT, O’Sullivan G. A randomized controlled trial of fluid preloading before low dose epidural analgesia for labour. Int J Obstet Anesth 2003;12:256-260. [PubMed] [Free full text]
- Erler I, Gogarten W. Prevention and treatment of hypotension during caesarean delivery. Anasthesiol Intensivemed Notfallmed Schmerzther 2007;42:208-13. [PubMed]
- NganKee WD, Khaw KS, Ng FF. Prevention of hypotension during spinal anesthesia for cesarean delivery: an effective technique using combination phenylephrine infusion and crystalloid cohydration. Anesthesiology, 2005;103:744-750. [PubMed]
- Lee A, NganKee WD, Gin T. A dose-response meta-analysis of prophylactic intravenous ephedrine for the prevention of hypotension during spinal anesthesia for elective cesarean delivery. Anesth Analg, 2004;98:483-490. [PubMed]
- Lin FQ, Qiu MT, Ding XX, Fu SK, Li Q. Ephedrine versus Phenylephrine for the Management of Hypotension during Spinal Anesthesia for Cesarean Section: An Updated Meta-Analysis. CNS Neurosci Ther 2012;18:591–597. [PubMed] [Free full text]
- Cooper DW. Caesarean delivery vasopressor management. Curr Opin Anaesthesiol 2012;25:300–308. [PubMed]
- Ngan Kee WD, Khaw KS, Tan PE, Ng FF, Karmakar MK. Placental Transfer and Fetal Metabolic Effects of Phenylephrine and Ephedrine during Spinal Anesthesia for Cesarean Delivery. Anesthesiology 2009;111:506–12. [PubMed] [Free full text]
- Dyer RA, Reed AR, Van Dyk D, Arcache MJ, Hodges O, Lombard CJ, et al. Hemodynamic effects of ephedrine, phenylephrine, and the coadministration of phenylephrine with oxytocin during spinal anesthesia for elective cesarean delivery. Anaesthesiology 2009;111:753-765. [PubMed] [Free full text]
- Doherety A, Ohashi Y, Downey K, Carvalho JCA. Phenylephrine Infusion Versus Bolus Regimens During Cesarean Delivery Under Spinal Anesthesia: A Double-Blind Randomized Clinical Trial to Assess Hemodynamic Changes. Anesth Analg 2012;115:1343–1350. [PubMed]
- Gunda CP, Malinowski J, Tegginmath A, Suryanarayana VG, Chandra SB. Vasopressor choice for hypotension in elective Cesarean section: ephedrine or phenylephrine? Arch Med Sci 2010;6:257-263. [PubMed] [Free full text]
- Veeser M, Hofmann T, Roth R, Klöhr S, Rossaint R, Heesen M. Vasopressors for the management of hypotension afterspinal anesthesia for elective caesarean section. Systematicreview and cumulative meta-analysis. Acta Anaesthesiol Scand 2012;56:810–6. [PubMed] [Free full text]
- Prakash S, Pramanik V, Chellani H, Salhan S, Gogia AR. Maternal and neonatal effects of bolus administration of ephedrine and phenylephrine during spinal anaesthesia for caesarean delivery: A randomized study. Int J Obstet Anesth 2010;19:24–30. [PubMed] [Free full text]
- Adigun TA, Amanor-Boadu SD, Soyannwo SD. Comparison of intravenous ephedrine with phenylephrine for the maintenance of arterial blood pressure during elective caesarean section under spinal anaesthesia. Afr J Med MedSci 2010;39:13-20. [PubMed]
- Cooper DW, Sharma S, Orakkan P. Retrospective study of association between choice of vasopressor given during spinal anaesthesia for high-risk caesarean delivery and fetal pH. Int J Obstet Anesth 2010;19:44-49. [PubMed] [Free full text]
- Nazir I, Bhat MA, Qazi S, Buchh VN, Gurcoo SA. Comparison between phenylephrine and ephedrine in preventing hypotension during spinal anesthesia for cesarian section. J Obs Anesth & Critical Care 2012;2:92-97. [Free full text]
- Habib AS. A review of the impact of phenylephrine administration on maternal hemodynamics and maternal and neonatal outcomes in women undergoing cesarean delivery under spinal anesthesia. Anesth Analg 2012;114:377-390. [PubMed]
- Biddle C. To press or not to press, and if so, with what? A single question-focused meta-analysis of vasopressor choice during regional anesthesia in obstetrics. AANA J. 2013;81:261-264. [PubMed]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube