Chhavi S. Sharma, DA, DNB, MNAMS*, Manpreet Singh MD, FIMSA, FACEE, FCCP, MAMS**, Rajesh S. Rautela, MD***, Anjali Kochhar, MD****, Nandita Adlakha, MD*
*Specialist; ***Director Professor, Department of Anesthesiology & Critical Care, UCMS & GTB Hospital, Dilshad Garden, Delhi-110095 (India)
**Assistant Professor, Department of Anesthesiology & Intensive Care, Govt. Medical College & Hospital, Sector 32, Chandigarh (India)
****Associate Professor, Department of Anesthesiology, Hamdard Institute of Medical Sciences & Research, Delhi (India)
Correspondence: Dr Manpreet Singh, Department of Anesthesiology and Intensive Care,
Govt. Medical College & Hospital, Sector 32, Chandigarh (India); Phone: +919646121503;E-mail: manpreetdawar@gmail.com
ABSTRACT
Background: Patients experience considerable pain during the first 24 hours after laparoscopic surgeries in spite of great progress in pain relief methods. Intraperitoneal local anesthetics in different doses have been used effectively to reduce this pain.The present study was conducted to compare whether moderate dose (75 mg) intraperitoneal and peri-portal bupivacaine or ropivacaine can produce effective pain relief after laparoscopic cholecystectomy.
Material and Methods: Eighty ASA I and II female patients undergoing laparoscopic cholecystectomy under general anesthesia were included in the study and were assigned to either of the two groups in a double blind randomized manner, Group B and Group R. At the end of the surgery, patients in Group B received 20 ml of 0.25% bupivacaine intraperitoneally and 10 ml was infiltrated in periportal area. Patients in Group R received 20 ml of inj. ropivacaine 0.25% intraperitoneally and 10 ml was infiltrated in periportal areas. Visual analogue score for pain and vital signs were recorded for 24 hours in the postoperative period. Injection of tramadol was administered as rescue analgesic. Total analgesic consumption in 24 hours and side effects were recorded.
Results: Statistically significant difference (p<0.05) was found in pain intensity (visceral and parietal pain) within groups during the first 4-6 hrs in the postoperative period. The total number of rescue analgesic doses were similar in both groups and statistically insignificant. Variables of post operative recovery were similar in both groups.
Conclusion: Moderate dose intraperitoneal analgesia with local anesthetic (ropivacaine and bupivacaine) is simple to use and effective method with minimal side effects.
Key words: Laparoscopic cholecystectomy; Intraperitoneal; Bupivacaine; Ropivacaine
Citation:Sharma CS, Singh M, Rautela RS, Kochhar A, Adlakha N. Comparison of intraperitoneal and periportal bupivacaine and ropivacaine for postoperative pain relief in laparoscopic cholecystectomy: a randomized prospective study. Anaesth Pain & Intensive Care 2014;18(4):350-54
INTRODUCTION
Laparoscopic cholecystectomy is the preferred surgical technique for uncomplicated cholecystectomy. Severity of postoperative pain and opioid consumption is less with better pulmonary function in laparoscopic procedures compared with open cholecystectomy.1,2
Although post-operative pain is less intense as compared to open procedure, patients often complain of considerable pain in the first 24 hours.Post-operative nausea, vomiting and pain are two of the common complications seen after ambulatory laparoscopic cholecystectomy.3
After laparoscopic surgery, visceral pain is experienced due to stretching of intraperitoneal cavity, peritoneal inflammation and phrenic nerve irritation, whereas in open procedures pain is mainly somatic in nature.
Many methods have been used to decrease post-operative pain including NSAID’s, opioids and intraperitoneal local anesthetics with variable success. A combined approach using intra-peritoneal and peri-portal infiltration of local anesthetic solution may be more beneficial than intra-peritoneal infiltration alone. A literature search revealed limited studies examining the combined effect of somato-visceral blockade for pain relief during laparoscopic cholecytectomy.4Significant analgesic effect with a large dose of intra-peritoneal buupivacaine (150 mg) has been described.5,6
Ropivacaine, an amide local anesthetic, has similar efficacy to bupivacaine with reduced systemic and cardiac toxicity.7
The aim of this study was to compare whether moderate dose (75 mg) intraperitoneal and peri-portal bupivacaine and ropivacaine can produce effective pain relief after laparoscopic cholecystectomy and to record analgesic consumption and minor morbidities after administration of moderate dose in post-operative period up to 24 hours.
METHODOLOGY
This prospective randomized double blind study was conducted after hospital ethical committee approval and written informed consent from all the patients. The study group included 80 ASA I and II female patients between the ages of 20-60 years undergoing laparoscopic cholecystectomy under general anesthesia. Patients with acute cholecystitis, allergy to local anesthetics or opioids, previous history of opioid intake, morbid obesity and surgery converted to open procedure were excluded from the study.
Anesthetic technique: Patients were premedicated with 0.5 mg alprazolam at night and 0.5 mg on the morning of surgery orally. Anesthesia was induced with inj. propofol 1.5–2 mg/kg IV and intubation achieved with inj.vecuronium 0.08 mg/kg. Anesthesia was maintained with O2, N2O (60:40), 1% isoflurane and intermittent doses of vecuronium guided by peripheral nerve stimulator. For intra-operative analgesia inj. morphine sulphate 0.15 mg/kg was used. Standard patient monitoring was performed. Ventilation was adjusted to maintain end-tidal CO2 between 35-40 mm of Hg and intra-abdominal pressure was kept between 10-12 mmHg. Injection diclofenac sodium 1.5 mg/kg IM was given at the end of surgery as a part of multimodal approach for post-operative pain.
At the end of procedure, intra-abdominal CO2 was carefully vented out by the operating surgeon and the patients were randomly assigned to one of the following groups;
- Group R (Ropivacaine, n=40): 30 ml of 0.25% ropivacaine
- Group B (Bupivacaine, n=40): 30 ml of 0.25% bupivacaine
Randomization was done with computer generated random number tables and closed envelope technique. In this technique the chits were kept with the number and then the group was chosen accordingly. The surgeon performing the surgery was blinded to the drug solution.
A 20 ml of test solution was sprayed on the upper surface of liver and on right sub-diaphragmatic space and 10 ml was injected into site of incision and in all portals at the end of the surgery with the patient in Trendelenberg position. Postoperatively, patients were assessed for parietal pain (defined as superficial pain located on abdominal wall) and visceral pain (defined as deep, dull, more difficult to localize, inside the abdomen) using a 10 cm VAS. Time to first rescue analgesia, number of analgesic doses, sedation, nausea and vomiting, dizziness, backache and urinary retention were also assessed at 30 min and at 1, 2, 3, 4, 6, 8,12 and 24 hours. Blood pressure, heart rate and respiratory rate were assessed at 0, 30, 60 and 120 min. Rescue analgesia consisted of an injection of tramadol 100 mg intravenous (slow) if the VAS score was more than 4.
Statistical analysis: Power analysis was done with pain score as primary criterion. Standardized difference of 1.5 (VAS) was calculated, which gave a sample size of 80, i.e. 40 patients in each group (assuming a power of 80% and a significance level of 0.05).
Data analysis was done using unpaired t-test for continuous variables (age, duration, intra-abdominal pressure).Two factor repeated measure ANOVA was used for comparing VAS score. One factor time as a repeated and second factor group was taken as a fixed factor. Mauchly’s test for sphericity was done to find correlation across the time points. If significant HUYN-FELDT (epsilon) correction was done.
RESULTS
A total of eighty patients were included in the study. No difference was found in age (36.9 ± 12.3 yr vs. 34.6 ± 12.5 yr), duration of surgery (1.42 ± 0.51 hrs vs. 1.24 ± 0.53 hrs) and IAP (11.6 ± 0.74 vs. 11.3 ± 0.80) between Group R and Group B (p>0.05). Hemodynamic variables were comparable in both the groups (Figures 1-3).
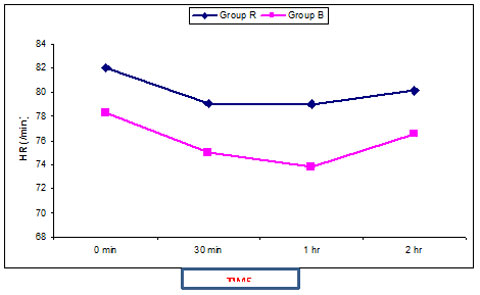
Figure 1: Comparison of heart rate changes
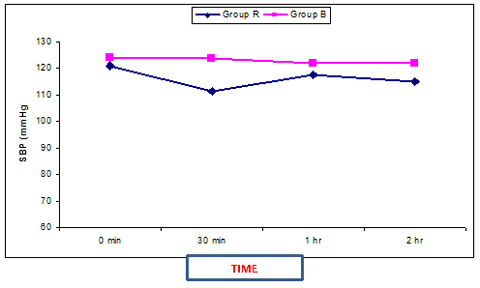
Figure 2: Comparison of systolic blood pressure with time
Figure 3: Changes in oxygen saturation with time
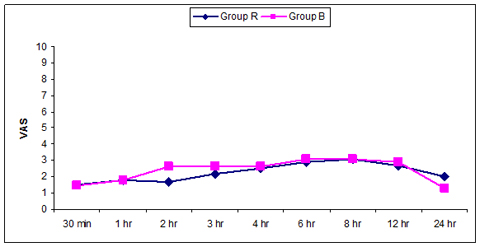
Figure 4: VAS scoring of somatic pain
*Significant at p<0.05, interaction between group and time is significant (p<0.05)
Sphericity assumption is validated, hence (VAS & group) H & F correction was done
Figure 5: VAS scoring in visceral pain
*Significant at p<0.05, interaction between group and time is significant (p<0.05)
Sphericity assumption is validated, hence (VAS & group) H & F correction was done
Mean VAS score for parietal pain (Figure 4) at 4 hrs was1.6 ± 1.5 versus 1.7 ± 1.2 in Group R and B respectively. Mean VAS score for visceral pain (Figure 5) at 4 hrs was 2.5 ± 1.4 versus 2.6 ± 1.1 in Group R and B respectively. Statistically significant difference (p<0.05) was found in pain intensity of the visceral and parietal pain within the groups during first 4-6 hrs in the postoperative period but there was no statistically significant difference (p>0.05) between the two groups.
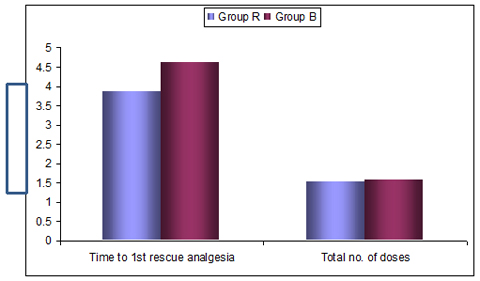
Time to first rescue analgesia was 3.85 ± 3.7 versus 4.6 ± 3.7 in Group R and B respectively and the total number of rescue analgesic doses were similar in both the groups and statistically non-significant (Figure 6).
Figure 6: Comparison of time to first rescue analgesia and total doses required
Variables of post operative recovery were similar in both the groups. There was no systemic toxic reaction to local anesthetic in any of the patients. Incidence of nausea and vomiting was 15-20% in both the groups, incidence of other minor morbidities were similar in both the groups.
DISCUSSION
Early pain after laparoscopic cholecystectomy is multifactororial, secondary to different pain mechanisms including abdominal wall trauma, abdominal distension and pneumoperitoneum using CO2.4,8 It has three components:visceral, parietal and shoulder tip pain. Bisguard et al4 and Ure et al9 have suggested that predominant type of pain in these patients is parietal pain, however, some authors have differed from this opinion.10,11 Visceral and shoulder tip pain can be blocked by intraperitoneal instillation and parietal pain requires portside infiltration.
Intraperitoneal injection of local anesthetic after gynecologic laparoscopy has proved to be effective.12 Similar technique for pain relief after laparoscopic cholecystectomy has shown conflicting results as there are several factors that can influence the benefits of intraperitoneal analgesia. These factors are dose and concentration,site of instillation (sub-diaphragmatic versus sub-hepatic) and timing of instillation (before or after) of the anesthetic solution, volume of residual CO2, spillage of bile and blood,instillation in head-down position versus supine position and postoperative analgesia regimen.12
Initial studies used smaller doses of local anesthetic, in contrast, two studies have used large doses of intra-peritoneal bupivacaine and shown it to be effective.8,10Study by Mraovic et al5 and Pasqualucci et al6 have both described significant analgesic effect with a large dose of bupivacaine (150 mg).
Various other studies have demonstrated effectiveness of ropivacaine in reducing pain after laparoscopic cholecystectomy. Gupta et al demonstrated effectiveness of intermittent injections of ropivacaine 0.5% using a catheter in the gall bladder bed in reducing early post-operative visceral pain and pain on coughing in the initial few hours.1
Bucciero et al used either instillation of ropivacaine 0.5%, 20 ml (150 mg) after induction of the pneumoperitoneum, or nebulization of ropivacaine 1%, 3 ml before and after surgery. There were no differences between both the groups in pain scores or in analgesic consumption.They concluded that 1% ropivacaine nebulisation was more effective for reducing shoulder pain. Intra-peritoneal nebulisation provides a uniform spread of local anesthetic throughout the peritoneal cavity and thus is more beneficial.13
Kucukc et al14 did a comparative study using intra-peritoneal bupivacaine (100mg) and ropivacaine (100 mg, 150 mg) and found ropivacaine (150mg) to be more effective than bupivacaine (100mg) and ropivacaine (100 mg).
Evidence for potency of ropivacaine compared with bupivacaine is clear cut with several minimum local analgesic concentration studies3,8,10 demonstrating that ropivacaine has 60% of potency of bupivacaine. Mraovic et al4 assessed the analgesic efficacy of ropivacaine ranging from 37.5 to 150 mg infiltrated into the wound at time of inguinal hernia repair. This study as well as others have used even larger dose after inguinal hernia suggesting a ceiling effect at 100 mg of ropivacaine. Indeed 100 mg of ropivacaine or 300-375 mg does not produced analgesic efficacy superior to 75 mg.5
In the present study either 75 mg of bupivacaine or ropivacaine were equally effective as the concentration used was 0.25% and the test solution was sprayed on the upper surface of liver, on right sub-diaphragmatic space, into site of incision and in all portals at the end of surgery in the Trendelenberg position. Incidence of shoulder pain was low as intra-abdominal CO2 was carefully vented out by the surgeon. A decreased incidence of shoulder pain at rest was seen in ropivacaine group but the difference was not statistically significant.
One of the limitations with our study was that we did not measure plasma concentration of local anesthetics after Intra-peritoneal injection. Several reports have shown that range of mean plasma concentration (0.92-1.14 µg/ml) after intra peritoneal administration of plain bupivacaine (100-150 mg) was well below toxic concentration of 3 ug/ml.5 With maximum increased dose a concentration of more than 4 µg/ml has been reported (considered as limit of potential toxicity).15 With Intraperitoneal ropivacaine (100-300 mg) a mean plasma concentration was 0.66-3.76 µg/ml which again was well below the toxic range.Several studies have evaluated doses of ropivacaine as large as 300-375 mg for inguinal hernia or intraperitoneal instillation with no clinical evidence of toxicity.6 Scott et al17 and Kundsen et al6 demonstrated a large tolerated CNS dose for ropivacaine (124 and115 mg respectively) than for bupivacaine (99 and 103 mg respectively).
Although intraperitoneal injection of local anesthetics is effective in the initial few hours, a multimodal approach can be used for pain relief after laparoscopic cholecystectomy.
From present study it is concluded that moderate dose of intraperitoneal and periportal analgesia with both ropivacaine and bupivacaine was, effective simple to use and with less side effects and can berecommended in patients undergoing laparoscopic cholecystectomy.
Funding: Authors declare no funding from any source for conducting this study
Conflict of interest: No conflict of interest declared by any of the authors
REFERENCES
- Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D.. Laparoscopic versus open cholecystectomy: hospitalization, sick leave, analgesia and trauma responses. Br J Surg 1994;81:1362–5. [PubMed]
- Saunders CJ, Leary BF, Wolfe BM. Is outpatient laparoscopic cholecystectomy wise? Surg Endosc 1995;9:1263–8. [PubMed]
- Gupta A1, Thörn SE, Axelsson K, Larsson LG, Agren G, Holmström B et al. Postoperative pain relief using intermittent injections of 0.5% ropivacaine through a catheter after laparoscopic cholecystectomy. Anaesth Analg 2002;95:450-6. [PubMed]
- Bisgaard T, Kehlet H, Rosenberg J. Pain and convalescence after laparoscopic cholecystectomy. Eur J Anaesthesiol 2001;167:84–96. [PubMed]
- Mraovic B, Majeric-Kohler V. Pain after laparoscopic cholecystectomy. Br J Anaesth 1998;80:406-7. [PubMed][Free Full Text]
- Pasqualucci A1, de Angelis V, Contardo R, Colò F, Terrosu G, Donini A et al. Preemptive analgesia:intrapetitoneal local anesthetic in laparoscopic cholecystectomy: a randomized, double-blind, placebo-controlled study. Anesthesiology 1996;85:11-20. [PubMed]
- Knudsen K, Beckman Suurküla M, Blomberg S, Sjövall J, Edvardsson N.. Central nervous and cardiovascular effects of i.v. infusions of ropivacaine, bupivacaine and placebo in volunteers. Br J Anaesth 1997;78:507–14. [PubMed][Free Full Text]
- Scheinin B, Kellokumpu I, Lindgren L, Haglund C, Rosenberg PH.. Effect of intraperitoneal bupivacaine on pain after laparoscopic cholecystectomy. Acta Anaesthesiol Scand 1995;39:195-8. [PubMed]
- Ure BM, Troidl H, Spangenberger W, Dietrich A, Lefering R, Neugebauer E. Pain after laparoscopic cholecystectomy: intensity and localization of pain and analysis of predictors in preoperative symptoms and intraoperative events. Surg Endosc 1994;8:90–6. [PubMed]
- Alexander DJ, Ngoi SS, Lee L, So J, Mak K, Chan S, Goh PM.Randomized trial of periportal peritoneal bupivacaine for pain relief after laparoscopic cholecystectomy. Br J Surg 1996;83:1223-5. [PubMed]
- Rawal N, Axelsson K, Hylander J, Allvin R, Amilon A, Lidegran G et al. Postoperative patient-controlled local anesthetic administration at home. Anesth Analg 1998;86:86–9. [PubMed]
- Boddy AP, Mehta S, Rhodes M. The effect of intra-peritoneal local anaesthesia in laparoscopic cholecystectomy: A systematic review and meta-analysis. Anesth Analg 2006 ;103:682-8. [PubMed]
- Bucciero M1, Ingelmo PM, Fumagalli R, Noll E, Garbagnati A, Somaini M et al. Intraperitoneal Ropivacaine Nebulization for Pain Management After Laparoscopic Cholecystectomy: A Comparison with Intraperitoneal Instillation. Aneath Analg 2011;113:1266-71. [PubMed]
- Kucuk C, Kadiogullari N, Canoler O, Savli S. A placebo-controlled comparison of bupivacaine and ropivacaine instillation for preventing postoperative pain after laparoscopic cholecystectomy. Surg Today 2007;37:396-400. [PubMed]
- Narchi P,Benhamou D, Fernandez H. Intra-peritoneal local anaesthetic solution for shoulder pain after day case laproscopy. Lancet 1991;338:1569-70. [PubMed]
- Axelsson K, Nordenson U, Johanzon E, Rawal N, Ekbäck G, Lidegran G et al. Patient controlled regional anesthesia (PCRA) with ropivacaine after arthroscopic acromial decompression (ASD). Reg Anesth Pain Med 2001;26:S127. [PubMed]
- Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R.. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesth Analg 1989;69:563–9. [PubMed]






 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube