Yogita Dwivedi, MD1, Amrita Gupta2, Uma Srivastava3, Keshav Dev Jagar4, Atiharsh Mohan2, Sandeep Mangla4
1Assistant Professor; 2Lecturer; 3Professor; 4Senior Resident
Sarojini Naidu Medical College, Mahatma Gandhi Road, Agra, Uttar Pradesh, (India)
Correspondence: Dr. Amrita Gupta, Lecturer, Sarojini Naidu Medical College, Mahatma Gandhi Road, Agra, Uttar Pradesh, (India); Mob: 09837077784; E-mail: amritagupta78@gmail.com
ABSTRACT
Introduction: LMA Proseal™ is considered the premier supraglottic airway device in children. I-gel circumvents the cuff related problems of second generation devices as its seal is made of thermoplastic elastomer. Its potential advantages include easy insertion, minimal tissue compression and good stability. We planned this study to assess the clinical performance of i-gel, LMA Proseal™ and LMA classic in children breathing spontaneously.
Methodology: 90 patients of ASA grade I and II, weighing between 10-25 kg, posted for elective surgery with a duration of less than 2 hrs, were randomly divided into three groups (30 each). Standard general anesthesia was administered to all children. Ease of insertion of the device and nasogastric tube, oropharyngeal seal pressure, hemodynamic parameters and intra- and postoperative complications were noted.
Results: The patients were comparable with respect to demographic data. Insertion was assessed as very easy in all three groups. Success rate of insertion in first attempt was >90% in each group. I-gel showed shortest mean time for insertion (16 ± 4 seconds). I-gel had highest seal pressure (25.2 ± 2.8). followed by LMA Proseal™ (22.6 ± 2.8) and Classic LMA (16.8 ± 2.6).
Conclusion: I-gel is comparable to LMA Proseal™ and Classic LMA in clinical performance. I-gel had highest oropharyngeal seal pressure and required least time for insertion. Therefore, it can be reliably used in pediatric anesthesia.
Key words: Supraglottic devices; Anesthesia, Pediatric; Ventilation; Airway; Airway management
Citation: Dwivedi Y, Gupta A, Srivastava U, Jagar KD, Mohan A, Mangla S. Comparison of i-gel™, LMA Proseal™ and LMA Classic™ in spontaneously breathing pediatric patients. Anaesth Pain & Intensive Care 2016;20(2):176-181
Received: 4 March 2016; Reviewed: 12, 30 March 2016; Corrected: 31 March, 6 June 2016; Accepted: 6 June 2016
INTRODUCTION
Introduction of new supraglottic devices (SGD’s) has changed the era of airway management in children due to ease of insertion, easy learning curve and ease to ventilate at peak airway pressure without gastric distention. Previous randomised studies1,2 have established the safety of Proseal LMA (PLMA) in children. It is now considered premier SGD in children and has set a bench mark in second generation devices. I-gel circumvents the cuff related problems of above devices as its anatomic seal is made of thermoplastic elastomer. The airway seal improves as it slowly adapts to the temperature of body. Its elliptical shape minimise axial rotation and improves stability.3,4,5 Despite its advantages there are a few studies comparing Classic LMA (CLMA) and PLMA with i-gel in children.
The aim of our study was to compare the clinical performance between CLMA, PLMA Proseal and i-gel in spontaneously ventilating children. Our primary objective was to compare oropharyngeal seal pressure and secondary objective was to compare insertion parameters, mean duration of insertion, gastric tube placement and haemodynamic parameters.
MATERIAL AND METHODS
After approval from the hospital proforma committee and obtaining written and informed consent from patients,90 patients with ASA grade 1 and 2 weighing between 10-25 kg were included in this randomized prospective study to compare i-gel, PLMA and CLMA in spontaneously breathing children undergoing elective surgery of less than 2 hours duration (colostomy closure, herniotomy, circumcision, cataracts, upper and lower limb surgeries etc.) performed under general anesthesia in our department during the time period of January 2013 to August 2014.
Patients with irritable upper respiratory tract, risk of aspiration, trismus, limited mouth opening, were excluded from the study. Ninety patients were divided randomly into one of the three groups of 30 each by concealed chits. (Groups C, P and I)
A standard anesthesia protocol was followed for every case. All the children were kept nil per orally before surgery. After shifting the patient to operation theatre, standard monitors pulse oximeter, non-invasive blood pressure, 5 lead Electrocardiogram, EtCO2 was applied and baseline parameters was recorded. Patients were premedicated with inj glycopyrrolate 0.005 mg/kg, fentanyl 1-2 µg/kg and inj ondansetron 0.08 mg/kg before induction.
Anesthesia was induced with propofol 3 mg/kg IV along with sevoflurane in oxygen. Once an adequate depth of anesthesia was achieved, judged by loss of verbal contact, jaw relaxation and absence of movement on jaw thrust, the SGD was inserted with the standard routine technique (introducer for PLMA, single finger technique for CLMA and i-gel). PLMA of size 1.5 and 2 were used for patients weighing 5-10 and 10-20 kg respectively. I-gel size 1.5, 2 or 2.5 was used for patients weighing 5-12, 10-25 and 25-35 kg respectively. The device was inserted in sniffing position or a combination of maneuvers such as chin lift, jaw thrust, head extension and neck flexion as required. All the insertions were done by anesthesiologist with minimum one year of experience and who had inserted each of the device more than 25 times earlier. Insertion of device was recorded as very easy: when assistant help was not required), easy: when jaw thrust was needed by assistant, and difficult: when jaw thrust and deep rotation or second attempt was used for proper device insertion.
Once inserted into the pharynx, the cuff was inflated with air until effective ventilation was established or the maximum recommended inflation volume reached (60 cmH2O). Fixation of the devices was done according to the manufacturer’s instructions. Effective ventilation was judged by observation of chest wall movement, auscultation of bilateral breath sound and a square wave capnography trace. Anesthesia was maintained with 1-2% sevoflurane and 70% nitrous oxide in oxygen. Insertion time was noted from the time of picking of device and time to achievement of adequate airway as judged by adequate chest expansion, auscultation of bilateral breath sound and a square wave capnography trace. Number of insertion attempts was noted. Three attempts were allowed before insertion was considered a failure. If insertion failed, alternative device was used.
Once insertion was successful, the intra-cuff pressure was set at 60 cmH2O (for CLMA and PLMA) using a digital manometer (Mallinckrodt Medical, Ireland). This pressure was maintained throughout the surgery by regular cuff pressure monitoring. The oropharyngeal leak pressure was determined by closing the expiratory valve of the breathing system at a fixed gas flow of 3 lit/min and noting the airway pressure at which equilibrium was reached (maximum allowed, 40 cm H2O). At this point gas leak was heard from mouth, epigastrium. Manometric test was considered the most reliable test.
Any episodes of desaturation, coughing, bronchospasm or aspiration / regurgitation/ vomiting were documented. At the end of the procedure, the SGD was inspected for any blood stains, tongue-lip-dental trauma. Postoperative sore throat was noted.
The following hemodynamic parameters were recorded in all patients; heart rate (HR), mean arterial pressure (MAP) in mmHg, pulse oxygen saturation (SpO2) and EtCO2. Insertion of a nasogastric tube Fr 8-10 was attempted through the gastric port of PLMA and i-gel, before the commencement of surgery. Correct gastric tube placement was assessed by suction of fluid or detection of injected air by epigastric stethoscope. Three attempts were made before gastric tube insertion was considered a failure.
Statistical analysis; Statistical analysis was done, using SPSS software. To calculate sample size oropharyngeal sealing pressure was considered the primary variable with Type one error .05 and power of 0.8 considering a projected difference of 30% between the three groups. ANOVA test was used for demographic data (age, weight), oropharyngeal seal pressure (OSP) and hemodynamic data analysis. The insertion characteristics and complications were analyzed using Chi square test. Fischers test was used to analyze insertion attempts of gastric tube.
RESULTS
There was no statistical difference in demographic data between groups (Table I). No failure with insertion and gastric tube placement in all the three groups.
Table I: Demographic data
Parameter Group C
N= 30 Group I
N=30 Group P
N=30 Group C vs Group I
(P value) Group I vs Group P
(P value) Group P vs Group C
(P value)
AGE (YRS) 3.51 ± 1.37 3.13 ± 1.51 3.3 ± 1.46 0.947 1.000 1.000
WEIGHT (KG) 16.17 ± 2.98 15.67 ± 3.01 15.40 ± 3.42 0.520 0.747 0.356
(M/F) (14/16) (15/15) (13/17) NS NS NS
Majority of insertion attempts were very easy (83.3, 93.3 and 83.3 in Groups C, I and P respectively). Two difficult insertions were encountered in Group P and none in Group C and Insertion of device was successful on first attempt in 96% of patients and was comparable to Group P (93%) and Group C (91%). Mean insertion time of Group C, I, and P was 22.1 ± 4.4, 16 ± 4.1 and 19.4 ± 6.3 respectively. Group I showed the shortest time for insertion. In the present study mean oropharyngeal seal pressure in Group I (25 ± 2.3) was significantly higher than Group P (22 ± 6 .3) and Group C (16.8 ± 2.6). There was neither desaturation nor significant changes in blood staining and postoperative nausea and vomiting was observed in two cases in Group C and n
one in Group I and P (Table 2).
Table 2: Comparative data between Classic LMA, i-gel, LMA Proseal
Parameter Group C
N= 30 Group I
N=30 Group P
N=30 Group C vs Group I
(P value) Group I vs Group P
(P value) Group P vs Group C
(P value)
Ease of intubation
(VE / E / D / F) 25 / 5 / 0 / 0 28 / 2 / 0 / 0 25 / 3 / 2 / 0 .577 .732 .343
Mean insertion time (SECS) 22.13 ± 4.4 16 ± 4.11 19.4 ± 6.3 .000 .034 .128
Oropharyngeal seal pressure
(cmH2O) 16.8 ± 2.6 25.2 ± 2.8 22.6 ± 2.8 .000 .002 .000
Number of attempts
1st / 2nd / 3rd / failure 27 / 3 / 0 / 0 29 / 1 / 0 / 0 28 / 2 / 0 / 0 NS NS NS
Gastric tube placement
1st / 2nd / 3rd / failure – 27 / 2 / 1 / 0 28 / 1 / 1 / 0 – NS –
Nausea and vomiting 2 0 0 NS NS NS
Laryngospasm/bronchospasm 0 0 0 NS NS NS
Hypoxia(Oxygen Desaturation) 0 0 0 NS NS NS
Tongue-lip-dental trauma 1 0 0 NS NS NS
Blood staining of device 1 0 0 NS NS NS
Regurgitation 0 0 0 NS NS NS
Sore throat & hoarseness in PACU 0 0 0 NS NS NS
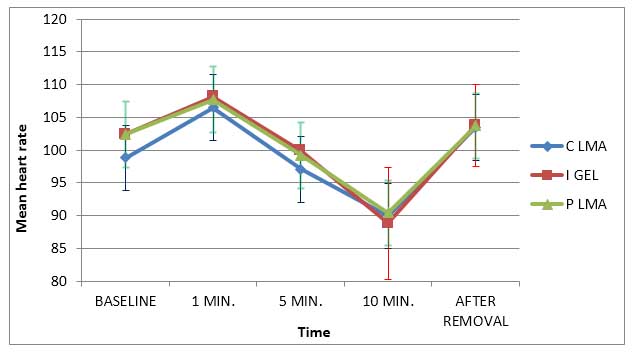
Comparative mean heart rate changes in all the three groups at different time intervals are given in Figure 1.
Figure 1: Showing comparative mean heart rate changes during various stages
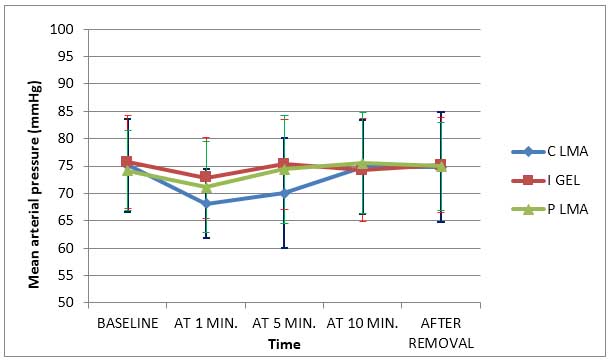
Comparative mean arterial blood pressures in all the three groups at different time intervals are given in Figure 2.
Figure 2: Showing comparative mean arterial pressure during various stages
DISCUSSION
Oropharyngeal seal pressure is used to monitor airway seal which was the primary variable in the study. Pro seal LMA is better suited for pediatric airway than adults6 and its OSP is higher than CLMA. The mean oropharyngeal seal pressure of i-gel was 25.2 ± 2.8 cmH2O for size 1.5, 2.0, 2.5 which was significantly higher than PLMA 22.6 ± 2.8 (size 1.5, 2, 2.5). These results indicate that i-gel provides better seal than same sizes PLMA and CLMA (16.8 ± 2.6). Goldman et al1 reported OSP of 23 cmH2O for PLMA size 1.5, 2.5. Beylacq9 conducted observational study in children and reported an OSP of 25 cmH2O for i-gel in children. Similar results were obtained by Goyal et al10 who concluded that OSP of size 2 i-gel was 26 ± 2.6 cmH2O which was statistically higher than size 2 PLMA (23 ± 1.2 ). Similar results were obtained by Tokgoz11 and Das et all 12.
In patients with high airway pressure i-gel may provide a wide safety range for positive-pressure ventilation. The cuff of the size 1.5, 2 and 2.5 PLMAs differ from the adult sizes as they lack a dorsal cuff which plays a minor role in the improved seal13.Perhaps, wider proximal end and larger distal cuff helps in improved seal.
Shimbori et al found no significant difference in children and found OSP of PLMA 18 cmH2O and CLMA 19 cmH2O, whereas Krippacheril reported OSP of 23.1 and 23.26 cmH2O respectively for these devices.
The majority of insertion attempts were very easy in all three devices. There were two difficult insertions with PLMA. The placement of PLMA has been found to be more difficult in adults than children. The larger bowl of PLMA is more difficult to insert and is likely to fold over. The large tongue, floppy epiglottis, anterior larynx and presence of tonsillar hypertrophy makes PLMA difficult to insert in pediatric patients.15 I-gel and CLMA are easier to insert as they have small bowl and cuff size. Our results are in concurrence with previous studies.16
First attempt insertion rates were greater than 90% in all three groups. No patients required third attempt nor was there a failure to insert the device in any group. Our results are similar with previous studies.9,17,18,19 In manikin study using eight types of SGD overall success rate for insertion of i-gel was >90%.20
In our present study, the mean times for insertion in groups C, I and P were 22.13 ± 4.439 seconds, 16.03 ± 4.115 and 19.43 ± 6.393 seconds respectively. I-gel showed lshortest mean time for insertion. Shorter insertion times influence the feasibility of SGD for routine use.21 This can be attributed to the fact that I-gel has a more robust and streamlined design than the PLMA and LMA Classic, making it easier to hold and insert. Also it does not have a cuff so the time taken to inflate the cuff is saved in this device. This advantage might not have a marked clinical impact on routine elective surgeries but it definitely gains importance in situations of resuscitation and in difficult airway situations where achieving an effective airway quickly is of paramount importance.
Both i-gel™ and PLMA are more reliable than CLMA in terms of aspiration risk because they allow gastric drainage. Previous studies indicated that nasogastric tubes (N/G) of size 8-10 fr could be easily passed through the i-gel channel and gastric contents could be aspirated via the N/G.17,22 In present study success rate of gastric tube placement in 1st attempt was 90% and 93.33% for i-gel and PLMA respectively and the gastric tube was inserted in 100% of cases in 2nd attempt. This helps in preventing and decreasing air leak and thus decreasing postoperative nausea and vomiting. The successful placement of the gastric tube also aids in correct positioning of the PLMA.
Regarding the hemodynamic stability and effect of each of the SGDs, no statistically significant difference was reported when comparing heart rate and mean arterial blood pressure intraoperatively.23,24 Since placement of the CLMA and PLMA involves the inflation of the cuff in the hypopharynx, these are expected to produce a similar response. I-gel does not have an inflatable cuff, it has a cuff made of thermoplastic elastomer it still showed a similar response like the other two devices. As the receptors adapt to constant pressure on the pharyngeal wall these changes were expected to be transient as showed in the present study.
One of the most important parameters to be compared between three SGDs was perioperative complications. It was estimated that difference between CLMA, i-gel and PLMA regarding perioperative complications was not statistically significant except nausea / vomiting, and blood staining of device. Incidence of postoperative nausea vomiting was significantly higher in CLMA due to high incidence of gastric insufflation. There was no incidence of sore throat in any group. This observation of our study is supported by the study of Wong et al25 where they stated that if the intracuff pressure remains less than 60 cmH2O there is minimal chance of sore throat. None of the children had laryngospasm/bronchospasm, hypoxia, tongue-lip-dental trauma and sore throat and hoarseness in post anesthesia care unit in the present study.
LIMITATIONS
Our study has few limitations that need discussion. We included children with normal airway. Therefore, the results of this study cannot be extrapolated to patients with difficult airway. Although group assignment was random but the person collecting the data was not blind to study groups. Therefore an observer’s bias can exist.
CONCLUSION
Based on these finding we conclude that i-gel is comparable to PLMA and CLMA in clinical performance. There was no difference regarding ease of insertion, number of attempts for successful placement and perioperative complications. I-gel has a higher oropharyngeal seal pressure than CLMA and PLMA and time taken for insertion was also shorter. It has an added advantage of gastric channel, which is found only in PLMA and LMA supreme.
Thus i-gel is equally safe, efficient and cost effective in children compared with other pediatric supraglottic airway devices and can be reliably used routinely by anesthesiologist in pediatric patients.
Conflict of interest: None declared by the authors
Author contribution: YD, AG: Help in conduction of study. US: Help in manuscript editing (guide). AM: Help in statistics. KDJ & SM: Conducted the study
REFERENCES
- Goldmann K, Jakob C. A randomized crossover comparison of the size 2 1/2 laryngeal mask airway ProSeal versus laryngeal mask airway-Classic in pediatric patients. Anesth Analg 2005;100:1605-1. [PubMed]
- Goldmann K, Roettger C, Wulf H. The size 1.5 Proseal laryngeal mask airway in infants: a randomised,crossover investigation with the classic laryngeal mask airway. Anesth Analg 2006;102:405-10. [PubMed]
- Ramesh S, Jayanthi R. Supraglottic airway devices in children. Ind J Anaesth 2011;55:476-82. doi: 10.4103/0019-5049.89874. [PubMed] [Free full text]
- Mitra S, Das B, Jamil SN. Comparison of size 2.5 i-gelTM with proseal LMA in anaesthetised, paralyzed children undergoing elective surgery. North Am J Med Sci. 2012;4:453-7. [PubMed] [Free full text]
- Sharma S, Scott S, Rogers R, Popat M. The I-gel airway for ventilation and rescue intubation. Anaesthesia 2007;62:419-20. [PubMed] [Free full text]
- Gabbot DA, Beringer R. The iGELsupraglotticairway:A potential role for resuscitation? Resuscitation 2007;73:161-2. [PubMed]
- Sinha A, Sharma B, Sood J. ProSeal as an alternative to endotracheal intubation in pediatric laparoscopy. PediatrAnesth. 2007;17:327–32 [PubMed]
- Karippacheril JG, Varghese E. Crossover comparison of airway sealing pressures of 1.5 and 2 size LMA-ProSeal™ and LMAClassic™ in children, measured with the manometric stability test. PediatrAnesth. 2011;21:668–72. doi: 10.1111/j.1460-9592.2011.03554.x [PubMed]
- Beylacq L, Bordes M, Semjen F, Cros AM. The i-gel, a single use supraglottic airway device with a non-inflatable cuff and an esophageal vent: An observational study in children. Acta Anaesthesiol Scand 2009;53:376-9. [PubMed] doi: 10.1111/j.1399-6576.2008.01869.x.
- Goyal R, Shukla RN, Kumar G. Comparison of size 2 i-gel supraglottic airway with LMA-ProSeal™ and LMA-Classic™ in spontaneously of Anesthesiologists (ASA) Annual Meeting; 17–21 October, 2009. p. A147. [PubMed]
- Tokgoz O, Tufek A, BeyazSG, Yuksel MU, Celik F, AycanI O, Guzel A. Comparison of the efficacies of I-gel™ and LMA-ProSeal™ for airway management in pediatric patients. Turk J Med Sci. 2013;43:208-213.
- Das B, Mitra B, Jamil SN, Varshney RK; Comparison of three supraglottic devices in anesthetised paralysed children undergoing elective surgery. Saudi J Anaesth. 2012:6;224-228 . [PubMed] [Free full text]
- Lopez-Gil M, Brimacombe J, Garcia G. A randomised non-crossover study comparing the ProSeal and Classic laryngeal mask airway in anaesthetised children. Br J Anaesth 2005;95:827-830. [PubMed] [Free full text]
- Saran S Mishra, S K bandhe, A S Vasudev, A Elakkumanan, LB Mishra. Comparison of I gel supraglottic airway and LMA proseal in paediatric patients under controlled ventilation. J Anaesthesiol Clin Pharmacol. 2014;30:195-8 [PubMed] [Free full text]
- ClinicalTrials.gov [Internet] Comparison of I-gel to the Laryngeal Mask Airway. [updated 2011 March 11; cited 2012 Jan 22]. Available from: www.clinicaltrials.gov/ct2/show/NCT00706823.
- Janakiraman C, Chethan DB, Wilkes AR, Stacey MR, Goodwin N. A randomised crossover trial comparing the i-gel supraglottic airway and classic laryngeal mask airway. Anaesthesia 2009;64:674-8. doi: 10.1111/j.1365-2044.2009.05898.x. [PubMed] [Free full text]
- Richez B, Saltel L, Banchereau F, Torrielli R, Cros AM. A new single use supraglottic airway device with a noninflatable cuff and an esophageal vent: An observational study of the i-gel. Anesth Analg. 2008;106:1137-9. doi: 10.1213/ane.0b013e318164f062. [PubMed]
- Bopp C, Carrenard G, Chauvin C, Schwaab C, Diemunsch P. American Society of Anesthesiologists (ASA) Annual Meeting. A147. New Orleans, USA: 2009. Oct 17-21, The I-gel in paediatric surgery: Initial series.
- Shimbori H, Ono K, Miwa T, Morimura N, Noguchi M, Hiroki K. Comparison of the LMA-ProSeal and LMA-Classic in children. Br J Anaesth 2004;93:528-31. [PubMed] [Free full text]
- Jackson KM, Cook TM. Evaluation of four airway training manikins as patient simulators for the insertion of eight types of supraglottic airway devices. Anaesthesia. 2007;62:388-93. [PubMed] [Free full text]
- Lee JR, Kim MS, Kim JT, Byon HJ, Park YH, Kim HS, et al. A randomised trial comparing the i‑gelTM with the LMA classicTM in children. Anaesthesia. 2012;67:606‑11. doi: 10.1111/j.1365-2044.2012.07072.x. [PubMed] [Free full text]
- Gibbison B, Cook TM, Seller C. Case series: Protection from aspiration and failure of protection from aspiration with the i-gel airway. Br J Anaesth 2008;100:415-7. doi: 10.1093/bja/aem396 [PubMed] [Free full text]
- Jindal P, Rizvi A, Sharma JP. Is I-gel a new revolution among supraglottic airway devices?–a comparative evaluation. Middle East J Anaesthesiol. 2009 Feb;20(1):53-8. [PubMed]
- Helmy AM, Atef HM, El-Taher EM, Henidak AM. Comparative study between I-gel, a new supraglottic airway device, and classical laryngeal mask airway in anesthetized spontaneously ventilated patients. Saudi J Anaesth 2010;4:131-6. doi: 10.4103/1658-354X.71250. [PubMed] [Free full text]
- Wong JG, Heaney M, Chambers NA, Erb TO, von Ungern-Sternberg BS. Impact of laryngeal mask airway cuff pressures on the incidence of sore throat in children. PediatrAnesth. 2009;19:464–9. doi: 10.1111/j.1460-9592.2009.02968.x [PubMed]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube