Mirza Majid Ali Zaki1, Sarmad Wahaj Siddiqui2, Madiha Zafar3
Author affiliation:
- Mirza Majid Ali Zaki, Dept. of Anaesthesia ITU,LNWUH Trust NHS, Watford Road, HA13UJ, London, UK; E-mail: mirzamajidalizaki@yahoo.com
- Sarmad Wahaj Siddiqui, Dept. of Primary Secondary Healthcare, Lahore, Punjab, Pakistan; E-mail: swissjack@gmail.com
- Madiha Zafar, Department of Anaesthesia, KEMU, Lahore, Punjab, Pakistan; E-mail: Dr.madihazafar@hotmail.com
Correspondence: Mirza Majid Ali Zaki; E-mail: mirzamajidalizaki@yahoo.com; Phone: +44 7506806093
Abstract
Background: Vaccine acceptance can play a pivotal role towards control of COVID-19. Many healthcare workers (HCWs) have articulated safety and effectiveness concerns despite being the frontline takers of vaccination. This survey was aimed to investigate the causes of COVID-19 vaccine hesitancy and distrust among HCWs of Pakistani origin.
Methodology: This internet-based survey was conducted on 138 HCWs of Pakistani origin from January 2021 to April 2021.
Results: Out of a total of 138 subjects, 137 (99.3%) HCWs responded to the survey. COVID-19 vaccinations had already been administered to 101 (74%) of the respondents. Out of 36 (26.2%) unvaccinated individuals, 19 (14%) completely declined the vaccination. The prevalence of participants who distrust vaccination effectiveness and safety was 110 (80.3%), while 94 (68.6%) believed vaccine safety was compromised due to rapid development. The prevalence of HCWs who believed long-term adverse effects and that the manufacturers falsified the data was 36 (26.3%) and 22 (16%) respectively.
Conclusion: Our survey found that fears and concerns about the efficacy of the vaccine can impasse struggles to disease transmission and vaccine distribution. Healthcare workers in Pakistan had a higher prevalence of vaccine acceptance compared to other surveys.
Key words: Acceptance; COVID-19; COVID-19 vaccine; Healthcare workers; HCWs; Vaccine hesitancy
Citation: Zaki MMA, Siddiqui SW, Zafar M. Vaccine hesitancy and distrust: concerns of healthcare workers of Pakistani origin-a survey. Anaesth. pain intensive care 2022;26(6):767-772; DOI: 10.35975/apic.v26i6.2056
Received: December 31, 2021; Reviewed: September 17, 2022; Accepted: September 18, 2022
Introduction
COVID-19 pandemic has been propagated with resurgent third wave and delta variants across the globe. Vaccination is among the various measures taken to control this widespread pandemic threat.1,2 Affluent countries have already secured adequate vaccine supplies, while impoverished countries had to wait for their turn. COVID-19 vaccines are being distributed worldwide. However, vaccine hesitancy among the population is the major challenge for policymakers.3 Various studies have discovered the COVID-19 vaccine acceptance rate and factors that influence it.4-6 Nicola et al. compared the acceptance rate of COVID-19 vaccine among Chinese healthcare workers (HCWs) versus the general population.7 A USA based study found that about 20% population intended to refuse COVID-19 vaccination.8 The pandemic news began to spread in Pakistan in early 2020, whereas some COVID-19 infected cases were reported in pilgrims returning from the Iranian shrines. SARS-Cov-2 has currently affected 120 million people worldwide and a staggering number of deaths was reported to be about 2.65 million.9 The statistics of mortality and infected people in Pakistan were 21,022 and 926,695 respectively.10 Pakistan began its coronavirus vaccination campaign in first quarter of 2021 when the first batch of the vaccines arrived from China. The vaccine was first given to HCWs who were treating COVID-19 patients. It was then made available to people over the age of 60 through a nationwide campaign, and it is now available to everyone aged 19 and above.11
Quarantines and social isolation or distancing like unstipulated measures can slow the virus spread, gaining epidemic flattened curve, but without establishing the herd immunity among the population through vaccination, the COVID-19 epidemic will not end.12 More than 40 academic institutes and pharmaceutical companies had started their vaccine development process against infectious coronavirus while some started clinical trials before launching the vaccine to the real world.13 However, healthcare authorities failed to communicate efficacy and safety of vaccine to the population convincingly. Lack of trust in vaccines efficacy and success, vaccination systems, as well as the ease of gaining service and higher costs, may all have reduced the vaccination acceptance.14 Furthermore, HCWs can play a key role in spreading awareness regarding vaccinating and increasing acceptance rates among the general population irrespective of their exposure to high-risk pathogen infectious diseases such as COVID-19 and influenza viruses.15,16
A study conducted in Pakistan found that the major barriers to vaccination are myths and conspiracies which apply to most vaccination campaign outcomes, affecting people’s reservations regarding vaccine efficacy and safety.17 Vaccine hesitancy was found in a significant proportion of the population. Concerns about vaccine safety are central to the majority of these anti-vaccine movements. Yang et al.18 investigated the reasons for vaccine refusal and discovered them to be quite complex.
The purpose of this study was to determine the prevalence and predictors of COVID-19 vaccine hesitancy (VH) among Pakistani-origin HCWs.
Methodology
This internet-based survey was conducted on 138 HCWs of Pakistani origin in January 2021. The questionnaire contained queries regarding HCWs’ hesitancy and safety concerns of the COVID-19 vaccine. Also, the prevalence of hesitant HCWs was identified. The questionnaire was approved and revised by all the researchers and was pilot tested on 138 participants, out of which 137 responded and one declined..
The completed questionnaire comprised of different sections: demographic details, details about COVID-19 vaccination, contracting COVID-19 during the current pandemic, beliefs, and information about COVID-19 vaccination, and hesitancy and barriers to COVID-19 vaccination. All the participants (HCWs) were grouped into six categories according to age: 18 to 25 y, 26 to 30 y, 31 to 35 y, 36 to 40 y, 40 to 50 y, and > 50 y. Individuals who intended to refuse vaccination were defined as vaccine-hesitant. The social media platforms like e-mail were used for distributing the questionnaire to potential HCWs (participants) either living in Pakistan or other countries having Pakistani origin. Participants were encouraged to give details about their family and friends who were infected with coronavirus. The title, purpose, inclusive, and exclusive criteria of the study were clarified to the contributors following written informed consent taken prior to conducting the survey.
The second section evaluated acceptance and hesitance toward the COVID-19 vaccination by asking, ‘Do you intend to get the COVID-19 vaccine when it becomes available?’ Based on the responses ‘Yes’ and ‘No/Unknown,’ participants were divided into two groups: ‘vaccine acceptant’ and ‘vaccine hesitant’. The second section also evaluated participants’ COVID-19 vaccine perceived beliefs and knowledge.
The third section looked at the perceptions about the COVID-19 vaccine concerns, risks, and safety.
Finally, the fourth section inquired about the sources from which the participants obtained information on COVID-19 vaccines, as well as their level of trust in these sources.
Statistical analysis
SPSS version 20 was used for data analysis. Chi-square test was used to investigate the relationship between socio-demographic characteristics and attitudes toward COVID-19 vaccination at a 5% significance level.
Results
Of the total 138 HCWs approached, 137 (99.3%) responded to the questionnaire-based survey and 1 (0.7%) declined. COVID-19 vaccination had already been done in 101 (74%) respondents. A good number of 127 (93%) participants found that contacting infected patients could cause COVID-19, while the prevalence of positive PCR and raised antibodies were 36 (26.3%) and 14 (10%) respectively. Out of the 36 (26.2%) unvaccinated individuals, 19 (14%) completely declined the vaccination. The number of participants who expressed distrust towards vaccination effectiveness and safety was 110 (80.3%), while 94 (68.6%) believed vaccine safety was compromised due to rapid development and lack of evidence. The prevalence of HCWs who believed long-term adverse effects and manufacturer falsified data was in 36 (26.3%) and 22 (16%) respectively.
The participants overall mean age was 35.26 ±1.01 y with an age range from 18 y to 59 y. The frequency of participants in different age groups were as follows: 18-25 y 8 (5.8%), 26-30 y 37 (26.8%), 31-35 y 34 (24.6%), 36-40 y 35 (25.4%), 40-50 y 11 (8%), and > 50 y 12 (8.7%) as shown in Figure 1.
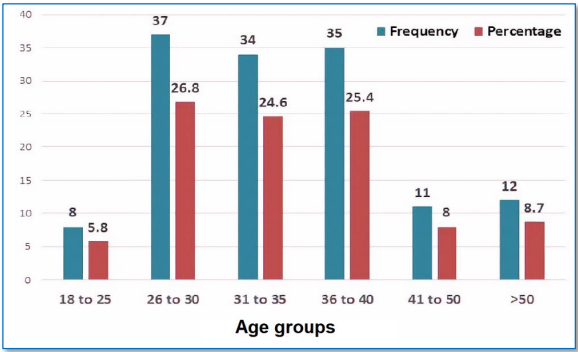
Figure 1: Age-wise distribution of the participants (n = 137)
The vaccine hesitance group had lower understanding, knowledge, and confidence regarding the COVID-19 vaccine compared to the acceptance group. The odds of knowing which vaccine to get, believing that the vaccine will effectively stop the pandemic, vaccines work understanding and believing that the immune system improved with vaccination were prevalent in acceptance group HCWs. Demographic details of participants are shown in Table 1.
| Table 1: Demographic details of health worker (n=138) | ||
| Demographic Factors | N (%) | |
| Age (y)
|
18-25
26-30 31-35 36-40 41-50 > 50 |
8 (5.8)
37 (26.8) 34 (24.6) 35 (25.4) 11 (8) 12 (8.7) |
| Residency
|
Pakistan
KSA USA UK Other |
110 (79.7)
8 (5.9) 2 (1.45) 14 (10.1) 4 (2.85) |
| Clinical Specialty | Medical Specialty
Family Physician Medical Students Public Health Businessman Administrator |
128 (92.8)
1 (0.7) 3 (2.2) 3 (2.2) 1 (0.7) 1 (0.7) |
Most of the HCWs agreed to coronavirus vaccination’s safety, effectiveness, comfort, and efficacy as shown in Table 2. The participant’s response regarding hesitancy and distrust of COVID-19 vaccine is also shown in Table 2.
| Table 2: Participant’s knowledge, beliefs, and hesitancy about the COVID-19 vaccine (n = 137) | |||
| Parameters | Response | n | % |
| COVID-19 vaccination done
|
Yes
No |
101
36 |
73.7
26.3 |
| Have you ever had symptoms of COVID-19 disease? | Yes
No |
35
102 |
26.3
73.7 |
| Have you ever tested PCR positive for COVID-19? | Yes
No Never Tested |
36
69 32 |
26.3
50.4 23.3 |
| Have you ever had positive antibodies to COVID-19?
|
Yes
No Never Tested |
13
50 74 |
9.4
36.5 54.1 |
| Due to your job are you at high risk for contracting COVID-19 from direct patient contact? | Yes
No |
127
10 |
92.7
7.3 |
| Has anyone in your household been diagnosed with COVID-19? | Yes
No |
48
89 |
35
65 |
| Has anyone in your family members or friends been diagnosed with COVID-19? | Yes
No |
121
16 |
88.3
11.7 |
| Have you ever come across anyone (in clinical practice or otherwise) who has had severe side effects of COVID-19 vaccine? | Yes
No Not Sure |
44
88 5 |
32.1
64.2 3.6 |
| If not would you like to get vaccinated against COVID-19? | Yes
No No response |
28
9 100 |
20.4
6.7 72.9 |
| Have you ever refused to be vaccinated against COVID-19?
|
Yes
No No Response |
19
115 3 |
13.9
83.9 2.2 |
| Do you think COVID-19 vaccines safe?
|
Yes
No |
125
12 |
91.2
8.8 |
| Do you think benefits of COVID-19 vaccine outweigh its risks?
|
Yes
No Not Sure |
120
14 3 |
87.6
10.2 2.2 |
| Do you think COVID-19 vaccines will reduce infection rate and help prevent disease?
|
Yes
No Not Sure |
127
7 3 |
92.6
5.1 2.2 |
Overall, HCWs have a more comprehensive knowledge of the infectious disease compared to over-all population. Mostly HCWs agreed that the corona virus is dangerous to people of all ages, and that infected people who are elderly or have chronic diseases face an increased risk of death. Of the total 137 HCWs who responded, 92% related COVID-19 high risk from possible contact with infected patients whereas polymerase chain reaction (PCR) was either tested positive in 26.3% or antibodies level raised in 9.4%. A great majority of HCWs showed concerns over vaccine safety and efficacy and 68.1% believed that vaccination was rapidly developed without considering their safety. About15.9% believed that vaccination manufacturer falsified their data while 26.1% responded to vaccination’s long-term adverse effects. The COVID-19 vaccine, which is currently being developed, was deemed necessary by 90% of HCWs. The future vaccine was tolerated better by the HCWs. In comparison to the general population, about 68.1% of HCWs assumed that additional time was required before vaccine introduction, that they could accept severe effects like allergic reactions, and that they could accept more severe reactions.
Discussion
The present Pakistani region-stratified study surveyed the HCWs knowledge of COVID-19 and their approach toward forthcoming vaccination in Pakistan using an internet-based questionnaire. In comparison to the general population, HCWs demonstrated greater tolerance for adverse effects and vaccine effectiveness. The epidemic may also provide additional potential benefits, such as influenza or pneumonia vaccination. Disease trends, communal acquaintances’ decisions, and infectious disease-related high risks, are all related with an elevated likelihood of selecting vaccination among HCWs. Most HCWs agreed to get the vaccination for coronavirus post-introduction, which is mainly due to the risk assessment of infectious disease and assurance in the vaccine’s efficacy and safety. HCWs were much more likely to become infected with the corona virus. In our study, 92% of HCWs considered that they got coronavirus as a result of close contact with infected patients. Uncertainty about how the epidemic will unfold also plays a role in risk assessment.
While the COVID-19 pandemic has globally overwhelmed healthcare systems, Pakistan has escaped the worst of the disease’s high mortality. Pakistani caseload has been lower than in the developed countries due to its younger population and early adherence to facemask and social distancing mandates. Other South Asian countries with comparable socioeconomic and demographic characteristics to Pakistan fared worse in terms of COVID-19-related morbidity and mortality.19 In contrast, Pakistan has a difficult history of polio eradication due to vaccine aversion in many of its endemic regions.20,21 A US-based study conducted on HCWs reported a higher vaccine acceptance rate in male HCWs compared to female HCWs.22 Our study contradicts these findings due to higher female HCWs acceptance compared to male HCWs in our study. Additionally, HCWs involved in indirect patientcare had higher hesitancy of vaccine acceptance compared to direct patientcare HCWs, which was in agreement to their study. Also, HCWs of the age range 51 to 60 y had a higher rate of vaccine acceptance.
HCWs had a favorable attitude toward the vaccine. HCWs play an important role in the public willingness to get vaccinated, which can lead to an increase in vaccine coverage. It was discovered that knowledge and acceptance increased with HCWs readiness to recommend immunization. According to a United Kingdom based study, highly educated HCWs (nurses) preferred influenza vaccination to their families and recommended it for the future.23 Concerned about the poor quality of local based vaccine production, vaccine hesitancy developed in certain HCWs, which may influence their own decisions and the public advocacy regarding vaccination. In the present study, about 22.7% of HCWs trusted vaccines produced by domestic manufacturers.24
Another potential advantage of the COVID-19 pandemic is that it serves as a virtuous health education against contagious diseases. In our study, we observed health protection such as wearing masks and receiving more vaccinations. The difference in getting a vaccination for COVID-19 in HCWs from the general population might be explained by their risk evaluation and knowledge level. The increased perception of coronavirus disease as enhanced influenza may increase the vaccine acceptance rate among HCWs.25 The social status of both HCWs and the general population influence their knowledge and perception regarding COVID-19 vaccination. The attitude and behavior of friends, relatives, and neighbors also play a key role in HCWs’ decisions regarding vaccinations. The acceptance and uptake of the coronavirus vaccine by others significantly influence the vaccine intent in terms of weakness or strength.26 The coronavirus vaccine’s social acceptance and clear choice increase the vaccination rate among HCWs and the public.
Currently, vaccine acceptance has been a major challenge, raising public and HCWs concern about trust in the COVID-19 immunization process even in developed countries; similar conspiracies and myths were also encountered for rubella, polio, mumps, and measles resulting in a reduction of vaccination acceptance.27 In Pakistan, similar to polio vaccination, the COVID-19 vaccination is facing certain issues regarding its safety and efficacy.28 Many researchers from the US and Canada studied the possible association of education level with beliefs in vaccination and found that a significant proportion of the educated population had similar concerns regarding the efficacy and safety of the coronavirus vaccine.29,30 Educated participants like HCWs in our case had doubts about vaccine safety but mostly agreed to the vaccine immunity and were against the myths.
The coronavirus vaccination rates can boost by providing obvious data regarding vaccine composition, working, side effects and risks, effectiveness, testing, and safety. Unfortunately, no strict stance was taken by the government against false claims, myths, and disinformation about coronavirus vaccines. Putting all efforts into implementing the actions towards reducing the spread of misinformation will result in control and mitigation of the coronavirus pandemic.
Conclusion
Our study found that fears about the efficacy and the consequence of the COVID-19 vaccine can impasse struggles to control the disease spread. The safety and efficacy issues influenced the coronavirus vaccine acceptance. Healthcare workers in Pakistan had a higher prevalence of vaccine acceptance compared to other surveys. Healthcare workers advocacy and official effective communication can ensure success of the national vaccine strategy.
Conflict of interest
No author had any conflict of interest.
Data availability
The numerical data generated during this research is available with the authors.
Acknowledgement
We gratefully thank all participants of this project.
Funding
The study did not utilize any internal or external or industry grant.
Authors’ contribution
All authors equally contributed in concept of the study, conduct the study, data collection, data analysis. manuscript writing, editing and correction, and final approval.
References
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020 Mar 26;382(13):1199-1207. [PubMed] DOI: 1056/NEJMoa2001316
- Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020 May 1;368(6490):489-93. [PubMed] DOI: 1126/science.abb3221
- Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020 Mar 21;395(10228):931-934. [PubMed] DOI: 1016/S0140-6736(20)30567-5
- Zhang J, Zeng H, Gu J, Li H, Zheng L, Zou Q. Progress and prospects on vaccine development against SARS-CoV-2. Vaccines. 2020 Jun;8(2):153. [PubMed] DOI: 3390/vaccines8020153
- Saladino V, Algeri D, Auriemma V. The psychological and social impact of Covid-19: new perspectives of well-being. Front Psychol. 2020 Oct 2;11:577684. [PubMed] DOI: 3389/fpsyg.2020.577684
- Chaudhary FA, Ahmad B, Ahmad P, Khalid MD, Butt DQ, Khan SQ. Concerns, perceived impact, and preparedness of oral healthcare workers in their working environment during COVID-19 pandemic. J Occup Health. 2020 Jan;62(1):e12168. [PubMed] DOI: 1002/1348-9585.12168
- Alradhawi M, Shubber N, Sheppard J, Ali Y. Effects of the COVID-19 pandemic on mental well-being amongst individuals in society- A letter to the editor on “The socio-economic implications of the coronavirus and COVID-19 pandemic: A review”. Int J Surg. 2020 Jun;78:147-148. [PubMed] DOI: 1016/j.ijsu.2020.04.070
- Forni G, Mantovani A. COVID-19 vaccines: where we stand and challenges ahead. Cell Death Differ. 2021 Feb;28(2):626-639. [PubMed] DOI: 1038/s41418-020-00720-9
- Cavaleri M, Enzmann H, Straus S, Cooke E. The European Medicines Agency’s EU conditional marketing authorisations for COVID-19 vaccines. Lancet. 2021 Jan 30;397(10272):355-357. [PubMed] DOI: 1016/S0140-6736(21)00085-4
- Felter C. What to Know About the Global COVID-19 Vaccine Rollout So Far. Council on Foreign Relations; 2021 Jan 21. Available from: https://www.cfr.org/in-brief/what-know-about-global-covid-19-vaccine-rollout-so-far
- Duplaga M. The Determinants of Conspiracy Beliefs Related to the COVID-19 Pandemic in a Nationally Representative Sample of Internet Users. Int J Environ Res Public Health. 2020 Oct 26;17(21):7818. [PubMed] DOI: 3390/ijerph17217818
- Khan YH, Mallhi TH, Alotaibi NH, Alzarea AI, Alanazi AS, Tanveer N, et al. Threat of COVID-19 Vaccine Hesitancy in Pakistan: The Need for Measures to Neutralize Misleading Narratives. Am J Trop Med Hyg. 2020 Aug;103(2):603-604. [PubMed] DOI: 4269/ajtmh.20-0654
- MacDonald NE. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015 Aug 14;33(34):4161-4. [PubMed] DOI: 1016/j.vaccine.2015.04.036
- Skjefte M, Ngirbabul M, Akeju O, Escudero D, Hernandez-Diaz S, Wyszynski DF, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. 2021 Feb;36(2):197-211. [PubMed] DOI: 1007/s10654-021-00728-6
- Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger JA. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013 Aug 8;9(8):1763-73. [PubMed] DOI: 4161/hv.24657
- Schuster M, Eskola J, Duclos P. Review of vaccine hesitancy: Rationale, remit and methods. Vaccine. 2015 Aug 14;33(34):4157-60. [PubMed] DOI: 1016/j.vaccine.2015.04.035
- Funk C, Tyson A. Intent to get a COVID-19 vaccine rises to 60% as confidence in research and development process increases. Pew Research Center. 2020 Dec 3;3. [FreeFullText]
- Yang R, Penders B, Horstman K. Addressing vaccine hesitancy in china: A scoping review of chinese scholarship. Vaccines. 2020 Mar;8(1):2. [PubMed] DOI: 3390/vaccines8010002
- Hussain SF, Boyle P, Patel P, Sullivan R. Eradicating polio in Pakistan: an analysis of the challenges and solutions to this security and health issue. Global Health. 2016 Oct 12;12(1):63. [PubMed] DOI: 1186/s12992-016-0195-3
- Kobes WJ, Mulder AT, Sonneveld JJ. Whose Agenda Is It Anyway? The Effect of Disinformation on COVID-19 Vaccination Hesitancy in the Netherlands. In: Electronic Participation: 13th IFIP WG 8.5. International Conference, EPart 2021. Granada, Spain, September 7-9, 2021: Proceedings 2021 (Vol. 12849, p. 55). Springer Nature;2021.
- Abbas Q, Mangrio F, Kumar S. Myths, beliefs, and conspiracies about COVID-19 Vaccines in Sindh, Pakistan: An online cross-sectional survey. Authorea. 2021 Mar 8. DOI: 22541/au.161519250.03425961/v1
- Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021 Jan 4;12(1):29. [PubMed] DOI: 1038/s41467-020-20226-9
- Elbarazi I, Al-Hamad S, Alfalasi S, Aldhaheri R, Dubé E, Alsuwaidi AR. Exploring vaccine hesitancy among healthcare providers in the United Arab Emirates: a qualitative study. Hum Vaccin Immunother. 2021 Jul 3;17(7):2018-2025. [PubMed] DOI: 1080/21645515.2020.1855953
- Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID-19 Vaccine in Southeast Asia: A Cross-Sectional Study in Indonesia. Front Public Health. 2020 Jul 14;8:381. [PubMed] DOI: 3389/fpubh.2020.00381
- Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, et al Acceptability of vaccination against covid-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res. 2020 Oct 29;11:103-109. [PubMed] DOI: 2147/POR.S271096
- Abid K, Bari YA, Younas M, Tahir Javaid S, Imran A. Progress of COVID-19 Epidemic in Pakistan. Asia Pac J Public Health. 2020 May;32(4):154-156. [PubMed] DOI: 1177/1010539520927259
- Ali M, Ahmad N, Khan H, Ali S, Akbar F, Hussain Z. Polio vaccination controversy in Pakistan. Lancet. 2019 Sep 14;394(10202):915-916. [PubMed] DOI: 1016/S0140-6736(19)32101-4
- El-Showk S. Don’t demonize parents who are hesitant to vaccinate – discuss their worries instead. Nature. 2019 Nov;575(7784):S57. [PubMed] DOI: 1038/d41586-019-03641-x
- Global MW. How Does the World Feel about Science and Health. GALLUP: London, UK; 2018.
- Fernández-de-Las-Peñas C, Navarro-Santana M, Gómez-Mayordomo V, Cuadrado ML, García-Azorín D, Arendt-Nielsen L, et al. Headache as an acute and post-COVID-19 symptom in COVID-19 survivors: A meta-analysis of the current literature. Eur J Neurol. 2021 Nov;28(11):3820-3825. [PubMed] DOI: 10.1111/ene.15040




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube