Indira Kumari, MBBS, MD*, Udita Naithani, MBBS, MD**,
Devendra Verma, MBBS, MD**, Rajkumar S, MBBS***,
Dharm Chand Jain, MBBS, MD****, Pradeep D S, MBBS*****
*Professor and Head, **Associate Professor, ***Junior Registrar, ****Senior Resident, *****Senior Registrar
Department of Anesthesiology, RNT Medical College attached to MB Government Hospital, Udaipur, Rajasthan (India)
Correspondence: Dr. Udita Naithani, II/ 238, OTC Scheme, Charak Marg, Udaipur, Rajasthan-313001 (India); E-mail: dr.rajkumar@ymail.com; druditanaithani@yahoo.com
ABSTRACT
Surgical tourniquets are commonly used in orthopaedic and trauma surgery, but these have their complications. Reperfusion injury following simultaneous release of bilateral tourniquets is the most likely explanation of cardiac arrest in this case. We describe an unusual complication experienced by a 40 year old, 65 kg healthy male who underwent surgery for trauma to the lower extremity (bilateral fracture tibia). Bilateral mid-thigh tourniquets (Esmarch bandage) were applied, which were simultaneously released after 90 min. After 5 min of tourniquet release sudden severe hypotension occurred followed by cardiac arrest. Patient was immediately intubated and cardio pulmonary cerebral resuscitation (CPCR) was started. We conclude that bilateral tourniquet application can be hazardous within the safe limit of tourniquet time (<2 hours) and their simultaneous release should be avoided. Moreover, Esmarch tourniquet may generate very high uncontrolled pressures and should be avoided.
Keywords: Bilateral tourniquet; Simultaneous release of bilateral tourniquets; Cardiac arrest; Reperfusion syndrome
Citation: Kumari I, Naithani U, Verma D, Rajkumar S, Bansal S, Jain DC, Dr Pradeep DS. Cardiac arrest after simultaneous release of bilateral thigh tourniquets: A case report. Anaesth Pain & Intensive Care 2013;17(3):285-288
INTRODUCTION
Tourniquets are required in orthopedic surgery to facilitate surgical exposure and to reduce blood loss.1 Tourniquet application can lead to both local complications (like skin necrosis, direct neurovascular injury, ischemia of tissue and muscle, thrombus formation as well as systemic complications like pulmonary embolism and reperfusion injury.2,3 Most of these problems are transient but sometimes may be permanent or life threatening.
Bilateral limb surgeries using tourniquets is increasing now a days because of advantages like limiting an invasive surgical procedure and anesthesia to a single event, promoting symmetrical rehabilitation of both limbs, potentially reducing the length of hospital stay and cost. However higher cardiopulmonary complications and blood transfusion requirement with simultaneous procedures questioned its true safety.4
The cases of cardiac arrest have been reported following tourniquet release attributed to reperfusion syndrome,5 pulmonary artery embolization6,7 and coronary artery vasospasm8.
We report a case of cardiac arrest that occurred 5 min after simultaneous release of bilateral thigh tourniquets. The patient was resuscitated successfully. Possible mechanisms of cardiac arrest, precautions and management are discussed.
CASE REPORT
A 40 year, 65 kg male (ASA grade I) had multiple fractures (both tibias and right ulna) due to road traffic accident. He was planned for proximal fixation of left tibia and distal fixation with plating of right tibia under spinal anesthesia. His history, physical examination and investigations were unremarkable. Patient was taken in elective operating room after overnight fasting. A multiparameter monitor with non-invasive blood pressure (NIBP), electrocardiography (ECG) and pulse oximetry (SpO2) was attached. Patient’s baseline BP was 130/84 mmHg, HR 96/min and SpO2 98% on air. He was preloaded with 500 ml of Ringer’s lactate via 18G peripheral intravenous cannula. After taking full aseptic precautions lumbar puncture was done in L4-5 interspace using 25G Quincke spinal needle in sitting position and 3 ml of 0.5% hyperbaric bupivacaine (15 mg) was injected intrathecally for subarachnoid block and the patient turned supine.
Exsanguination of both limbs was carried out by elevating both lower limbs at 45 degrees for 5 minutes. Bilateral tourniquets with Esmarch bandage of 6 inch width were applied with three and a half wraps simultaneously at middle of thighs (pneumatic tourniquets were not available). Two surgical teams operated simultaneously and the surgery lasted for 90 min. Intraoperatively 2 lit of Ringers’ lactate was administered, urinary output was 400 ml and vital parameters remained stable throughout. After completion of the surgery, both tourniquets were released simultaneously with a tourniquet time of 1 ½ hours and rate of intravenous infusion was increased.
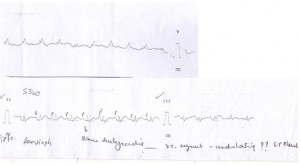
After 5 minutes of tourniquet release sudden severe hypotension (systolic BP<70 mmHg) occurred, pulses becoming feeble, and SpO2 becoming unrecordable. Inj. mephentermine 15 mg was given and the patient was oxygenated but he went into cardiac arrest. Immediate cardiopulmonary resuscitation (CPR) was started (intubation, ventilation, chest compression). Inj. adrenaline, atropine, and dopamine, adrenaline and noradrenaline infusions, and sodium bicarbonate 50 ml were given. Ringer lactate and hydroxyethyl starch were pushed IV. Patient was revived after 30 minutes of continuous CPR. After revival ECG showed atrioventricular re-entrant tachycardia (HR≥140 bpm, undulating ST segment, wide QRS and intermittent ventricular premature beats (Figure 1). Arterial blood gas analysis showed metabolic acidosis and hyperkalemia (pH 7.23, PO2 143 mmHg, PCO2 42 mmHg, base excess 9.7 mmol/l, HCO3─ 17.2 mmol/l and potassium 5.6 mmol/l). He was unconscious but spontaneous respiration with inadequate tidal volume was present. BP was then 70/40 mmHg and HR 140-150/min on vasopressor support (inj. dopamine, adrenaline and noradrenaline infusions)
Figure 1: The trace of ECG of the patient
He was shifted to ICU; vasopressor and ventilatory support (SIMV mode, tidal volume 500 ml, respiratory rate 15/min) were continued. Sodium bicarbonate 50 ml was repeated. Patient became conscious after 10 hours. Ventilatory and vasopressor supports were gradually weaned off overnight, he was extubated the next morning (after 24 hours) and discharged after 7 days with complete recovery.
DISCUSSION
Tourniquets are useful aids for orthopaedic surgical procedures on extremities, as they provide a relatively bloodless surgical field and decrease the blood loss during surgery if used properly.1 Tourniquet application on a muscular leg causes interruption of blood supply and muscle ischemia which leads to cellular hypoxia, tissue acidosis, accumulation of lactate, toxic metabolites, intracellular mediators, cytokines and free oxygen radicals. Muscle damage results in release of myoglobin, creatinine phosphokinase and potassium.9,10 After release of tourniquets these toxic mediators enter the blood circulation and may cause complications. Most of the times, the changes in circulation are transient and unnoticeable but sometimes may result in reperfusion syndrome characterised by hypotension, metabolic acidosis, hyperkalemia, myoglobinemia, myoglobinuria, renal failure, arrhythmias and even cardiac arrest.5,8
Esmarch tourniquet which is a rubber band wrapped around the extremity to exsanguinate the blood and tied at the proximal end is capable of generating very high pressures and shearing forces, leading to skin trauma, nerve injury, and even fatal complications like pulmonary embolism.11 To overcome these shortcomings, the pneumatic tourniquet was introduced in 1904 by Harvey Cushing.13 The complications with these tourniquets are less frequent if proper inflation pressures and tourniquet times are observed. However, many centres in developing countries including ours still use Esmarch bandages as tourniquet because of unavailability of pneumatic tourniquets.
Orthopedic surgeons generally use fixed tourniquet inflation pressures (typically 250 mmHg for upper arm and 300 mmHg for thigh) or +100 mmHg for upper arm and 100-150 mmHg for thigh above systolic arterial pressure.14 But recently limb occlusion pressure (LOP) has been utilized to calculate the tourniquet inflation pressure by the AORN (Association of Perioperative Registered Nurses).12 It is the pressure in the tourniquet at which the distal arterial blood flow, as assessed by a Doppler probe held over a distal artery, is occluded. This value is generally higher than the SBP. The AORN guidelines recommend that the tourniquet be inflated intraoperatively to a pressure higher than the LOP.12 A safety margin is added to cover intraoperative fluctuations in arterial pressure. If LOP is <130 mmHg, the safety margin is 40 mmHg; for LOP 131-190 mmHg, the margin is 60 mmHg; and if LOP is >190 mmHg, the margin is 80 mmHg.12 It is recommended that the tourniquet should be inflated according to the LOP and should be deflated after 2 hours for the lower limb and after 1½ hours for the upper limb for at least 10 minutes.
In the present case, occurrence of hypotension and cardiac arrest approximately 5 minutes after tourniquet release coupled with the elevated serum potassium level and metabolic acidosis support the etiology to be reperfusion injury following simultaneous release of bilateral thigh tourniquets. In this case tourniquet pressure could not be assessed since Esmarch bandages were in use. Use of Esmarch bandage as tourniquets may result in inconsistent or high pressure.15 Though tourniquet time was 90 min, not crossing the recommended time limit of 2 hours for lower limb but bilateral tourniquet application for 90 min and their simultaneous release could have resulted in massive return of toxic metabolites to circulation leading to reperfusion syndrome manifesting.
Haung et al ( 2012 )5 reported a case of 54 year old healthy male, in which cardiac arrest occurred 5 min after tourniquet deflation in tibial plateau fracture surgery under general anesthesia who was resuscitated successfully. In this case tourniquet pressure was 300 mmHg and inflation time was 2 hours and 12 min. Cardiac arrest was attributed to reperfusion injury due to tourniquet release after prolonged inflation time. Circulating mediators have also been implicated in causing a degree of coronary vasospasm8 with ECG changes which can rapidly revert on resuscitation as observed in our case and also observed by others.5
Lynn et al16 assessed the hemodynamic and metabolic effects of deflation of pneumatic tourniquets in 15 children, 7 of which had bilateral tourniquet application. They observed that larger increase in lactate level was seen with longer tourniquet inflation times (>75 min) or with bilateral tourniquets. The greatest decrease in pH was seen with simultaneous deflation of bilateral tourniquets. Caroline et al17 discussed about bilateral tourniquet use and reported that if bilateral tourniquets are used, each tourniquet should be deflated 30-45 min apart to lessen the potential for adverse patient reaction. Inflation of both tourniquets at the same time may considerably increase the afterload for the left ventricle and expose the patients to a significant upsurge of procoagulants once the tourniquets are released.18 This potential complication can be avoided by doing the bilateral procedures without the application of tourniquet or avoiding the simultaneous release of bilateral tourniquets.
In our case, simultaneous release of bilateral tourniquet might have caused reperfusion syndrome and cardiac arrest. Aggressive management with CPR resulted in revival and complete recovery of the patient.
Tourniquets produce local rheologic changes resulting in venous thrombosis which subsequently embolise on tourniquet release8. It has been reported that there is 100% incidence of asymptomatic or non-fatal pulmonary emboli and 27% incidence of grade 3 embolic (leading to cardiopulmonary impairment).19,20 Pulmonary embolism presents as pleuritic chest pain, dyspnea, and altered blood gases, and can be confirmed with pulmonary arteriography, a ventilation/perfusion scan or echocardiography.4 Cardiac arrest secondary to massive pulmonary embolism is rarely reversible by conventional resuscitative measures. Specific therapy like thrombolysis or surgical embolectomy might improve the prognosis.6
In our hospital, facilities like transesophageal echocardiography (TEE) and portable transthoracic echocardiography are not available that could show evidence of pulmonary embolism in this case. However absence of any specific symptoms of pulmonary embolism and rapid patient recovery without any specific treatment for embolism excludes the possibility of pulmonary embolism in present case.
CONCLUSION
After ruling out other common triggers, the most likely explanation of sudden hypotension and cardiac arrest in our case is reperfusion syndrome that occurred following simultaneous release of bilateral tourniquets. Moreover, Esmarch bandages used in this case might have generated significantly high pressure, further contributing to the noticed complication.
We conclude that the use of Esmarch bandages as tourniquets, especially on more than one limb simultaneously and their simultaneous release, may cause adverse cardiac events, hence must be avoided.
REFERENCES
- Tetro AM, Rudan JF. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Can J Surg 2011;44:33-38 [PubMed] [Free full text]
- Noordin S, McEwen JA, Colonel Kragh, Jr., Andrew Eisen and Bassam A. Surgical Tourniquets in Orthopaedics. J Bone Joint Surg Am 2009;91:2958-2967 [PubMed] doi: 10.2106/JBJS.I.00634.
- Murphy CG, Winter DC, Bouchier- Hayes DJ. Tourniquet injuries: Pathogenesis and modalities for attenuation. Acta Orthop Belg 2005;71:635-645 [PubMed] [Free full text]
- Kiran EK, Malhotra R, Bhan S. Unilateral vs. one stage bilateral total knee replacement in rheumatoid and osteoarthritis – A comparative study. Indian J Orthop 2005;39(1):14-20 [Free full text]
- Houng WR, Lee CL, Chiou HM, Wei YS. Cardiac arrest after tourniquet deflation in tibial plateau fracture surgery in a healthy man – a case report. Formosan Journal of Musculoskeletal Disorders 2012;3:34-38
- Bharti N, Mahajan S. Massive pulmonary embolism leading to cardiac arrest after tourniquet deflation following lower limb surgery. Anesthesia and Intensive Care 2009;37(5) Available on http://www.biomedsearch.com/article/Massive-pulmonary-embolism-leading-to/208535211.html [Accessed on 23/7/13]
- Cohen JD, Keslin JS, Nili M, Yosipovitch Z, Gassner S. Massive pulmonary embolism and tourniquet deflation- a case report. Anesth Analg 1994;79:583-585 [PubMed]
- Satoh J, Arakawa J, Ohmori H, Takahashi H, Yamakage M, Namiki A. Intraoperative cardiac arrest due to coronary vasospasm after tourniquet release–a case report. Masui. 2006;55(4):460-463. [PubMed]
- Broom MA, Rimmer C, Paris MR. Tourniquet- associated cardiac ischaemia in healthy patient undergoing trauma hand surgery. Eur J Anaesthesiol 2007;28(8);729-730
- Klenerman L. The Tourniquet Manual: Principles and Practice. London: Springer; 2003 Available on http://elib.fk.uwks.ac.id/asset/archieve/e-book/TRAUMATOLOGY/The%20Tourniquet%20 Manual-Principles%20and%20Practice.pdf [Accessed on 23/7/13]
- Lu CW, Chen YS, Wang MJ. Massive pulmonary embolism after application of an Esmarch bandage. Anesth Analg 2004;98:1187-9. [PubMed]
- AORN Committee. Recommended practices for the use of the pneumatic tourniquet in the perioperative practice setting. AORN J. 2007;86:640–55 [PubMed]
- Murphy CG, Winter DC, Bouchier-Hayes DJ. Tourniquet injuries: pathogenesis and modalities for attenuation. Acta Orthop Belg 2005;71:635-45. [PubMed]
- Deloughry JL, Griffiths R. Arterial tourniquets. Continuing Education in Anesthesia. Crit Care Pain (Indian Edition) 2009;2:64-8.
- O’Connor, Caroline, Murphy, Siobhan. Journal of Perioperative Practice. Date: August, 2007;17(8) Available on http://www.biomedsearch.com/article/Pneumatic-tourniquet-use-in-perioperative/192485433.html [Accessed on 23/7/13]
- Biehl III WC, Morgan JM, Wagner Jr. FW, Gabriel RA. The Safety of the Esmarch Tournique. Foot & Ankle International 1993;14(5):278-283 [PubMed]
- Lynn AM, Fischer T, Brandford HG, Pendergrass TW. Systemic responses to tourniquets release in children. Anesth Analg 1986;65:865-72 [PubMed]
- Nilesh P,Hemant W. Morbidity and Mortality of Simultaneous Bilateral Total Knee Arthroplasty. Orthopedics 2008;31(8). Available on http://www.healio.com/orthopedics/journals/ORTHO/%7B7D939BBC-F2AA-488F-966B-2836B26811BF%7D/Morbidity-and-Mortality-of-Simultaneous-Bilateral-Total-Knee——Arthroplasty?full=1 [Accessed on 23/7/13]
- McGrath BJ, Hsia J, Boyd A, Shay P, Graeter J, Conry K. Venous embolization after deflation of lower extremity tourniquets. Anesth Analg 1994;78:349-353 [PubMed]
- Kato N, Nakanishi K, Yoshino S, Ogawa R. Abnormal echogenic findings detected by transesophageal echocardiography and cardiorespiratory impairment during total knee arthroplasty with tourniquet. Anesthesiology 2002;97(5):1123-8. [PubMed] [Free full text]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube