Sarika Sudhir Lonkar, MBBS, DNB*, Sonal Khatavkar, MBBS, DA, DNB**,
Sonali Hastir, MBBS***
*Assistant Professor; **Associate Professor; ***Resident
Department of Anesthesiology, Dr. D.Y. Patil Medical College, Hospital &Research Centre, Pimpri, Pune, Maharashtra411018(India)
Correspondence:Dr. Sarika Sudhir Lonkar, A/203 Platinum Towers, Wakad, Pune, Maharashtra 411057 (India); Cell: +91 8888814895; E-mail: sdlonkar@rediffmail.com
ABSTRACT
One lung ventilation (OLV) can be a real challenge in the paediatricpopulation,as the margin of errorsisminimum, thetime to adapt and make decisions lessens, and stress levelsincrease. Theanesthetic management of a 5 year old girl with pneumatocele and bronchopleural fistula posted for thoracotomy is described. Right sided endobronchial intubation with uncuffed PVC endotracheal tube (ETT) was used for OLV. Thoracic epidural was given forperioperative analgesia and to facilitate postoperative physiotherapy.
Key words:Bronchopleural Fistula;Respiratory Tract Fistula; Airway Management; Positive-Pressure Respiration; One-Lung Ventilation; Analgesia;Analgesia, Epidural; Pneumonectomy
Citation:Lonkar S,Khatavkar S, Hastir S. Approach to one lung ventilation during lobectomy for pneumatocele with bronchopleural fistula in a five-year-old child: A case report.Anaesth Pain & intensive Care 2015; 19(3):412-415
INTRODUCTION
The pneumatocele is a bullous emphysematous cyst caused by over distension and rupture of alveoli secondary to bacterial pneumonia or mechanical injury.1Abronchopleural fistula is a direct communication between the bronchial tree and the pleural cavity causing an air leak from the lung that may result from rupture of lung abscess, bronchus, bulla, cyst or parenchymal tissue in the pleural space, erosion of bronchus by carcinoma or chronic inflammation.2 Diagnosis is mainly clinical and the patient presents with sudden onset dyspnoea, subcutaneous emphysema, contralateral deviation of trachea and decrease of fluid level on serial radiographs of chest.2
Anesthetic concerns in patients undergoing lobectomy or pneumonectomy are; lateral position with an open chestwhich can lead to V/Q mismatch and shunt, OLV and risk of spillage of contents into healthy lung. Good analgesia is essential for maintenance of efficient respiratory function, minimizing cardiac stress, compliance with physiotherapy &early mobilization. Here we report a case of a child with pneumatocele and bronchopleural fistula for thoracotomyunder generalplus epidural anesthesia.
CASE REPORT
A 5 year old female child with a weight of 18 kg diagnosed with left sided pneumatocele and bronchopleural fistula was posted for left lobectomy and decortication of the pleura. The patient had main complaints of chronic productive cough, dyspnoea and fever for 2 months. She had history of ICU stay 2 months back in view of high grade fever and breathlessness, was diagnosed with pneumonia,and improved with parenteral antibiotics.
The preoperative interview revealed an active child with stable vital signs. She had an oxygen saturation of 94-96% on room air. She developed persistent air leak through chest drain and pneumothorax after chest drain removal.On auscultation air entry was significantly reduced in left lung.
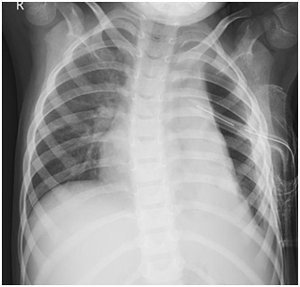
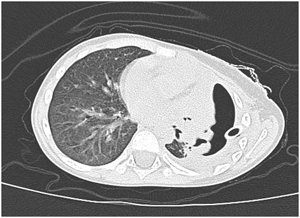
Baseline investigations (hemogram, renal and liver function tests) were within normal limits with haemoglobin of 12.5 gm %.Sputum culture didnot reveal any growth. Pre-operative arterial blood gas (ABG) values were PH-7.4, PCO2-33.3, PO2-64, and HCO3–-18.4. Chest radiography and computed tomography showed left sided hydropneumothorax, lung collapse with mediastinal and tracheal shift to right. Collapsed lung showed multiple air filled cavities of variable size and demonstration of a fistulous communication (Images 1&2).
Image 1: Preoperative chest x-ray showing left lung pneumothorax with collapse and consolidation
Image 2: Preoperative CT thorax showing left lung pneumothorax with collapse and consolidation
Elective thoracotomy was planned under general anesthesia.Due to the presence of bronchopleural fistula with pneumatocele, OLV was favored with rapid sequence endobronchial intubation.In the operating room standard monitors were attached. Right femoral vein was cannulated. Preoxygenationwas done with 100% O2.Inj. glycopyrrolate 0.04 mg, inj. fentanyl 40 mcg and inj. propofol 40 mg plus inj. succinylcholine 40 mgIV given to induce anesthesia. Rapid sequence selective right-sided endobronchial intubation wasdone with No. 5 uncuffed PVC left bevelled ETT,air entry on right sideand its absence on left sidewas confirmed and tube was fixed at 16 cm mark. 19 G epidural catheter was placed at L1-L2 level in lateral position after induction, epidural space confirmed with saline method at 1.8 cm, catheter fixed at 10 cm.
Anesthesia was maintained with sevoflurane, O2, air and atracurium. The patient was then placed in the right lateral position, supported by axillary rolls and beanbag, with the head supported by a gel donut. Placement of the ETT was verified once again via auscultation and end-tidal carbon dioxide. Patient was put on the ventilator using pressure control ventilation. Ventilator settings were maintained with apeak inspiratory pressure of 25 cmH2O; tidal volumesmaintained around 90 ml and a respiratory rate of24/min.SpO2 remained 90-94% with FiO2 of 0.5and EtCO2at 30-40 mmHg throughout the OLV of one and half hour. There was no need of additional oxygen supplementation to non-ventilated lung. Normothermia was maintained intraoperatively with warm mattress. Epidural was topped-upwith 0.125% bupivacaine+ fentanyl at fixed intervals throughout the surgery.
Left middle and partial lower lobectomy and decortication of the thickened pleurawas completed without complication. The absence of leak at suture site was confirmed by applying positive pressure ventilation after withdrawing the tube to a depth of 14 cm, re-inflation of left lung was achieved and confirmed visually on open chest with SpO2 of 100% At the endchest drain was placed. Left upper lobe expansion occurred as expected.
A total of 800 mlof crystalloid and 100 ml of colloid (6% hydroxyethyl starch 130/0.4 in 0.9% sodium chloride injection)were administered. Estimated blood loss was 100 ml. Before extubation, a chest radiograph confirmed ETTand chest tube placement, and adequate lung expansionof both left and right sides. Venous blood gasmeasurement revealed the following: pH 7.17; carbondioxide 59 mmHg; PO2 54 mmHg; base excess –7.7mEq/L; SaO2 79%; haemoglobin 11g; sodium 139 mEq/L; and potassium 3.9 mEq/L.
It was decided to extubate the child fully awake. Oxygen saturation values remained at 100% with respiratory rates varying from 24-30/min. After extubation, she was given oxygen via face mask and thentransported to the paediatric intensive care unit. Postoperatively, epidural top ups were given for 3 days with 0.125% bupivacaine plus fentanyl. Further course in the hospital was uneventful and she was discharged home on 20th day.
DISCUSSION
Anesthesia for patients with bronchopleural fistula is based on two important techniques during thoracic anesthesia: effective lung isolation and ventilation of an open airway. Prompt lung isolation is essential during anesthetic management in order to minimize the risk of ventilating the pleural cavity and soiling the contralateral lung.1
The method chosen for OLV will dependupon the type of surgery, the patient, and the surgeon preference. Lung isolation may be needed in massive haemorrhage, bronchopleural fistula, unilateral pulmonarydisease, and control of secretions during the removal ofan infected part of lung tissue.2,3The techniques toisolate a lung include a single-lumen ETT, adouble lumentube, bronchial blockers, and the Univent ETT. In infants and young children, the available sizes of the double lumen tubes or the Univent tubes do not match the anatomy of this age group. A bronchial blocker combined with a single lumen tracheal tube may be used. Fiberoptic bronchoscopy is needed to confirm the proper position of the blocker.
The simplest technique for OLV in infants and young children is to intubate the main stem bronchus of the non-operated lung by the conventional single-lumen tracheal tube.4-6 In children ETT is more likely to enter the more vertical and wider right main stem bronchus than the more obliquely placed and narrower left main stem bronchus.5 Right upper lobe obstruction is frequent after a right main stem bronchus intubation.
In this particular case, we used single lumen ETT endobronchial intubation for OLV due tothe unavailability of specialized pediatric lung isolation equipment for the concerned age category.The tracheal diameter of 18 Kg, five-year-oldgirl is expected to be around 6.5 +_1mm. The smallestDLT (Rüsch®, 26 French) and Univent tubesavailable have an outer diameter of respectively9.0 mm and 7.5 mm.Most manufacturers (Mallinckrodt®, Sheridan®) sell uncuffed ETT’s with internal diameters (ID) as small as 2.0 mm,which makes it suitable for children of all ages, including premature neonates.6
During thoracic surgery, severalfactors act to increase ventilation/perfusion (V/Q) mismatch.Compression of the dependent lung in the lateraldecubitus position may cause atelectasis. Surgical retraction and/or OLV result in collapse of the operative lung.Tidal volumes are redistributed away from the dependentlung. When spontaneous contraction of the diaphragmceases, there is increased tension on the diaphragm of thedependent lung.8 and impaired ventilation. With improper positioning, lung movement is further limited. All of these issue scontribute to an increase in the ventilation-perfusion ratio mismatch. the main change in perfusionis caused by hypoxic pulmonary vasoconstriction, which is stimulated after the onset of OLV.8 Hypoxic pulmonary vasoconstriction actually helps decrease the ventilation-perfusion mismatch from OLV by shunting blood flow away from the less oxygenated to the more oxygenate dalveoli. Hypoxic pulmonary vasoconstriction may be diminished by inhalational anesthetic agents and other vasodilating drugs.
In Pressure Control Ventilation (PCV), the ventilator generates the preset pressure during a preset inspiratory time at the preset respiratory rate. The pressure is constant during the inspiratory time and the flow is decelerating. PCV provides advantages over volume-controlled breaths: Lower peak airway pressures to deliver the same volume, better volume distribution within the lungs, better oxygenation, less risk of barotrauma, leak compensation without affecting volume delivery to the patient. The use of volume control ventilation isavoided in paediatrics because of the high risk of barotraumaand inaccurate tidal volumes delivered at so fewmillilitres per kilogram.9
The combination of GA+RA and postoperative analgesia is particularly desirable for thoracotomy especially when ICD is kept which is a source of significant pain.Also thoracic epiduralanesthesia preserves hypoxicpulmonary vasoconstriction.Although the placement of catheters in anesthetized patients is questioned, this technique is widely used by paediatricanesthesia practitioners and the incidence of neurologic injury is unknown.10 A variety of local anesthetics has been used for epidural but majority cases the use of bupivacaine has been reported.11 Epidural opioids are often combined with local anesthetic agents for maximal pain relief and also allows the use of lower concentrations of local anesthetics and thus reduces the chances of toxicity, but possibility of respiratory depression must be kept in mind.Fentanyl11 morphine and hydromorphone are currently in use for epidural administration.
CONCLUSION
Infants and children undergoing thoracic surgery pose a great challenge for the anesthesiologist.These include careful preoperative preparation, obtaining OLV in a small airway, and maintaining a delicate balance of ventilation and hemodynamics while allowing the surgeon access to avery limited intrathoracic cavity.The unique considerations forOLV in children include the typeof surgery, the patient’s anatomical and physiological conditions, surgeon preference, the anesthesia provider’scomfort level with various techniques, and the equipmentavailable in the institution.The use of regional anesthetic technique provides good results in perioperative analgesia and the recovery of pulmonary function.
REFERENCES
- Slinrger PD,Campos JH. Anaesthesia for Thoracic Surgery. Chapter in Miller’s Anaesthesia, pp.1847-1866, Seventh Edition,2010
- Hollaus PH, Lax F, el-Nashef BB, Hauck HH, Lucciarini P, Pridun NS. Natural history of bronchopleural fistula after pneumonectomy: a review of 96 cases. Ann Thorac Surg.1997 May;63(5):1391-6; discussion 1396-7.[PubMed]
- Ferreira HC, Zin WA, Rocco PRM. Physiopathology and clinical management of one-lung ventilation. J Bras Pneumol. 2004;30(5):566-573.
- Hammer GB, Fitzmaurice BG, Brodsky JB. Methods for single lung ventilation in pediatric patients. AnesthAnalg. 1999 Dec;89(6):1426-9.[PubMed]
- Muallem M, Baraka A. Aids for facilitation of difficult tracheal intubation. MEJ Anesth. 2012 Oct;21(6):785-91.[PubMed] [Free full text]
- Peeters Y, Van de Velde M, Neyrinck AP, Vermeylen K. Approach to OLV during the surgical resection of an intrathoracic ganglioneuroblastoma in a three-year-old child: A case report and review of the literature. ActaAnaesth Belg. 2014;65(1):45-9. [PubMed]
- Mattioli G, Buffa P, Granata C, Fratino G, Rossi G, Ivani G, et al. Lung resection inpediatric patients. PediatrSurg Int. 1998;13(1):10-13. [PubMed]
- Grichnik KP, Clark JA. Pathophysiology and management of one-lung ventilation. ThoracSurgClin. 2005;15(1):85-103. [PubMed]




 Facebook
Facebook Twitter
Twitter GooglePlus
GooglePlus Youtube
Youtube