Mukesh Kumar*, Kewal Krishan Gupta*, Amar Parkash Kataria**
*Assistant Professor, Department of Anaesthesiology & Intensive Care, Guru Gobind Singh Medical College& Hospital, Sadiq Rd, Kotakpura, Faridkot, Punjab 151203 (India)
**Professor, Department of Anaesthesiology & ICU, Government Medical College,Circular Road, Amritsar, Punjab 143001 (India)
Correspondence: Dr.Kewal Krishan Gupta, House No. 204, Medical Campus, Faridkot, Punjab 151203 (India); Tel: +91-9988316306; E-mail:doc_krishan31@yahoo.co.in
ABSTRACT
Aim: The aim of our study was to compare the efficacy and duration of analgesia ofcaudally administered 0.2% ropivacaine with 0.2% bupivacaine along with recovery of motor and sensory blockade in pediatric patients undergoing infraumbilical surgery.
Methodology: In this prospective, double blind study, 60 pediatric patients planned for infraumblical surgery, of ASA grade I or II, were randomly allocated in two different groups to receive 1 ml/kg of either 0.2% ropivacaine(Group A)or 0.2% bupivacaine(Group B)via caudal route after induction of general anesthesia. Objective pain score (OPS) and total duration of analgesia along with rescue analgesia were compared in both the groups. Recovery of motor and sensory blockade was also noted.The results were analyzed statistically using student’s paired t-test for inter group comparison and chi square test for non-parametric data or complications.
Result:Both the groups were comparable regarding age, weight, sex distribution and duration of surgery. Patients remained hemodynamically stable during intraoperative period in both the groups. The maximum mean sedation score at the beginning of the stay in the recovery room was 0.60 ± 0.67 and 0.67 ± 0.71 in Group A and B respectively. Though the OPS were marginallyhigher in Group B as compared to Group A but the differences in total duration and quality of analgesia were not statistically significant. Average duration of analgesia was 390.2 ± 35.16 min and 377.0 ± 34.41 min in Group A and B respectively. However, motor recovery was faster in ropivacaine group with MPS of 10.00±0.00 in comparison to 8.80±0.99 in bupivacaine group(P value <0.01) at 2 hours in postoperative period.
Conclusion:Caudal ropivacaine 0.2% is equally effective local anesthetic agent when compared to caudal bupivacaine 0.2% in terms of postoperative analgesia, but with faster motor recovery in pediatric patients.
Key words: Caudal block; Bupivacaine; Ropivacaine; Analgesia, Epidural; Analgesia
Citation: Kumar M, Gupta KK, Kataria AP. Comparison of caudal ropivacaine 0.2% with bupivacaine 0.2% in pediatric patients – a randomized controlled trial. Anaesth Pain & Intensive Care 2015;18(2):141-46
INTRODUCTION
Caudal anesthesia is commonly used in pediatric patient for pain relief following surgical procedure.[1] Wide acceptance of caudal block is due to its technical simplicity, reliability, safety and rapid performance in large series of infants and children.[2] Bupivacaine is a commonly used local anesthetic in caudal anesthesia for perioperative analgesia in perineal and lower abdominal surgeries.[3,4]
Ropivacaine is another local anesthetic recently introduced in clinical practice.It is the N-propyl homologue of bupivacaine.[5] Compared with bupivacaine which is a racemic mixture, ropivacaine is the pure S–enantiomer.[6] Ropivacaine has several properties which may be useful in pediatric practice, namely the potential to produce differential neural blockade with less motor block, and reduced cardiovascular and neurological toxicity.
We planned this randomized, prospective, double blind study to compare the quality and duration of analgesia along with motor and sensory blockafter single shot caudal block with either 0.2% ropivacaine or 0.2% bupivacaine in pediatric patients undergoing infra umbilical surgeries.Earlier studies have compared different concentrations of both the drugs like 0.25% bupivacaine with 0.2% ropivacaine or 0.25% ropivacaine, but we used a lower concentration of ropivacaine and bupivacaine i.e. 0.2%.[7-9]
METHODOLOGY
After obtaining approval from Institutional Ethical Committee and parental written informed consent, 60 pediatric patients, aged 2-8 years, of ASA grade I or II, undergoing various infraumblical surgeries like circumcision, herniotomy, rectal polyp excision or orchidopexy,were enrolled in the study. Sample size was calculated by our statistician by using power of study 70% with error of 10%.Patients were randomly allocated to one of the two groups of 30 patients each, to receive 1 ml/kg of 0.2% ropivacaine (Group A) and 0.2% bupivacaine (Group B) for caudal block. The study drugs are available in our country as 0.5% solution. We made 0.2% solution by taking 4 ml of the drug plus 6 ml of normal saline in a 10 ml syringe. Children with significant sacral deformity, local infection, coagulation defects, CNS problem and refusal of parents were excluded from the study.
After detailed preanesthetic check-up a day prior to surgery, patients were kept fasting for 4-6 hours before surgery. On the day of surgery, premedication was given with intranasal midazolam 0.2 mg/kg 30 minutes prior to surgery. In the operating room, precordial stethoscope and multichannel monitors attached for ECG, respiratory rate, noninvasive blood pressure (NIBP) and SpO2. General anesthesia was induced with halothane (1% MAC) and nitrous oxide 50% in oxygen via face mask. Intravenous cannula was placed and infusion of Isolyte-P® solution started. Intravenous atropine 0.02 mg/kg was administered as premedicant. After induction of anesthesia, airway was secured with LMA of appropriate size and patient placed in left lateral position. No systemic narcotics were administered to avoid the interference with the effect of study drugs.
After stabilization of vital signs for 5 minutes which were taken as baseline, caudal block was given with 22G short beveled needle under aseptic precautions. Position of the needle was checked using ‘whoosh test’ i.e. injecting 1 ml of air caudally and auscultating whoosh sound over the spine as per institutional protocol. After confirmation of negative aspiration of cerebrospinal fluid or blood through needle, the coded drug solution with the volume of 1 ml/kg was injected.The study was made randomized and double blind by making 60 slips which were coded. The person performing the block and carrying out the observations was blinded to the drug solution injected. Patients were moved back to supine position immediately after completion of block and vital signs were recorded. Surgery was allowed after 15 minutes of caudal block to standardize the incision time.Caudal block was considered unsuccessful if there was an increase in heart rate (>10 beats/ minute) or mean arterial blood pressure (>10 mmHg)above the baseline values following surgical incision. These patients were given intravenous fentanyl 1µg/kg and were withdrawn from study.
Table 1: Objective Pain Score
Variable |
Score |
||
0 |
1 |
2 |
|
Crying |
None |
Consolable |
Not consolable |
Movement |
None |
Restless |
Thrashing |
Agitation |
Asleep/Calm |
Mild |
Hysterical |
Posture |
Normal |
Flexed |
Holds injury site |
Verbal |
Asleep/No complaint |
Complains but cannot localize |
Complains and can localize |
Intraoperatively, vital parameters were recorded every 5 min. Postoperative parameters were recorded immediately after shifting to recovery room, then after every 30 min for 2 hours. In the ward, first reading was taken at 0 hrs and then subsequent readings were noted 2 hourly for 12 hours. During postoperative period, Objective Pain Score (OPS)[4](Table 1)in all patients and sedation score(Table 2)in children of school going age group were used to assess the severity of pain and level of sedation respectively.
Table 2: Sedation Score
|
Grade |
Definition |
|
0 |
Fully awake |
|
1 |
Slightly drowsy |
|
2 |
Asleep but easily arousable |
|
3 |
Fully asleep but arousable |
|
4 |
Fully asleep but not arousable |
Motor power was assessed by Motor Power Scale (Table 3) and level of sensory block by pin prick method in the postoperative period. Rescue analgesia was given at pain score >5, as rectal paracetamol 20mg/kg. The first and total requirement of analgesics required in the postoperative 12 hours period was noted. Side effects like nausea, vomiting, pruritus and urinary retention were also noted.
Table 3: Motor Power Scale (0 to 10)
|
Muscle Tone |
Flaccid 0 |
Hypotonia 1 |
Normal 2 |
|
Muscle power* |
Unable |
Partial |
Normal |
|
Ankle |
0 |
1 |
2 |
|
Knee |
0 |
1 |
2 |
|
Thigh |
0 |
1 |
2 |
|
Ability to stand |
0 |
1 |
2 |
Tested by ability to flex against resistance
At the end of the study decoding of the drugs was done and the results were analyzed statistically. For metric data, student’s t-test was used for intergroup comparison and chi square test was used for non-parametric data or complications. Statistical Package for Social Sciences (SPSS) and MS Excel software were used for data analysis.
RESULTS
Both the groups were comparable regarding age, weight, sex distribution and duration of surgery (Table 4).
Table 4: Patient characteristics and clinical parameters
|
Variable |
Group A |
Group B |
P value |
|
Age (Yrs) (Mean ± SD) |
5.50 ± 2.07 |
4.70 ± 2.14 |
0.147 NS |
|
Weight (Kg) (Mean ± SD) |
18.40 ± 5.12 |
17.37 ± 5.77 |
0.466 NS |
|
Sex ratio (M:F) |
25:5 |
25:5 |
- |
|
Duration of surgery(Min) (Mean ± SD) |
28.00 ± 11.79 |
26.17 ± 10.31 |
0.524 NS |
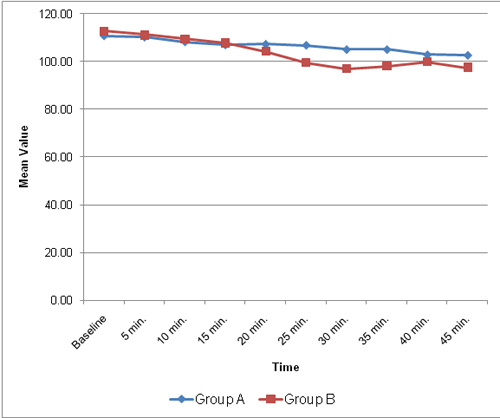
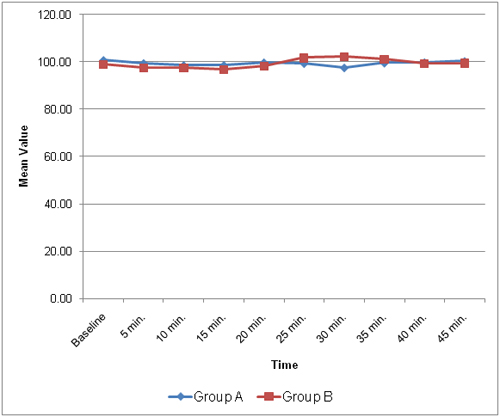
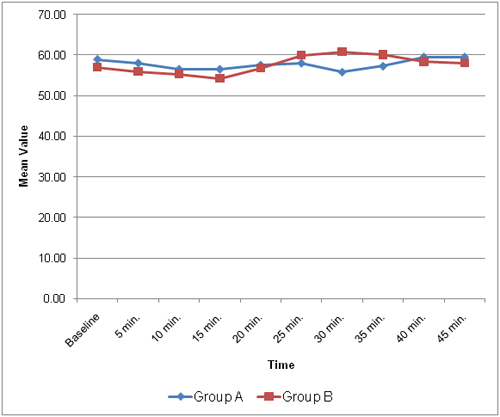
Mean HR, SBP and DBP as noted intraoperatively did not vary significantly in two groups (Figures 1 to 3).
Figure 1: Mean heart rate (per min) in the two groups during intraoperative period
Figure 2: Mean systolic blood pressure (mmHg) in the two groups during intraoperative period
Figure 3: Mean diastolic blood pressure (mmHg) in the two groups during intraoperative period
The response to incision was equivalent in both groups and there was no significant hemodynamic differences. The maximum mean sedation score at the beginning of the stay in the recovery room was 0.60 ± 0.67 and 0.67 ± 0.71 in Group A and B respectively. No significant difference was found between the sedation scores in two groups. All the patients became fully conscious within one hour.The quality and duration of postoperative pain relief did not differ significantly between the two groups. Postoperatively OPS was higher in Group B as compared to Group A at all times but the difference was statistically not significant (Table 5).Average duration of analgesia was 390.2±35.16 min and 377.0±34.41 min in Group A and B respectively. On admission to PACU, the motor power score was 7.00±1.02 in Group A and 6.67±0.96 in Group B, the difference being statistically insignificant. Complete motor power recovery was achieved at 2 hours in Group A and at 4 hours in Group B (Table 6).
Table 5: showing comparison of mean OPS between two groups during postoperative period
Observation |
OPS (Mean ± SD) |
p value |
||
Group A |
Group B |
|||
Recovery Room |
0 min | 0.40 ± 0.67 |
0.47 ± 0.73 |
0.71 |
| 30 min | 0.67 ± 0.88 |
0.73 ± 0.86 |
0.77 |
|
| 60 min | 1.03 ± 1.03 |
1.07 ± 0.98 |
0.89 |
|
| 90 min | 1.07 ± 1.04 |
1.10 ± 0.99 |
0.90 |
|
| 120 min | 1.10 ± 1.02 |
1.17 ± 1.02 |
0.80 |
|
Ward |
0 hr | 1.10 ± 1.02 |
1.17 ± 1.02 |
0.80 |
| 2 hr | 1.43 ± 0.89 |
1.70 ± 0.79 |
0.22 |
|
| 4 hr | 2.17 ± 0.74 |
2.50 ± 0.73 |
0.08 |
|
| 6 hr | 4.43 ± 1.04 |
4.53 ± 1.45 |
0.76 |
|
| 8 hr | 4.93 ± 1.79 |
4.27 ± 2.01 |
0.18 |
|
| 10 hr | 2.47 ± 1.10 |
2.53 ± 1.38 |
0.75 |
|
| 12 hr | 4.53 ± 1.04 |
4.60 ± 1.52 |
0.84 |
|
NS – Statistically not significant (p>0.05)
Table 6: Comparison of mean MPS between two groups during postoperative period
Observation |
MPS (Mean ± SD) |
p value |
|||
Group A |
Group B |
|
|||
Recovery Room |
0 min. |
7.00 ± 1.02 |
6.67 ± 0.96 |
0.197 |
|
30 min. |
7.20 ± 0.99 |
6.80 ± 0.99 |
0.125 |
||
60 min. |
7.70 ± 0.79 |
7.20 ± 0.99 |
0.036* |
||
90 min. |
8.33 ± 0.84 |
7.93 ± 0.98 |
0.096 |
||
120 min. |
10.00 ± 0.00 |
8.80 ± 0.99 |
<0.01** |
||
Ward |
0 hr |
10.00 ± 0.00 |
8.80 ± 0.99 |
<0.01** |
|
2 hr |
10.00 ± 0.00 |
10.00 ± 0.00 |
- |
||
4 hr |
10.00 ± 0.00 |
10.00 ± 0.00 |
- |
||
6 hr |
10.00 ± 0.00 |
10.00 ± 0.00 |
- |
||
8 hr |
10.00 ± 0.00 |
10.00 ± 0.00 |
- |
||
10 hr |
10.00 ± 0.00 |
10.00 ± 0.00 |
- |
||
12 hr |
10.00 ± 0.00 |
10.00 ± 0.00 |
- |
||
* P < 0.05: Significant, ** P < 0.001; Highly significant. NS – Statistically not significant (p>0.05)
Sensory blockade was satisfactory in both the groups but wore off earlier in Group A than Group B. All the patients had complete sensory recovery at 2 hours in Group A and between 2 to 4 hours in Group B.The mean number of doses of rescue analgesia required in Group A was and in Group B was 1.27 ± 0.45 and 1.43 ± 0.50 respectively,but the difference was not significant.Postoperatively, urinary retention was noted in 3(10%) in Group A and in 5(16.6%) patients in Group B. Nausea was observed in one patient in each group. No patient had vomiting, pruritus, hypotension or flushing in either group.
DISCUSSION
Pediatric regional anesthesia has gone through significant development in recent years with advances in safety, pharmacology and block techniques. There is an increased interest in regional anesthesia in pediatrics including caudal, epidural or spinal. Caudal anesthesia is a relatively simple technique with a predictable level of blockade and provides excellent postoperative analgesia. It is the most popular regional anesthetic technique used in pediatric surgery for various surgical procedures,such as lower abdominal, urological and lower limb operations. This long acting regional technique provides good postoperative analgesia with a smooth recovery period and therefore facilitates early discharge.
In our study both of the groups were homogenous with regard to age, sex, weight, duration of surgery and baseline vital parameters. Pervin et al, compared bupivacaine and ropivacaine for caudal block in children and found no changes in ECG and the heart rate and blood pressure remained stable throughout perioperative period.[7] In our study also, the variation in vital parameters in perioperative periods was comparable in both the groups and there was no significant effect on hemodynamics during perioperative period.
Ivani G et al conducted a study in 245 children to compare the analgesic effect of bupivacaine 0.25% (1 ml/kg) and ropivacaine 0.2% (1 ml/kg). The mean time to first analgesicrequirement was 233 min in bupivacaine group and 271 min in ropivacaine group.[8] Manjushree et al also noted the average duration of analgesia of 398±23 min in bupivacaine (0.25%) group and 405±18 in ropivacaine (0.25%) group, which is comparable to our results.[9]The duration of analgesia in our study was taken from the time when caudal effectiveness was achieved after giving caudal block to the time offirst rescue analgesia. In our study, the quality and duration of analgesia did not differ significantly between the two groups. The variability of duration in various studies may be due to the differences in the operations performed, calculation of analgesia time, or method of pain scoring.OPS combines the physiological and behavioural parameters and various studies indicated its reliability for assessment of pain in children.[4]
In our study, the OPS wereslightlyhigher in Group B than in Group A at all the times but this was not significant statistically. Clinically there was good analgesia in the Group A with low OPS.In a study conducted by Ray M. et al, to compare analgesic efficacy of ropivacaine and bupivacaine, the postoperative pain scores were statistically comparable in two groups in first five hours but it was significantly less in ropivacaine group after five hours.[9]
All patients showed some amount of motor weakness in both the groups immediately after surgery. But after two hours almost normal motor power was recorded in ropivacaine group as compared to bupivacaine group. Khalil et al also reported significant motor block initially which almost recovered to normal power within three hours in ropivacaine group.[10] Motor recovery was significantly slow in bupivacaine group in their series.
Sensory recovery was faster in patients of ropivacaine group in our study.The sensory recovery was complete in all the thirty patients at 2 hours in ropivacaine group as compared to twenty seven patients in bupivacaine group. The remaining three patients in the latter group recovered between 2 to 4 hours in bupivacaine group.
The requirement of rescue analgesia was comparable in both groups in our study. An earlier study also showed equivalent pain relief with two drugs.[11]The overall incidence of complications was low in our study. Martin et al found that common side effect of caudal anesthesia is urinary retention.[12] In our study 10% patients in Group A and 16.6% patients in Group B had urinary retention. None of the children in both groups were found to have respiratory difficulty and pruritus.
CONCLUSION
In conclusion, 0.2% ropivacaine provides a reliable postoperative analgesia similar to 0.2% bupivacaine in terms of quality and duration, but with shorter duration of motor blockade.Hence, ropivacaine may be a more suitable agent for day care surgery.
REFERENCES
- Dalens B.Regional anesthesia in children. Anesth Analg 1989; 68(5):654–72.[PubMed][Free Full Text]
- Markakis DA. Regional anaesthesia in pediatrics. Anesthesiol Clin North Am 2000; 18:355 – 81.[PubMed]
- Kay B. Caudal block for post-operative pain relief in children. Anaesthesia 1974; 29:610-11.[PubMed]
- Nordon J, Hannallah R, Geston P. Reliability of objective pain scale in children. Anesth Analg 1991; 72:99.
- McClure JH. Ropivacaine. Br J Anaesth 1996; 76: 300-7.[PubMed][Free Full Text]
- Mckenzie PJ, Loach AB. Local anaesthesia for orthopedic surgery. Br J Anaesth 1986; 58:779-89.[PubMed]
- Bozkurt P, Arslan I, Bakan M, Cansever MS. Free plasma levels of bupivacaine and ropivacaine when used for caudal block in children. Eur J Anaesthesiol.2005; 22:640-1.[PubMed]
- Ivani G, Lampugnani E, Torre M, Calevo Maria G.,De Negri P, Borrometi F.et al. Comparison of ropivacaine with bupivacaine for paediatric caudal block. Br J Anaesth. 1998; 81(2):247-48.[PubMed]
- Ray M, Mondal SK, Biswas A. Caudal analgesia in paediatric patients:comparison between bupivacaine and ropivacaine.Indian J Anaesth. 2003; 47:275-78.
- Khalil S, Campos C, Farag AM, Vijeh, Ritchey M, Chuang A. Caudal block in children, Ropivacaine compared with bupivacaine. Anesthesiology 1999; 91:1279-84.[PubMed][Free Full Text]
- Luz G, Innerhofer P,Haussler B. Comparison of ropivacaine 0.1% and 0.2% with bupivacaine 0.2% for single shot caudal anaesthesia in children. Pediatric Anesth 2000; 10:499-504.[PubMed]
- Martin LM, Kuebler JF, Glueer S, Suempelmann R, Ure BM and Petersen C. Penile block is associated with less urinary retention than caudal anesthesia in distal hypospadia repair in children. World J Urology 2009; 28:87-91.[Free Full Text]