Subhash1, Vipin Kumar Dhama1, Yogesh Kumar Manik2, Tanmay Tiwari2, Ganesh Singh3
1Associate Professor;2Assistant Professor
Department of Anesthesiology
3Assistant Professor (Statistician, Department of Community Medicine)
LalaLajpat Rai Memorial Medical College (LLRMC), Garh Road, Jai Bhim Nagar, Meerut, Uttar Pradesh 250004, (India)
Correspondence: Dr.
Vipin Kumar Dhama, LalaLajpat Rai Memorial Medical College (LLRMC), Garh Road, Jai Bhim Nagar, Meerut, Uttar Pradesh 250004, (India); Phone: 9760014177; E-mail: drvipindhama@yahoo.com
ABSTRACT
Objective:
Lightwand is a device which utilizes the principle of transillumination to assist endotracheal intubation.The authors evaluated the role of lightwand for nasotracheal intubation in patients having limited mouth opening on PAC assessment. Lightwand guided nasal intubation can be used for airway management where a fiberoptic bronchoscope is not always available. In elective surgery where the anesthetist has time to plan for airway management, lightwand can be an easy to use device.
Methodology:
Patients of either sexes, ASA physical status I or II, aged between 20 and 50 years, BMI (body mass index) between 18-25, and having mouth opening between 1-4 cm on PAC were included in our feasibility study. Ketofol (ketamine + propofol combination) was used to provide analgesic sedation. Lightwand was inserted into endotracheal tube and tip was bent into J shape before entering nasal cavity. Duration of procedure was calculated as the time between entry of lightwand into nose and starting of ETCO2 waveform on monitor after attaching the breathing circuit. Our study evaluated the lightwand guided nasotracheal intubation, hemodynamic changes and incidence of airway complications in 40 adult non-pregnant patients. Heart rate, systolic, diastolic and mean blood pressures were measured at 0, 1, 2, 5 and 10 min. Statistical analysis was done by using SPSS version 20. Paired T-test was used to compare all the baseline values to different time intervals.
Results:
Total time to perform intubation using lightwand was 94.44 ± 27.43 sec in our study.Hemodynamic changes (heart rate, blood pressure) in our study showed a significant increase from baseline values. Eight patients fulfilled our criteria of pain in posterior pharynx on swallowing. An equal number of patients had hoarseness of voice in post op period. In 3 patients nasotracheal intubation could not be done within 5 min (300 sec) and were excluded from the study.
Conclusion:
We conclude that lightwand may be used as an option for assisting nasotracheal intubation in patients with limited mouth opening when fiberoptic bronchoscope is not available.
Keywords: Intubation; Difficult airway; Ketamine; Lighted stylet, Lightwand; Airway management
Citation:
Subhash, Dhama VK, Manik YK, Tiwari T, Singh G. Use of lightwand for nasotracheal intubation in adult patients with limited mouth opening undergoing elective surgery. Anaesth Pain & Intensive Care 2015;19(4):468-472
INTRODUCTION
Transillumination of the tissues of the neck using a lighted stylet (lightwand) to facilitate intubation was first described by Yamamura et al in 1959.1 Since then, lightwand assisted intubation has been used in patients via oral or nasal route. Lightwand can also be used through the intubating laryngeal mask airway.2 We decided to use LightWand® lighted stylet (GE healthcare). This device is made up of a semi-rigid stylet, with a bulb at distal end, and electricity source at proximal end for lighting the bulb. Cost of this style is Indian Rs. 3700/- only.
The most important advantage of a lightwand is that it can be used via oral or nasal route to perform intubation in patients having limited mouth opening. In such situations, lightwand provides an alternative to fiberoptic bronchoscopy or blind intubation. The authors aimed to evaluate hemodynamic parameters, duration and complications of lightwand guided nasotracheal intubation.
METHODOLOGY
The authors decided to conduct a feasibility study on the use of lightwand for nasotracheal intubation at LLRM Medical College, Meerut (India) after approval by the college ethics committee from June 2014 to December 2014. Forty patients, ages between 20 and 50 years were recruited, with BMI (body mass index) 18-25. All the patients had limited mouth opening (1-4 cm). Authors did not evaluate the causes of limited mouth opening. Patients unable to cooperate with airway assessment, patients having loose teeth, intra oral infection cervical spine disease, abnormal upper airway anatomy, and patients undergoing major cardiovascular, thoracic or neurological surgery were excluded from the study. At pre-anesthesia clinic (PAC), written informed consent was obtained from the participants. Thyromental distance (in cm) was measured using a straight ruler at PAC.
After arriving in OR, heart rate, systolic, diastolic and mean arterial pressures, and SpO2 were recorded. These were taken as baseline values.
0.1% xylometazoline hydrochloride (5 drops) was put in both nostrils. Patient’s head was put in neutral position. Inj. glycopyrrolate 0.2 mg (I/M lateral thigh) was given 15 min before starting the procedure. All patients breathed oxygen via face mask (4 lit/min). They were instructed to take deep, slow breathing via mask. This was done to increase FiO2 to more than 30% while nasal preparation was done. An anesthetist observed respiratory rate on monitor and the range was 14-18 breaths per minute. Patency of the nostrils was assessed by movement of a cotton wick during inspiration and expiration placed at nose opening with one nares closed. After 2 min of oxygenation, ketamine hydrochloride (0.5 mg/kg) and propofol (2 mg/kg) were prepared in a syringe and half (50% of the total) dose was given intravenously as bolus. Unresponsiveness to painful stimuli (pressing on patients’ middle finger nail bed) was confirmed before starting insertion of endotracheal tube (ETT) into the nostril. If both nares were found equally patent then right nares was chosen. If any movement was observed of the patient’s neck or limbs during procedure, a bolus of 20% of the remaining ketofol was given.
Appropriate sized ETT was inserted till it was in the oral cavity (feeling of sudden loss of resistance). Then, overhead OR lights were switched off. The lightwand was inserted in the ETT till the fixer touched the top of ETT. Guided by light glow showing through the skin of the neck, lightwand was pushed forward, rotated to left or right until the light glow was visible in the midline of the neck just above the cricothyroid membrane. After fixing the lightwand with one hand, the ETT was glided into the trachea with the other hand and lightwand was withdrawn. After connecting the breathing circuit, chest was auscultated and EtCO2 trace was monitored to confirm the position of ETT.
Statistical analysis:
Statistical analysis was done by using SPSS version 20. Data is presented as mean ± SD. Significance level was set at p < 0.5 while using student’s t-test. Hemodynamic changes at different time intervals were compared from baseline to determine statistical significance.
RESULTS
Demographic data and airway parameters of the study group are given in Table 1.
Table 1: Patient characteristics and airway parameters of the study group (at PAC)
In 15 patients, we had to take out the lightwand and introduce again due to resistance in pushing at first attempt. In no patient, third attempt for intubation was taken (Table 2).
Twelve patients complained of pain / scratchy feeling in throat. Of these, eight patients fulfilled our criteria of pain in posterior pharynx on swallowing. Seven patients had hoarseness of voice in postop period. All patients recovered to normal voice within 48 hrs. These observations were done 1 hour after patients had an Aldrete score3 of ≥ 9. An anesthetist not involved in intraoperative management made the observations.
In 3 patients, nasotracheal intubation could not be done and the ketofol dose was completely used up (Table 2).
Table 2: Success rate and complications in the study group
Hemodynamic changes (HR, SBP, DBP and MBP) in our study showed a significant increase from baseline values. This could be a result of a sympathetic reflex due to the effect of ketamine or light plane of anesthesia. After 10 min the differences were found not to be significant (Table 3).
Table 3: Systolic blood pressure (SBP) at different time intervals
Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and heart rate (HR)
Table 4: Mean diastolic blood pressure at various time intervals
P < 0.05 is considered as significant
Table 5: Non-invasive MAP (mean) at various time intervals
Table 6: Mean heart rate at various time intervals
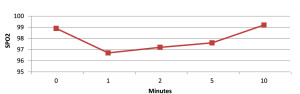 Figure 1: SpO2 (mean) at various time intervals.
Figure 1: SpO2 (mean) at various time intervals.
SpO2 was kept above 94% in every patient. In no patient SpO2 fell below 94% during the procedure.
DISCUSSION
Blind nasal intubation remains the technique for difficult airway management when a fiberoptic bronchoscope is not always available or the anesthetist is not trained in its use. Lightwand has been used in assisted oral intubation, but its use in nasal intubation is not very common. However, it has been shown to be associated with consuming less time than blind intubation in a study done by Y Dong.4 In addition, the illumination of the lightwand is not influenced by blood or secretions, so the lightwand is perhaps more effective than the fiberoptic bronchoscope in patients with active bleeding in the oral cavity following faciomaxillary trauma as stated by Agrò F.5 We chose deep sedation with spontaneous breathing to reduce the discomfort for the patients. Frizelle HP6 used 0.3 mg/kg ketamine for analgesic sedation in adult patients. Authors decided to use 0.5 mg/kg ketamine for this purpose.The approach to give 50% of total ketofol dose as initial bolus was based on author experience. Reduction in dose of these drugs when combined provides advantages of deep sedation, hemodynamic stability and analgesia.
In cases of difficulty during procedure, one or more of the following methods were adopted depending upon clinical assessment;
-external laryngeal manipulation
-extension / flexion of neck to raise the tube tip
-ETT cuff inflation to elevate the ETT tip
Above maneuvers were used in 18 out of 40 patients included in the study. An anesthesiologist with more than two years’ experience, assisted in the above maneuvers.The most important principle in lightwand guided nasotracheal intubation is “don’t force ETT against resistance”. This minimizes trauma and chances of creating false passages are also reduced.
In our study two patients had nasal bleeding during procedure. In one patients, ETT size was judged to be larger for the nares and in rest of the patients, excessive force was applied during nasal insertion of ETT. We used Aquasonic® ultrasound gel (Parker Laboratories, New Jersey, and USA) on outer surface of ETT to reduce resistance.
All patients were explained about the risk of hoarseness of voice, dysphagia and sore throat in PAC in Hindi language. After the completion of anesthetic recovery (Aldrete score > 9), they were asked about these complications. Friedman PG7 observed that lightwand intubation may decrease the incidence and severity of postoperative sore throat, hoarseness, and dysphagia in comparison to direct laryngoscopy guided intubation. Xue FS8 has shown a higher incidence of mild postoperative complications (upto 38%). This could be due to the fact that they used awake lightwand intubation in patients with difficult airway.
Some studies have shown that mallampati score, interincisive distance, and Cormack-Lehane classification of laryngoscopic view has no direct relation with nasotracheal intubation time. Manabe Y9 in their study observed no relationship between the ease of nasotracheal intubation using TrachLight™ and glottic visualization.
Increase in blood pressure and heart rate could be due to use of ketamine, inadequate anesthesia depth or long duration of procedure. Mechanical stimulation of oral / pharyngeal / laryngeal mucosa can increase sympathetic cardiovascular response. This sympathetic stimulation can increase with duration of stimulation. Reduction in intubation time with gentle manipulation of lightwand could minimize this increase. Sun Y10 have shown in their study that increase in blood pressure and heart rate occurs with a blind intubating device used for awake nasotracheal intubation. Takahashi S stated that direct stimulation of the trachea appears to be a major cause of the hemodynamic changes associated with tracheal intubation.11 The changes are almost the same as that which occur with the direct laryngoscopy.
LIMITATIONS
Limitations of our study include exclusion of pediatric and geriatric age groups. We did not evaluate the learning curve for the device use. Also, based on a study by Chung YT12, the authors placed patient heads in neutral position and not in sniffing position, so lightwand use in sniffing position was not evaluated. Ketamine-propofol combination provided satisfactory intubating conditions, however, other modalities for awake intubation can be used.
CONCLUSION
Our study shows that lightwand may be used in adult patients with limited mouth opening, where fiberoptic bronchoscopy is not available. Pharyngeal pain, hoarseness of voice and epistaxis were the complications observed in our study.
Financial Support: Department resources only
Disclaimers: None
Conflict of Interest: None
Author contribution:
SUB: Concept, conduction of study work
VKD: Concept, conduction of study work, manuscript editing
YKM: Concept, conduction of study work
TT: Conduction of study work, Manuscript editing
GS: Statistics, Manuscript editing
REFERENCES
1Associate Professor;2Assistant Professor
Department of Anesthesiology
3Assistant Professor (Statistician, Department of Community Medicine)
LalaLajpat Rai Memorial Medical College (LLRMC), Garh Road, Jai Bhim Nagar, Meerut, Uttar Pradesh 250004, (India)
Correspondence: Dr.
Vipin Kumar Dhama, LalaLajpat Rai Memorial Medical College (LLRMC), Garh Road, Jai Bhim Nagar, Meerut, Uttar Pradesh 250004, (India); Phone: 9760014177; E-mail: drvipindhama@yahoo.com
ABSTRACT
Objective:
Lightwand is a device which utilizes the principle of transillumination to assist endotracheal intubation.The authors evaluated the role of lightwand for nasotracheal intubation in patients having limited mouth opening on PAC assessment. Lightwand guided nasal intubation can be used for airway management where a fiberoptic bronchoscope is not always available. In elective surgery where the anesthetist has time to plan for airway management, lightwand can be an easy to use device.
Methodology:
Patients of either sexes, ASA physical status I or II, aged between 20 and 50 years, BMI (body mass index) between 18-25, and having mouth opening between 1-4 cm on PAC were included in our feasibility study. Ketofol (ketamine + propofol combination) was used to provide analgesic sedation. Lightwand was inserted into endotracheal tube and tip was bent into J shape before entering nasal cavity. Duration of procedure was calculated as the time between entry of lightwand into nose and starting of ETCO2 waveform on monitor after attaching the breathing circuit. Our study evaluated the lightwand guided nasotracheal intubation, hemodynamic changes and incidence of airway complications in 40 adult non-pregnant patients. Heart rate, systolic, diastolic and mean blood pressures were measured at 0, 1, 2, 5 and 10 min. Statistical analysis was done by using SPSS version 20. Paired T-test was used to compare all the baseline values to different time intervals.
Results:
Total time to perform intubation using lightwand was 94.44 ± 27.43 sec in our study.Hemodynamic changes (heart rate, blood pressure) in our study showed a significant increase from baseline values. Eight patients fulfilled our criteria of pain in posterior pharynx on swallowing. An equal number of patients had hoarseness of voice in post op period. In 3 patients nasotracheal intubation could not be done within 5 min (300 sec) and were excluded from the study.
Conclusion:
We conclude that lightwand may be used as an option for assisting nasotracheal intubation in patients with limited mouth opening when fiberoptic bronchoscope is not available.
Keywords: Intubation; Difficult airway; Ketamine; Lighted stylet, Lightwand; Airway management
Citation:
Subhash, Dhama VK, Manik YK, Tiwari T, Singh G. Use of lightwand for nasotracheal intubation in adult patients with limited mouth opening undergoing elective surgery. Anaesth Pain & Intensive Care 2015;19(4):468-472
INTRODUCTION
Transillumination of the tissues of the neck using a lighted stylet (lightwand) to facilitate intubation was first described by Yamamura et al in 1959.1 Since then, lightwand assisted intubation has been used in patients via oral or nasal route. Lightwand can also be used through the intubating laryngeal mask airway.2 We decided to use LightWand® lighted stylet (GE healthcare). This device is made up of a semi-rigid stylet, with a bulb at distal end, and electricity source at proximal end for lighting the bulb. Cost of this style is Indian Rs. 3700/- only.
The most important advantage of a lightwand is that it can be used via oral or nasal route to perform intubation in patients having limited mouth opening. In such situations, lightwand provides an alternative to fiberoptic bronchoscopy or blind intubation. The authors aimed to evaluate hemodynamic parameters, duration and complications of lightwand guided nasotracheal intubation.
METHODOLOGY
The authors decided to conduct a feasibility study on the use of lightwand for nasotracheal intubation at LLRM Medical College, Meerut (India) after approval by the college ethics committee from June 2014 to December 2014. Forty patients, ages between 20 and 50 years were recruited, with BMI (body mass index) 18-25. All the patients had limited mouth opening (1-4 cm). Authors did not evaluate the causes of limited mouth opening. Patients unable to cooperate with airway assessment, patients having loose teeth, intra oral infection cervical spine disease, abnormal upper airway anatomy, and patients undergoing major cardiovascular, thoracic or neurological surgery were excluded from the study. At pre-anesthesia clinic (PAC), written informed consent was obtained from the participants. Thyromental distance (in cm) was measured using a straight ruler at PAC.
After arriving in OR, heart rate, systolic, diastolic and mean arterial pressures, and SpO2 were recorded. These were taken as baseline values.
0.1% xylometazoline hydrochloride (5 drops) was put in both nostrils. Patient’s head was put in neutral position. Inj. glycopyrrolate 0.2 mg (I/M lateral thigh) was given 15 min before starting the procedure. All patients breathed oxygen via face mask (4 lit/min). They were instructed to take deep, slow breathing via mask. This was done to increase FiO2 to more than 30% while nasal preparation was done. An anesthetist observed respiratory rate on monitor and the range was 14-18 breaths per minute. Patency of the nostrils was assessed by movement of a cotton wick during inspiration and expiration placed at nose opening with one nares closed. After 2 min of oxygenation, ketamine hydrochloride (0.5 mg/kg) and propofol (2 mg/kg) were prepared in a syringe and half (50% of the total) dose was given intravenously as bolus. Unresponsiveness to painful stimuli (pressing on patients’ middle finger nail bed) was confirmed before starting insertion of endotracheal tube (ETT) into the nostril. If both nares were found equally patent then right nares was chosen. If any movement was observed of the patient’s neck or limbs during procedure, a bolus of 20% of the remaining ketofol was given.
Appropriate sized ETT was inserted till it was in the oral cavity (feeling of sudden loss of resistance). Then, overhead OR lights were switched off. The lightwand was inserted in the ETT till the fixer touched the top of ETT. Guided by light glow showing through the skin of the neck, lightwand was pushed forward, rotated to left or right until the light glow was visible in the midline of the neck just above the cricothyroid membrane. After fixing the lightwand with one hand, the ETT was glided into the trachea with the other hand and lightwand was withdrawn. After connecting the breathing circuit, chest was auscultated and EtCO2 trace was monitored to confirm the position of ETT.
Statistical analysis:
Statistical analysis was done by using SPSS version 20. Data is presented as mean ± SD. Significance level was set at p < 0.5 while using student’s t-test. Hemodynamic changes at different time intervals were compared from baseline to determine statistical significance.
RESULTS
Demographic data and airway parameters of the study group are given in Table 1.
Table 1: Patient characteristics and airway parameters of the study group (at PAC)
| Parameter | Mean ± SD |
| Male : female | 23 : 17 |
| Age (years) | 36.64 ± 12.041 |
| Mouth opening (cm) | 2.33 ± 0.6614 |
| MP grade | 2.16 ± 0.7177 |
| Thyromental distance (cm) | 5.28 ± 0.6712 |
Twelve patients complained of pain / scratchy feeling in throat. Of these, eight patients fulfilled our criteria of pain in posterior pharynx on swallowing. Seven patients had hoarseness of voice in postop period. All patients recovered to normal voice within 48 hrs. These observations were done 1 hour after patients had an Aldrete score3 of ≥ 9. An anesthetist not involved in intraoperative management made the observations.
In 3 patients, nasotracheal intubation could not be done and the ketofol dose was completely used up (Table 2).
Table 2: Success rate and complications in the study group
| Parameter | N (%) |
| Intubated at first attempt | 22 (55) |
| Intubated at second attempt | 15 (37.5) |
| Failed intubation | 3 (7.5) |
| Time (sec) (Mean ± SD) | 94.44 ± 27.4 |
| Pharyngeal pain | 8 (22) |
| Hoarseness of voice | 7 (19) |
| Epistaxis | 2 (5.4) |
Table 3: Systolic blood pressure (SBP) at different time intervals
| Time | Mean ± SD | P value | Smallest average difference
between pairs at 90% power |
Difference between pairs (study) |
| 0 min | 124.1 ± 12.115 | |||
| 1 min | 143.90 ± 8.595 | < 0.05 | 4.42 | 19.800 |
| 2 min | 145.10 ± 9.893 | < 0.05 | 4.70 | 21.000 |
| 5 min | 139.30 ± 9.262 | < 0.05 | 4.77 | 15.200 |
| 10 min | 121.20 ± 5.029 | > 0.05 | 4.82 | 2.900 |
Table 4: Mean diastolic blood pressure at various time intervals
| Time | Mean ± SD | P value | Smallest average difference
between pairs at 90% power |
Difference between pairs (study) |
| 0 min | 81.80 ± 5.996 | |||
| 1 min | 93.60 ± 4.971 | < 0.05 | 1.96 | 11.800 |
| 2 min | 94.2 ± 4.940 | < 0.05 | 3.31 | 12.400 |
| 5 min | 90.80 ± 2.658 | < 0.05 | 3.06 | 9.000 |
| 10 min | 77.60 ± 8.208 | > 0.05 | 3.66 | 4.200 |
Table 5: Non-invasive MAP (mean) at various time intervals
| Time | Mean ± SD | P value | Smallest average difference
between pairs at 90% power |
Difference between pairs (study) |
| 0 min | 96.40 ± 6.415 | |||
| 1 min | 110.1 ± 5.301 | < 0.05 | 2.57 | 13.700 |
| 2 min | 109.40 ± 4.575 | < 0.05 | 3.40 | 13.000 |
| 5 min | 107.0 ± 4.422 | < 0.05 | 2.76 | 10.600 |
| 10 min | 92.1 ± 4.508 | < 0.05 | 2.95 | 4.300 |
Table 6: Mean heart rate at various time intervals
| Time | Mean ± SD | P value | Smallest average difference
between pairs at 90% power |
Difference between pairs (study) |
| 0 min | 88.20 ± 6.443 | |||
| 1 min | 99.70 ± 7.484 | < 0.05 | 2.40 | 11.500 |
| 2 min | 102.1 ± 5.065 | < 0.05 | 2.17 | 13.900 |
| 5 min | 98.5 ± 3.979 | < 0.05 | 2.34 | 10.300 |
| 10 min | 80.5 ± 8.423 | < 0.05 | 4.42 | 7.700 |
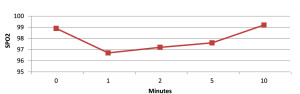 Figure 1: SpO2 (mean) at various time intervals.
Figure 1: SpO2 (mean) at various time intervals.
SpO2 was kept above 94% in every patient. In no patient SpO2 fell below 94% during the procedure.
DISCUSSION
Blind nasal intubation remains the technique for difficult airway management when a fiberoptic bronchoscope is not always available or the anesthetist is not trained in its use. Lightwand has been used in assisted oral intubation, but its use in nasal intubation is not very common. However, it has been shown to be associated with consuming less time than blind intubation in a study done by Y Dong.4 In addition, the illumination of the lightwand is not influenced by blood or secretions, so the lightwand is perhaps more effective than the fiberoptic bronchoscope in patients with active bleeding in the oral cavity following faciomaxillary trauma as stated by Agrò F.5 We chose deep sedation with spontaneous breathing to reduce the discomfort for the patients. Frizelle HP6 used 0.3 mg/kg ketamine for analgesic sedation in adult patients. Authors decided to use 0.5 mg/kg ketamine for this purpose.The approach to give 50% of total ketofol dose as initial bolus was based on author experience. Reduction in dose of these drugs when combined provides advantages of deep sedation, hemodynamic stability and analgesia.
In cases of difficulty during procedure, one or more of the following methods were adopted depending upon clinical assessment;
-external laryngeal manipulation
-extension / flexion of neck to raise the tube tip
-ETT cuff inflation to elevate the ETT tip
Above maneuvers were used in 18 out of 40 patients included in the study. An anesthesiologist with more than two years’ experience, assisted in the above maneuvers.The most important principle in lightwand guided nasotracheal intubation is “don’t force ETT against resistance”. This minimizes trauma and chances of creating false passages are also reduced.
In our study two patients had nasal bleeding during procedure. In one patients, ETT size was judged to be larger for the nares and in rest of the patients, excessive force was applied during nasal insertion of ETT. We used Aquasonic® ultrasound gel (Parker Laboratories, New Jersey, and USA) on outer surface of ETT to reduce resistance.
All patients were explained about the risk of hoarseness of voice, dysphagia and sore throat in PAC in Hindi language. After the completion of anesthetic recovery (Aldrete score > 9), they were asked about these complications. Friedman PG7 observed that lightwand intubation may decrease the incidence and severity of postoperative sore throat, hoarseness, and dysphagia in comparison to direct laryngoscopy guided intubation. Xue FS8 has shown a higher incidence of mild postoperative complications (upto 38%). This could be due to the fact that they used awake lightwand intubation in patients with difficult airway.
Some studies have shown that mallampati score, interincisive distance, and Cormack-Lehane classification of laryngoscopic view has no direct relation with nasotracheal intubation time. Manabe Y9 in their study observed no relationship between the ease of nasotracheal intubation using TrachLight™ and glottic visualization.
Increase in blood pressure and heart rate could be due to use of ketamine, inadequate anesthesia depth or long duration of procedure. Mechanical stimulation of oral / pharyngeal / laryngeal mucosa can increase sympathetic cardiovascular response. This sympathetic stimulation can increase with duration of stimulation. Reduction in intubation time with gentle manipulation of lightwand could minimize this increase. Sun Y10 have shown in their study that increase in blood pressure and heart rate occurs with a blind intubating device used for awake nasotracheal intubation. Takahashi S stated that direct stimulation of the trachea appears to be a major cause of the hemodynamic changes associated with tracheal intubation.11 The changes are almost the same as that which occur with the direct laryngoscopy.
LIMITATIONS
Limitations of our study include exclusion of pediatric and geriatric age groups. We did not evaluate the learning curve for the device use. Also, based on a study by Chung YT12, the authors placed patient heads in neutral position and not in sniffing position, so lightwand use in sniffing position was not evaluated. Ketamine-propofol combination provided satisfactory intubating conditions, however, other modalities for awake intubation can be used.
CONCLUSION
Our study shows that lightwand may be used in adult patients with limited mouth opening, where fiberoptic bronchoscopy is not available. Pharyngeal pain, hoarseness of voice and epistaxis were the complications observed in our study.
Financial Support: Department resources only
Disclaimers: None
Conflict of Interest: None
Author contribution:
SUB: Concept, conduction of study work
VKD: Concept, conduction of study work, manuscript editing
YKM: Concept, conduction of study work
TT: Conduction of study work, Manuscript editing
GS: Statistics, Manuscript editing
REFERENCES
- Yamamura H, Yamamoto T, Kamiyama M. Device for blind nasal intubation .Anesthesiology1959;20:221–2
- Kihara S,Watanabe S, Taguchi N et al .A comparison of blind and lightwand-guided tracheal intubation through the intubating laryngeal mask. Anaesthesia.2000 May;55(5):427-31.
- Aldrete JA, Kroulik D. A postanesthetic recovery score.Anesth Analg. 1970 Nov-Dec;49(6):924–934.
- Dong Y, Li G, Wu W, Su R. Lightwand-guided nasotracheal intubation in oromaxillofacial surgery patients with anticipated difficult airways: a comparison with blind nasal intubatioTop of Form International journal of oral and maxillofacial surgery September 2013;42(9):1049-1053,
- Agro F, Hung OR, Cataldo R, Carassiti M, Gherardi S. Lightwand intubation using the trachlight: a brief review of current knowledge. Can J Anaesth. 2001;48:592–599.
- Frizelle HP, Duranteau J, Samii K. A comparison of propofol with a propofol–ketamine combination for sedation during spinal anaesthesia. Anesth Analg1997;84:1318-22.
- Friedman PG, Rosenberg MK,Lebenbom-Mansour M. A comparison of light wand and suspension laryngoscopic intubation techniques in outpatients. Anesth Analg 1997;85(3):578-82.
- Xue FS, He N, Liao X, Xu XZ, et al. Clinical assessment of awake endotracheal intubation using the lightwand technique alone in patients with difficult airways. Chin Med J (Engl). 2009;122:408–415.
- Manabe Y, Seto M, Iwamoto S, Tominaga S, Taniguchi S. The success rate of nasotracheal intubation using lightwand does not depend on the laryngoscopic view. J Anesth. 2011;25:350–5.
- Sun y, Liu J, X Jiang H. Cardiovascular responses and airway complications following awake nasal intubation with blind intubation device and fibreoptic bronchoscope: a randomized controlled study. Eur J Anaesthesiol. 2010 May;27(5):461-7.
- Takahashi S, Mizutani T, Miyabe M, Toyooka H. Hemodynamic responses to tracheal intubation with laryngoscope versus lightwand intubating device (trachlight) in adults with normal airway. AnesthAnalg. 2002;95:480–4.
- Chung YT, Sun MS, Wu HS. Blind nasotracheal intubation is facilitated by neutral head position and endotracheal tube cuff inflation in spontaneously breathing patients. Can J Anaesth. 2003;50:511–3.