*Assistant Professor, Department of Surgery, Rehman Medical Institute, Peshawar (Pakistan)
**Resident; ***Associate Professor
Department of Anaesthesiology, Rehman Medical Institute, Peshawar (Pakistan)
Correspondence: Dr. Zubair Ahmad Khan,Assistant Professor, Department of Surgery, Rehman Medical Institute, Peshawar (Pakistan); Cell: +92 333 912 9360; E-mail: zubair.ahmad.khan71@gmail.com
ABSTRACT
Objectives: To document the frequency, age, gender, etiology, mortality and morbidity of patients suffering from acute pancreatitis (AP) and managed at a tertiary care hospital.
Methodology:This prospective, descriptive, institution-based study was conducted in Department of Surgery, Rehman Medical Institute (RMI), Peshawar (Pakistan), from June 2010 to June 2013. All patients with acute pancreatitis admitted to our institute were managed with a set protocol. Consecutive, non-probability sampling was done. Data were collected from all patients by a single investigator using a researcher-administered questionnaire, which included patient demographics, various risk factors, treatment options, complications and mortality.
Results: A total of 47 patients were included in the study; 28 female and 19 male patients. Out of 47 patients 35 (74%) were of Afghan origin, while 12 (26%) were Pakistani. Majority of patients (57%) were between 20-40 years of age. Gall stone pancreatitis (GSP) was the cause of AP in 13 (28%), dyslipidemia in 9 (19%), and traumatic AP in one patient, while in 24 patients (51%) it was idiopathic. Ten (21%) patients developed pseudocyst. Out of a total of 47 patients, 3 (6%) expired.
Conclusion: Patients suffering from acute pancreatitis and presenting to our hospital had a predominance of females. Majority of patients were between ages of 20-40 years. Idiopathic pancreatitis was the most common type followed by GSP. Mortality and morbidity in this study was low in comparison to other local studies.
Key words: Acute pancreatitis; Gall stone pancreatitis; Octreotide
Citation: Khan ZA, Shahab F, Khan RA. Management of acute pancreatitis: experience of a tertiary care hospital in Peshawar. Anaesth Pain & Intensive Care 2014;18(2):176-79
INTRODUCTIONAcute pancreatitis (AP) is a disease with a broad spectrum of clinical findings ranging from self-limiting mild disease to a very severe and lethal disease. It has an incidence of approximately 40 cases per 100,000 adults in the United States.1It has been observed that the incidence of acute pancreatitis is rising over the past several decades.2 It is a very lethal disease and the mortality due to pancreatitis ranges between 4% and 15% for all cases and between 15% and 90% for more severe cases.3
The etiology and pathogenesis of this disease has been studied in great detail over the past decades. Gall stone pancreatitis (GSP) and alcohol abuse are the most common causes of AP.4 There have been several descriptive studies which have shown the treatment outcomes in AP but these varied considerably due to a very broad spectrum of the severity of the disease.5
The objectives of this study were to document the frequency, age, gender, etiology, mortality and morbidity of patients suffering from acute pancreatitis that presented to a tertiary care hospital in Peshawar.
METHODOLOGY
A prospective, descriptive, institution-based study was conducted in Department of Surgery, Rehman Medical Institute (RMI), Peshawar (Pakistan); from June 2010 to June 2013. RMI is a 300-beded tertiary care hospital, which is the largest private sector hospital in Khyber Pakhtunkhwa province and receives patients from all over the province as well as from the neighboring Afghanistan.
Patients presenting with abdominal pain, raised serum amylase and lipase >3x the normal limits and diagnosed as suffering from acute pancreatitis were included in the study. Patients with abdominal pain due to all other causes were excluded from the study. Consecutive, non-probability sampling was done. Data were collected from all patients by a single investigator using a researcher-administered questionnaire which included patient demographics, various risk factors, treatment options, complications and prognosis.
The diagnosis of acute pancreatitis was made within 48 hours of admission in the surgical unit. In this regard, serum lipase estimation was considered as the most important factor because of its only source of production being the pancreas. To predict the severity and prognosis of disease, we used clinical evaluation of the cardiovascular and the respiratory systems, as well as renal function evaluation along with Ranson`s criteria, the Acute Physiology and Chronic Health Evaluation (APACHE II) score >8 and CRP >150 mg/L.
Management of Acute Pancreatitis:
After diagnosis, the management was done preferentially in our intensive care unit for the initial 48 hours and was mainly supportive; oxygen inhalation, vital sign monitoring, urinary catheterization and intake-output record. Patients were kept nil by mouth, hydrated with IV fluids, electrolyte replacement, pain relief and pancreatic rest. Antibiotics preferably imipenem were routinely given to all patients in a dose of 500 mg–1 Gm TID. Symptomatic treatment with antiemetics was added. Inj. octreotide (Sandostatin®, Novartis Pharma) 50 µg subcutaneously TID, inj. calcium gluconate 10 ml IV daily along with stress ulcer prophylaxis was also started. In severe cases with deranged liver function tests having low albumin, 20% human albumin (50-100 ml) was infused for three days. Infusion containing amino acid supplements was initiated to prevent protein catabolism. On improvement of Ranson’s criteria and APACHE scores, the patients were shifted to ward.
All patients with biliary pancreatitis underwent definitive surgical treatment of gall stones during the same hospital admission preferably in the second week, after the acute attack of pancreatitis was over. However, early ERCP for severe gall stone pancreatitis with endoscopic sphincterotomy and stenting was done in order to decompress and relieve cholangitis. In such cases, surgery was delayed till the severity of the disease subsided and the patient was advised elective surgery after 4-6 weeks.
CT scan was done in patients with persisting organ failure, signs of sepsis or deterioration in clinical status on the 4th/5th day of admission to avoid underestimation of the severity of the disease. Belthazar severity score was used and was considered as the main prognostic tool.
Data Analysis:
Data were recorded and analyzed using Statistical Package for Social Sciences v20.0 (SPSS, Inc., Chicago, IL, USA). Results were recorded as frequencies, mean ± standard deviation (SD).
RESULTS
A total of 47 patients were included in the study. There were 28 female and 19 male patients. Afghan patients constituted 74% (n=35) while Pakistani patients were 26% (n=12).
Figure 1 shows the age distribution of patients suffering from acute pancreatitis.
Figure 1: Age distribution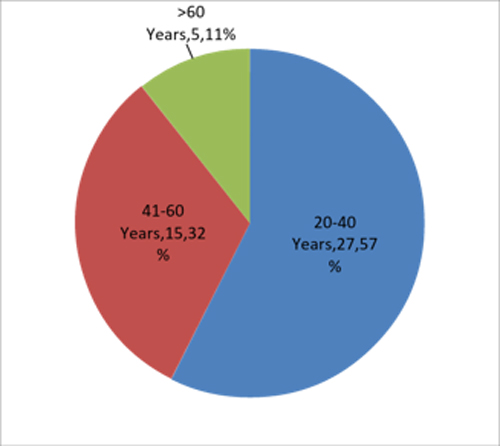
Ten patients presented in 2010, 15 patients in 2011, 14 patients in 2012 and 8 patients were admitted in 2013. GSP was the cause of AP in 13 (28%) and dyslipidemia in 9 (19%) patients. One patient had AP due to trauma while in 24 (51%) patients it was idiopathic. Table 1 shows the Ranson score on admission
Table 1: Ranson’s score|
Ranson’s score |
Patients (n) |
% |
|
1/5 |
4 |
8 |
|
2/5 |
10 |
21 |
|
3/5 |
23 |
49 |
|
4/5 |
7 |
15 |
|
5/5 |
3 |
6 |
The average duration of hospital stay was 9.8 days. Initially, all patients with Ranson’s score of 3 or more were kept in ICU for 48-72hours and on stabilization (decrease in WBC count, lipase, amylase and CRP levels) they were shifted to the ward. In 12 patients, the ICU stay was over 7 days. The initial severity of AP with Ranson’s score is shown in Table 1.
Aggressive management with recommended antibiotics and overall symptomatic treatment resulted in early diagnosis and decreased morbidity and mortality. The various morbidities developed in patients are shown in Table 2.
Table 2: Associated morbidities|
Morbidities |
Patients (n) |
% |
| Reactionary pleural effusion |
47 |
100 |
| Pseudocyst |
10 |
21 |
| Hemorrhagic pancreatitis |
3 |
6 |
| Abscess formation |
4 |
8 |
| Renal failure |
3 |
6 |
| Pancreatic necrosis |
1 |
2 |
All 3 patients with renal failure had acute hemorrhagic pancreatitis and expired. Reactionary pleural effusion occurred in almost all patients but all patients at discharge were normal except for the 3 patients who expired.
Nine patients with GSP (9/13) underwent laparoscopic/open cholecystectomy after making sure that there were no stones in CBD after appropriate imaging studies. Surgery was performed in same admission after the patient’s general condition got stabilized (average of 5 days). Four patients were referred for ERCP (sphincterotomy ± stenting) and their surgery was performed electively after 4-6 weeks.
One patient with necrosis of >30% of pancreatic tissue was debrided surgically which later on developed fistula and sepsis.
Ten (21%) patients developed pseudocysts. They were managed appropriately with U/S guided aspiration or surgery along with supportive management. All recovered well with no residual complications.
DISCUSSION
Acute pancreatitis is a common disease. The treatment modalities differ widely due to diverse etiology and pathogenesis. The management of this disease with a protocol used in our institute is presented in this study. The overall morbidity and mortality results of our study are comparable to various national and international studies.
In this study, the cause of AP could not be ascertained in 24 patients. Majority of the patients in this study were from Afghanistan, which is a war torn country with diverse cultures, ethnicity and living conditions. GSP accounted for 28% of patients in this study. In a study conducted by Qureshi et al, GSP accounted for 60% of patients.6 Asifi et al observed that gall stones accounted for 53% (24/45) of cases of acute pancreatitis in their study.7 In our study, cholecystectomy was done in all cases of GSP. Alam et al found in their quasi-experimental study that early surgery is safe and reduces hospital stay in patients with GSP.8 In a study conducted by Ong et al in New Zealand, they found that cholecystectomy for GSP is safe and results in decreased recurrence of acute pancreatitis.9 There are certain indications for which the surgery can be delayed. Nealon et al in their study concluded that cholecystectomy should be delayed in patients with severe AP who have peri-pancreatic fluid collection.10 They suggested a time interval of 6 weeks as pseudocysts would either resolve or persist by that time and in latter case cholecystectomy can be combined with pseudocyst-enterostomy. In our study, no patient suffering from GSP developed pseudocyst.
We provided antibiotic prophylaxis to all patients with imipenem. Manes et al conducted an RCT to evaluate effectiveness of meropenem and found no significant difference in comparison to imipenem.11 In a local study conducted by Khan, it was also found that antibiotic prophylaxis helps to reduce morbidity and mortality.12 Some authors have concerns regarding routine use of antibiotics for prophylaxis as it may lead to drug-resistant organisms.13 Da Costa et al found that antibiotic prophylaxis does not prevent infection of necrotic tissue but antibiotics should be specifically tailored according to bacteriological reports.14 Isenmann et al conducted a trial in which they compared ciprofloxacin/metronidazole and placebo in patients suffering from AP.15 They did not find any improvement in various parameters like systemic complications, infective necrosis and mortality rates.
Octreotide was used in all patients in this study. The role of octreotide in AP is controversial in the literature. Xu et al in a recent meta-analysis concluded that there are no added benefits of using octreotide in moderate to severe acute pancreatitis.16 A similar finding was noted in a local study conducted by Rafi et al.17 In contrast, Wang et al in a recent randomized controlled trial concluded that high dose octreotide within 48 hours of onset of AP may reduce the risk of severe acute pancreatitis as it raises plasma somatostatin levels to normal and decreases plasma levels of IL-6 and TNF-α.18 In our study, we used octreotide as part of standard treatment regimen for all patients and we had very good results.
The overall mortality in this study was 6% (3/47). One patient had necrotizing pancreatitis while 2 patients were brought to hospital in terminal stage of disease. Taj et al in their study reported mortality of 20% (11/52).19 All patients classified as severe cases by Ranson’s criteria died within one month. Asifi et al in their study observed overall mortality of 22.2% (10/45).7
There were a number of limitations in the study. There was no correlation with the levels of amylase, lipase or CRP with severity of the disease. The patients were not followed up after discharge from hospital. Further experimental studies are needed to look into efficacy of use of antibiotics, octreotide and/or early enteral feeding in patients suffering from acute pancreatitis.
CONCLUSION
Patients suffering from acute pancreatitis and presenting to our hospital had a predominance of females. Majority of patients were between ages of 20-40 years. Idiopathic pancreatitis was most common followed by GSP. Mortality and morbidity in this study was low in comparison with other local studies.
REFERENCES- Granger J, Remick D. Acute pancreatitis: models, markers, and mediators. Shock. 2005;24 Suppl 1:45-51. [PubMed]
- Singla A, Csikesz NG, Simons JP, Li YF, Ng SC, Tseng JF, et al. National hospital volume in acute pancreatitis: analysis of the Nationwide Inpatient Sample 1998-2006. HPB (Oxford). 2009;11:391-7. [PubMed][Free Full Text]
- Pitchumoni CS, Patel NM, Shah P. Factors influencing mortality in acute pancreatitis: can we alter them? J Clin Gastroenterol 2005;39:798–814. [PubMed]
- Spanier BW, Dijkgraaf MG, Bruno MJ. Epidemiology, aetiology and outcome of acute and chronic pancreatitis: An update. Best Pract Res Clin Gastroenterol 2008;22:45-63. [PubMed]
- Afzal MF, Islam HR, Majeed HJ, Ayyaz M, Azeem KM, Mirza AB. An Experience of Management of Acute Pancreatitis at Mayo Hospital Lahore. Ann King Edward Med Uni 1998;4:31-3.
- Qureshi S, Das H, Maher M. An audit of the management of acute pancreatitis in a general surgical ward. Pak J Surg 2007;23:26-8. [Free Full Text]
- Asifi M, Choudary MS, Ghazanfar A. Aetiological factors of Acute Pancreatitis. Ann King Edward Med Uni 2003;9:37-9.
- Alam T, Jamaluddin M, Tasneem B, Abbas S M. Role of surgery in acute pancreatitis associated with calculus cholecystitis. Pak J Surg 2008;24:87-91. [Free Full Text]
- Ong SK, Christie PM, Windsor JA. Management of gallstone pancreatitis in Auckland: progress and compliance. ANZ J Surg. 2003;73:194-9. [PubMed]
- Nealon WH, Bawduniak J, Walser EM. Appropriate timing of cholecystectomy in patients who present with moderate to severe gallstone-associated acute pancreatitis with peripancreatic fluid collections. Ann Surg. 2004;239:741-49. [PubMed][Free Full Text]
- Manes G, Rabitti PG, Menchise A, Riccio E, Balzano A, Uomo G. Prophylaxis with Meropenem of Septic Complications in Acute Pancreatitis: A Randomized, Controlled Trial Versus Imipenem. Pancreas: 2003;27(4):e79-e83. [PubMed]
- Khan MN. Antibiotic prophylaxis in severe acute pancreatitis. Fauji Found Health J Sep 2000;1:2-6. [Journal Abstract]
- Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology. Am J Gastroenterol 2013;108:1400-15. [PubMed]
- da Costa DW, Boerma D, van Santvoort HC, Horvath KD, Werner J, Carter CR, Bollen TL, Gooszen HG, Besselink MG, Bakker OJ. Staged multidisciplinary step-up management for necrotizing pancreatitis. Br J Surg 2014;101:e65-79. [PubMed][Free Full Text]
- Isenmann R, Runzi M, Kron M, Khal S, Kraus D, Jung N et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterol 2004;126:997–1004. [PubMed]
- Xu W, Zhou YF, Xia SH. Octreotide for primary moderate to severe acute pancreatitis: a meta-analysis. Hepatogastroenterology 2013;60:1504-8. [PubMed]
- Rafi Y, Akram B, Saqib M, Muhammad G, Muhammad Y. Octreotride in acute pancreatitis - have it or not?. Ann King Edward Med Uni 2006;12:276-8. [Journal Abstract]
- Wang R, Yang F, Wu H, Wang Y, Huang Z, Hu B, Zhang M, Tang C. High-dose versus low-dose octreotide in the treatment of acute pancreatitis: a randomized controlled trial. Peptides 2013;40:57-64. [PubMed]
- Taj A, Ghafoor MT, Amer W, Imran M, Ullah Z, Rasheed S. Mortality in patients with Acute Pancreatitis. Pak J Gastroenterol 2002;16:35-8. [Journal Abstract]