Abhijit S. Nair1, Rajendra Kumar Sahoo1, Muthuswamy Ganapathy1, Ravikiran Mudunuri1
1Department of Anesthesiology, Citizens Hospital, Serilingampally, Nalagandla Road, Hyderabad, (India)
Correspondence: Dr. Abhijit S. Nair. Department of Anesthesiology, Citizens Hospital, Serilingampally, Nalagandla Road, Hyderabad-500019, (India); Phone: +91 040 671 923 92; E-mail: abhijitnair95@gmail.com
ABSTRACT
Postoperative pain for surgeries involving chest wall is mostly managed using multimodal analgesia i.e. by using combination of non-steroidal anti-inflammatory drugs (NSAIDS), paracetamol, opioids and local anesthetic infiltration. In extensive surgeries like radical mastectomy and latissimus dorsi flaps, some anesthetists may employ use of paravertebral blocks or thoracic epidural analgesia. In this article, we describe use of ultrasound guided myofascial blocks involving chest wall that have shown to provide good analgesia after surgeries/ procedures involving the chest wall.
Key words: Nerve Blocks, Anesthesia, Local; Anesthesia, Conduction; Thoracic Nerves; Brachial Plexus; Chest Wall
Citation:Nair AS, Sahoo RK, Ganapathy M, Mudunuri R. Ultrasound guided blocks for surgeries/ procedures involving chest wall (Pecs 1, 2 and serratus plane block). Anaesth Pain & Intensive Care 2015;19(3):348-351
INTRODUCTION
Traditionally, analgesia for superficial chest wall surgeries (breast surgeries including mastectomy or implants, soft tissue excision etc.) involves a multimodal approach i.e. non- steroidal anti-inflammatory drugs (NSAIDs), opioids, paracetamol with or without local anesthetic infiltration by the surgeons. Patients having intercostal drains (ICD) are often not prescribed appropriate pain relief. Having a chest tube in situ may lead to severe excruciating pain. Patients who undergo coronary artery bypass grafting (CABG) or thoracotomy for non-cardiac surgeries have their pain score reduced by almost 60% once the ICD is removed.
Some enthusiastic anesthesiologists may use either paravertebral blocks or thoracic epidural analgesia as a strategy for pain relief in combination with multimodal analgesia. Schnabel et al did a quantitative systematic review to assess efficacy of paravertebral blocks in women undergoing breast surgeries.1 The review suggested that the quality of pain relief was excellent. The advantages of paravertebral blocks are less post-operative nausea and vomiting, less rescue analgesic requirement in first 12 hours and lower pain scores. However, the disadvantage is that, paravertebral block involves multiple level injections. Paravertebral blocks (PVB) are associated with few serious complications like; vascular puncture, epidural spread of local anesthetic, nerve damage, accidental pneumothorax and Horner’s/ Harlequins’ syndrome. The block done preoperatively with the patient remaining awake can be uncomfortable for the patient owing to injections done at multiple levels. Thoracic epidural analgesia (TEA) works well as it involves injection at single level, analgesia is predictable and continuous infusion with a catheter placement is possible. PVB or TEA is usually not practiced in superficial chest wall surgeries, the reason could be that surgeries involving chest wall are predominantly day care surgeries or the overall duration of hospital stay is usually less which doesn’t make it a feasible and cost effective mode of postoperative analgesia.
A POSSIBLE SOLUTION
The Pecs block came into the scenario to address these issues. The block is technically simple, in the lines of transverses abdominis plane (TAP) block which has turned out to be a very popular and successful block for dealing with postoperative pain after abdominal surgeries. The terminology of Pecs block was coined by Rafael Blanco. It was described in a letters to editor in the 2011 edition of Anaesthesia.2 It was an observational study for over two years which included approximately 50 patients. Blanco found this block very effective for breast cancer surgery and subpectoral prosthesis. However, the block couldn’t provide analgesia if the surgery extended to axilla (axillary dissection, radical mastectomy). So to tackle this, Blanco et al suggested an injection into another myofascial plane, this time between pectoralis minor and serratus anterior muscle at the level of 3rd and 4th rib. They called this block as modified Pecs block or Pecs block type II.3
Blanco et al studied the sonoanatomy of the chest wall further and identified two potential spaces in the lateral chest wall between serratus anterior muscle and intercostal nerve. The local anesthetic is injected after identifying serratus anterior muscle and latissimus dorsi muscle at the level of 5th rib. The block given at this level is known as serratus plane block and is a good alternative to paravertebral block or thoracic epidural anesthesia given for pain relief after surgeries involving lateral chest wall.4,5
RELEVANT ANATOMY PERTAINING TO INNERVATIONS OF CHEST:
The lateral pectoral nerve (C5, 6, 7) and median pectoral nerve (C8, T1) are the nerves relevant to Pecs 1 block. The lateral pectoral nerve is larger in size among the two and is located between pectoralis major and minor muscles in close relation to pectoral branch of thoracoacromial artery, eventually innervating the pectoralis major muscle. The median pectoral nerve passes under the pectoralis major muscle. The anterior division of thoracic intercostal nerves from T2-T6 contributes to the innervations of chest wall. The long thoracic nerve and the thoracodorsal nerve complete the innervations of chest wall along with the above mentioned nerves. The long thoracic nerve or nerve to serratus anterior (C5-C7) arises from the brachial plexus and enters the serratus anterior muscle for innervation. The thoracodorsal nerve or the nerve to latissimus dorsi arises from the posterior cord of the brachial plexus, travels along the thoracodorsal artery and innervates the latissimus dorsi muscle along the posterior wall of axilla.6-8
SEARCH STRATEGY
We’ve described the technique of Pecs and modified Pecs block with relevant sonoanatomy and have briefly reviewed the available literature by searching for words pectoral nerves, ultrasound, surgery. We searched databases like Medline, Scirus, Biomed Central, the Geneva Foundation of Medical Education and Research (GFMER). Search engines like PubMed, Scimago, Medscape and Embase were also explored. We found that the description of the block is quite recent one and the information about the efficacy is not described by randomized controlled studies. However, the information available from case report/ series and the description of technique of the block suggests that it’s a fairly easy block to perform.
THE DETAILS OF THE BLOCKS
Pecs block or the pectoral nerve block is the name given to ultrasound guided nerve block which adequately and reliably blocks the lateral and median pectoral nerves. The technique of the block is similar to transverses abdominis plane block i.e. it’s a fascial plane block and is an extension of the infraclavicular approach to the brachial plexus block. Using a curvilinear high frequency USG probe, pectoralis major and minor muscles are identified and the local anesthetic (LA) is deposited in the fascial plane between the two muscles. The block can be used for postoperative pain relief after surgeries involving breast expander and prosthesis placement, pain due to intercostal drains or for pacemaker placements. However, analgesia provided by the Pecs block was found insufficient for mastectomies and axillary dissection as several other nerves were involved during these surgeries.
After further research into sonoanatomy, a modification of Pecs block came into picture which was called Pecs 2 block or modified Pecs block. This USG guided block covers blockade of intercostobrachial nerve, intercostal nerves 3 to 6 and the long thoracic nerve which are spared with the Pecs block. In this modification, the fascial plane between pectoralis minor muscle and serratus anterior muscle is identified close to 3rd and 4th rib and local anesthetic is injected. Thus, a unilateral Pecs 1 and 2 block can provide analgesia for surgeries or procedures dealing with anterior aspect of chest.
Blanco et al continued their sono-exploration of chest wall and identified two potential spaces in the chest wall at the axillary level, with the probe in mid-axillary line. One potential space is above the serratus anterior and the other below it. After understanding Pecs 2 block, it’s easy to identify serratus anterior muscle. Other muscles which can be appreciated in this view are the latissimus dorsi and teres major muscle. The injection is given in the myofascial plane between latissimus dorsi and serratus anterior.
DESCRIPTION OF BLOCK TECHNIQUES
Figure 1: Sonoanatomy relevant to Pec block
PM- Pectoralis major muscle, Pm- Pectoralis minor muscle.
Blue arrow- myofascial plane were local anesthetic needs to be deposited by in-plane approach.
After skin preparation with 0.5% chlorhexidine w/v or by 10% povidone iodine, local anesthetic (2% lidocaine) should be injected at the point of skin entry. By careful scanning and using color Doppler, pulsations of pectoral branch of thoracoacromial artery can be identified. The needle is inserted by in-plane approach and is guided to the fascial plane between pectoralis major and minor muscle. 10 ml of local anesthetic can be injected in this plane after negative aspiration of blood. This block provides good analgesia for breast implants, chest tubes, pacemakers etc.
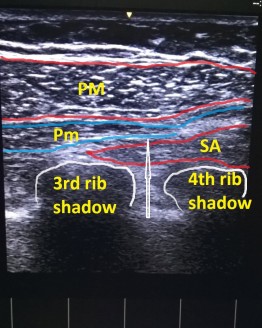
Figure 2: Sonoanatomy relevant to Pec 2 block
PM- Pectoralis major, Pm- Pectoralis minor muscle, SA- Serratus anterior muscle.
White arrow- myofascial plane were local anesthetic needs to be deposited by in-plane approach.
Skin preparation and local anesthetic infiltration should be done as described earlier. Using in-plane approach, the needle is guided to the fascial plane between pectoralis minor and serratus anterior muscle and 20 ml local anesthetic is injected after negative aspiration at the level of 4th rib. The needle is withdrawn back to reach the plane between pectoralis major and minor (Pecs 1 block) and 10 ml local anesthetic is injected here as well. This block provides good analgesia for pain due to radical mastectomies and axillary clearance.
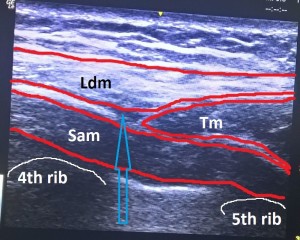
Figure 3: Sonoanatomy for serratus plane block.
Ldm: Latissimus dorsi muscle, Tm: Teres major muscle, Sam: Serratus anterior muscle.
The blue arrow is in the fascial plane were the local anesthetic has to be injected.
CONCLUSION
The Pecs 1 and 2 blocks along with serratus anterior plane block are recently described blocks which according to routine users, provide good analgesia for procedures involving anterior and anterolateral chest wall. All the 3 blocks are relatively easy to perform. Anesthesiologists who practice TAP block will find this block quite easy to master. The block is extremely helpful in day care procedures where thoracic epidural is not feasible. A successful block will automatically avoid use of opioids thereby the side-effects like nausea, vomiting, respiratory depression and constipation. However, an ultrasound machine with a linear array probe is a must for these blocks. It cannot be performed with blind or landmark techniques. Even a nerve stimulator will not be useful as it is a block given in myofascial plane. But the efficacy of the above mentioned blocks are described in a relatively small data. Therefore, we need to wait till well designed, randomized-controlled studies are conducted to demonstrate efficacy of Pecs block and serratus plane block over thoracic epidural analgesia or paravertebral blocks.
Conflict of interest: None declared by the authors.
Authors’ contribution:
ASN: Manuscript writing
AKS: Concept & design
MG: Manuscript writing
RM: Manuscript review, definition of intellectual content
REFERENCES
1Department of Anesthesiology, Citizens Hospital, Serilingampally, Nalagandla Road, Hyderabad, (India)
Correspondence: Dr. Abhijit S. Nair. Department of Anesthesiology, Citizens Hospital, Serilingampally, Nalagandla Road, Hyderabad-500019, (India); Phone: +91 040 671 923 92; E-mail: abhijitnair95@gmail.com
ABSTRACT
Postoperative pain for surgeries involving chest wall is mostly managed using multimodal analgesia i.e. by using combination of non-steroidal anti-inflammatory drugs (NSAIDS), paracetamol, opioids and local anesthetic infiltration. In extensive surgeries like radical mastectomy and latissimus dorsi flaps, some anesthetists may employ use of paravertebral blocks or thoracic epidural analgesia. In this article, we describe use of ultrasound guided myofascial blocks involving chest wall that have shown to provide good analgesia after surgeries/ procedures involving the chest wall.
Key words: Nerve Blocks, Anesthesia, Local; Anesthesia, Conduction; Thoracic Nerves; Brachial Plexus; Chest Wall
Citation:Nair AS, Sahoo RK, Ganapathy M, Mudunuri R. Ultrasound guided blocks for surgeries/ procedures involving chest wall (Pecs 1, 2 and serratus plane block). Anaesth Pain & Intensive Care 2015;19(3):348-351
INTRODUCTION
Traditionally, analgesia for superficial chest wall surgeries (breast surgeries including mastectomy or implants, soft tissue excision etc.) involves a multimodal approach i.e. non- steroidal anti-inflammatory drugs (NSAIDs), opioids, paracetamol with or without local anesthetic infiltration by the surgeons. Patients having intercostal drains (ICD) are often not prescribed appropriate pain relief. Having a chest tube in situ may lead to severe excruciating pain. Patients who undergo coronary artery bypass grafting (CABG) or thoracotomy for non-cardiac surgeries have their pain score reduced by almost 60% once the ICD is removed.
Some enthusiastic anesthesiologists may use either paravertebral blocks or thoracic epidural analgesia as a strategy for pain relief in combination with multimodal analgesia. Schnabel et al did a quantitative systematic review to assess efficacy of paravertebral blocks in women undergoing breast surgeries.1 The review suggested that the quality of pain relief was excellent. The advantages of paravertebral blocks are less post-operative nausea and vomiting, less rescue analgesic requirement in first 12 hours and lower pain scores. However, the disadvantage is that, paravertebral block involves multiple level injections. Paravertebral blocks (PVB) are associated with few serious complications like; vascular puncture, epidural spread of local anesthetic, nerve damage, accidental pneumothorax and Horner’s/ Harlequins’ syndrome. The block done preoperatively with the patient remaining awake can be uncomfortable for the patient owing to injections done at multiple levels. Thoracic epidural analgesia (TEA) works well as it involves injection at single level, analgesia is predictable and continuous infusion with a catheter placement is possible. PVB or TEA is usually not practiced in superficial chest wall surgeries, the reason could be that surgeries involving chest wall are predominantly day care surgeries or the overall duration of hospital stay is usually less which doesn’t make it a feasible and cost effective mode of postoperative analgesia.
A POSSIBLE SOLUTION
The Pecs block came into the scenario to address these issues. The block is technically simple, in the lines of transverses abdominis plane (TAP) block which has turned out to be a very popular and successful block for dealing with postoperative pain after abdominal surgeries. The terminology of Pecs block was coined by Rafael Blanco. It was described in a letters to editor in the 2011 edition of Anaesthesia.2 It was an observational study for over two years which included approximately 50 patients. Blanco found this block very effective for breast cancer surgery and subpectoral prosthesis. However, the block couldn’t provide analgesia if the surgery extended to axilla (axillary dissection, radical mastectomy). So to tackle this, Blanco et al suggested an injection into another myofascial plane, this time between pectoralis minor and serratus anterior muscle at the level of 3rd and 4th rib. They called this block as modified Pecs block or Pecs block type II.3
Blanco et al studied the sonoanatomy of the chest wall further and identified two potential spaces in the lateral chest wall between serratus anterior muscle and intercostal nerve. The local anesthetic is injected after identifying serratus anterior muscle and latissimus dorsi muscle at the level of 5th rib. The block given at this level is known as serratus plane block and is a good alternative to paravertebral block or thoracic epidural anesthesia given for pain relief after surgeries involving lateral chest wall.4,5
RELEVANT ANATOMY PERTAINING TO INNERVATIONS OF CHEST:
The lateral pectoral nerve (C5, 6, 7) and median pectoral nerve (C8, T1) are the nerves relevant to Pecs 1 block. The lateral pectoral nerve is larger in size among the two and is located between pectoralis major and minor muscles in close relation to pectoral branch of thoracoacromial artery, eventually innervating the pectoralis major muscle. The median pectoral nerve passes under the pectoralis major muscle. The anterior division of thoracic intercostal nerves from T2-T6 contributes to the innervations of chest wall. The long thoracic nerve and the thoracodorsal nerve complete the innervations of chest wall along with the above mentioned nerves. The long thoracic nerve or nerve to serratus anterior (C5-C7) arises from the brachial plexus and enters the serratus anterior muscle for innervation. The thoracodorsal nerve or the nerve to latissimus dorsi arises from the posterior cord of the brachial plexus, travels along the thoracodorsal artery and innervates the latissimus dorsi muscle along the posterior wall of axilla.6-8
SEARCH STRATEGY
We’ve described the technique of Pecs and modified Pecs block with relevant sonoanatomy and have briefly reviewed the available literature by searching for words pectoral nerves, ultrasound, surgery. We searched databases like Medline, Scirus, Biomed Central, the Geneva Foundation of Medical Education and Research (GFMER). Search engines like PubMed, Scimago, Medscape and Embase were also explored. We found that the description of the block is quite recent one and the information about the efficacy is not described by randomized controlled studies. However, the information available from case report/ series and the description of technique of the block suggests that it’s a fairly easy block to perform.
THE DETAILS OF THE BLOCKS
Pecs block or the pectoral nerve block is the name given to ultrasound guided nerve block which adequately and reliably blocks the lateral and median pectoral nerves. The technique of the block is similar to transverses abdominis plane block i.e. it’s a fascial plane block and is an extension of the infraclavicular approach to the brachial plexus block. Using a curvilinear high frequency USG probe, pectoralis major and minor muscles are identified and the local anesthetic (LA) is deposited in the fascial plane between the two muscles. The block can be used for postoperative pain relief after surgeries involving breast expander and prosthesis placement, pain due to intercostal drains or for pacemaker placements. However, analgesia provided by the Pecs block was found insufficient for mastectomies and axillary dissection as several other nerves were involved during these surgeries.
After further research into sonoanatomy, a modification of Pecs block came into picture which was called Pecs 2 block or modified Pecs block. This USG guided block covers blockade of intercostobrachial nerve, intercostal nerves 3 to 6 and the long thoracic nerve which are spared with the Pecs block. In this modification, the fascial plane between pectoralis minor muscle and serratus anterior muscle is identified close to 3rd and 4th rib and local anesthetic is injected. Thus, a unilateral Pecs 1 and 2 block can provide analgesia for surgeries or procedures dealing with anterior aspect of chest.
Blanco et al continued their sono-exploration of chest wall and identified two potential spaces in the chest wall at the axillary level, with the probe in mid-axillary line. One potential space is above the serratus anterior and the other below it. After understanding Pecs 2 block, it’s easy to identify serratus anterior muscle. Other muscles which can be appreciated in this view are the latissimus dorsi and teres major muscle. The injection is given in the myofascial plane between latissimus dorsi and serratus anterior.
DESCRIPTION OF BLOCK TECHNIQUES
- Pecs 1 block or Pecs block [Figure 1]:
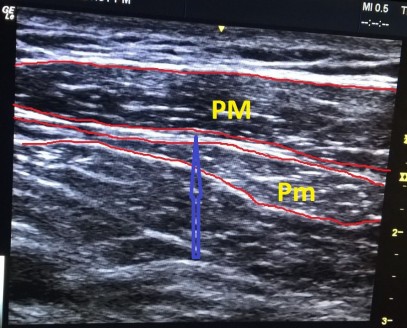
Figure 1: Sonoanatomy relevant to Pec block
PM- Pectoralis major muscle, Pm- Pectoralis minor muscle.
Blue arrow- myofascial plane were local anesthetic needs to be deposited by in-plane approach.
After skin preparation with 0.5% chlorhexidine w/v or by 10% povidone iodine, local anesthetic (2% lidocaine) should be injected at the point of skin entry. By careful scanning and using color Doppler, pulsations of pectoral branch of thoracoacromial artery can be identified. The needle is inserted by in-plane approach and is guided to the fascial plane between pectoralis major and minor muscle. 10 ml of local anesthetic can be injected in this plane after negative aspiration of blood. This block provides good analgesia for breast implants, chest tubes, pacemakers etc.
- Pecs 2 block [Figure 2]:
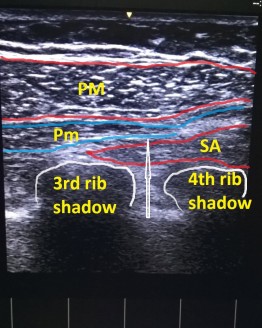
Figure 2: Sonoanatomy relevant to Pec 2 block
PM- Pectoralis major, Pm- Pectoralis minor muscle, SA- Serratus anterior muscle.
White arrow- myofascial plane were local anesthetic needs to be deposited by in-plane approach.
Skin preparation and local anesthetic infiltration should be done as described earlier. Using in-plane approach, the needle is guided to the fascial plane between pectoralis minor and serratus anterior muscle and 20 ml local anesthetic is injected after negative aspiration at the level of 4th rib. The needle is withdrawn back to reach the plane between pectoralis major and minor (Pecs 1 block) and 10 ml local anesthetic is injected here as well. This block provides good analgesia for pain due to radical mastectomies and axillary clearance.
- Serratus plane block [Figure 3]:
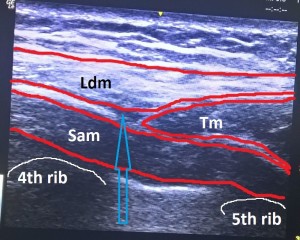
Figure 3: Sonoanatomy for serratus plane block.
Ldm: Latissimus dorsi muscle, Tm: Teres major muscle, Sam: Serratus anterior muscle.
The blue arrow is in the fascial plane were the local anesthetic has to be injected.
CONCLUSION
The Pecs 1 and 2 blocks along with serratus anterior plane block are recently described blocks which according to routine users, provide good analgesia for procedures involving anterior and anterolateral chest wall. All the 3 blocks are relatively easy to perform. Anesthesiologists who practice TAP block will find this block quite easy to master. The block is extremely helpful in day care procedures where thoracic epidural is not feasible. A successful block will automatically avoid use of opioids thereby the side-effects like nausea, vomiting, respiratory depression and constipation. However, an ultrasound machine with a linear array probe is a must for these blocks. It cannot be performed with blind or landmark techniques. Even a nerve stimulator will not be useful as it is a block given in myofascial plane. But the efficacy of the above mentioned blocks are described in a relatively small data. Therefore, we need to wait till well designed, randomized-controlled studies are conducted to demonstrate efficacy of Pecs block and serratus plane block over thoracic epidural analgesia or paravertebral blocks.
Conflict of interest: None declared by the authors.
Authors’ contribution:
ASN: Manuscript writing
AKS: Concept & design
MG: Manuscript writing
RM: Manuscript review, definition of intellectual content
REFERENCES
- Schnabel A, Reichl SU, Kranke P, Pogatzki-Zahn EM, Zahn PK. Efficacy and safety of paravertebral blocks in breast surgery: a meta- analysis of randomized controlled trials. Br J Anesth. 2010 Dec;105(6):842-52.
- Blanco R. The 'pecs block': a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011 Sep;66(9):847-8.
- Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012 Nov;59(9):470-5.
- Tighe SQ , Karmakar MK. Serratus plane block: do we need to learn another technique for thoracic wall blockade? 2013;68(11):1103-6.
- Blanco R , Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound guided thoracic wall nerve block. 2013;68(11):1107-13. [PubMed] [Free full text] doi: 10.1111/anae.12344.
- Porzionato A , Macchi V, Stecco C, Loukas M, Tubbs RS, De Caro R. Surgical anatomy of the pectoral nerves and the pectoral musculature. Clin Anat. 2012;25(5):559-75.
- David S , Balaguer T, Baque P, Peretti Fd, Valla M, Lebreton E et al. The anatomy of the pectoral nerves and its significance in breast augmentation, axillary dissection and pectoral muscle flaps. J Plast Reconstr Aesthet Surg. 2012;65(9):1193-8.
- Desroches J, Grabs U, Grabs D. Selective ultrasound guided pectoral nerve targeting in breast augmentation: How to spare the brachial plexus cords? Clin Anat. 2013;26(1):49-55.