Archana Byadarahalli Narayanappa, DA, DNB1, Shivakumar Gurulingaswamy, MD2, Umesh Nagavalli Prabhakaraiah., MD3
1Senior Resident; 2Professor & HoD; 3Assistant Professor
Department of Anesthesiology, Mandya Institute of Medical Sciences, Mandya, 571401, Karnataka (India)
Correspondence: Dr. Archana B.N, Senior Resident, Department of Anesthesia, Mandya Institute of Medical Sciences, Mandya 571401, Karnataka (India); Phone:9902358965; E-mail: drarchanabn@yahoo.co.uk.
ABSTRACT
Aims: The aim of our study was to compare the onset and duration of sensory and motor block, hemodynamic effects, neonatal outcome and adverse effects of isobaric levobupivacaine and hyperbaric bupivacaine in parturients undergoing elective lower segment cesarean section.
Methodology: Clinical records of parturients, who had undergone elective cesarean section and who had received either isobaric levobupivacaine 2 ml or hyperbaric bupivacaine 2 ml, and fulfilled inclusion and exclusion criteria were reviewed retrospectively and sorted out in two groups of 30 each. Variables investigated included demographic profile, ASA grading, block characteristics, hemodynamic parameters, neonatal apgar score and any anesthesia related complications.
Results: One hundred and forty medical records were evaluated. Demographic profile, block characteristics and anesthesia related complications were similar in both of the groups and statistically insignificant. There was more drop in systolic blood pressure in bupivacaine group at second (p=0.001) and fourth minute (p=0.006), when compared to levobupivacaine group.
Conclusion: Isobaric levobupivacaine is a good alternative to hyperbaric bupivacaine for subarachnoid block due to its better hemodynamic stability in cesarean sections.
Key words: Apgar score; Bupivacaine; Cesarean section; Levobupivacaine; Retrospective Study; Anesthesia, Spinal
Citation: Narayanappa AB, Gurulingaswamy S, Prabhakaraiah UN. A retrospective comparison of intrathecal levobupivacaine with bupivacaine for elective lower segment cesarean section. Anaesth Pain & Intensive Care 2016;20(1):26-31.
INTRODUCTION
Although use of levobupivacaine for spinal and epidural anaesthesia has been well described in literature, very few studies have examined the effects of levobupivacaine in obstetric anaesthesia.10-13 Therefore, we undertook this study in patients undergoing elective cesarean section to compare the block characteristics, hemodynamic stability, adverse effects and neonatal outcome of intrathecal isobaric levobupivacaine with hyperbaric bupivacaine.
METHODOLOGY
Standard protocols of pre-anesthetic check-up, investigations, and preoperative orders were followed. Informed consent was taken prior to surgery. On the night of surgery parturients were premedicated with oral ranitidine 150 mg. Metoclopramide 10 mg and ranitidine 50 mg were given IV one hour prior to surgery. Basic monitoring consisted of electrocardiogram (ECG), non-invasive blood pressure (NIBP) and pulse oximetry (SpO2). All patients were preloaded with 10 ml/kg of ringer’s lactate solution. Spinal anesthesia was performed in left lateral position at L2-3 or L3-4 space using 25 G Quincke spinal needle. The patients were placed supine with a left lateral tilt following the subarachnoid block. Oxygen was administered through face mask. Oxytocin 10 IU in infusion and methylergonovine maleate 200 mg IM were given to all parturients after clamping of umbilical cord.
Sensory level was assessed by pinprick sensation using a blunt 25 G needle along the mid-clavicular line bilaterally. The time to reach T10 dermatome (onset time), the maximum sensory level achieved, time for two segment (the duration of sensory block) were recorded. The motor block was assessed according to the modified Bromage scale (0 = No paralysis, able to flex hips/knees/ankles; 1 = Able to move knees, unable to raise extended legs; 2 = Able to flex ankles, unable to flex knees; 3 = Unable to move any part of the lower limb). . For motor blockade, onset time was considered as time from spinal injection to achievement of Bromage 3, whereas duration was considered as time between Bromage 3 to Bromage 0. In the intraoperative period, vital parameters (HR, SBP and Spo2) were recorded immediately after the block, every 2 min for first 10 min and every 5 min till the end of surgery.
Any complication, e.g. hypotension, bradycardia, nausea, vomiting, shivering or headache were noted and treated accordingly. A drop in SBP, of > 20% from the baseline or < 90 mmHg, was considered as hypotension and was treated with bolus of mephentermine sulphate 6 mg. A drop of heart rate (HR) > 20% or less than 50 per min was considered as bradycardia and treated with atropine 0.6 mg IV. Neonatal outcome was assessed by the Apgar score at 1 and 5 min.
The sample size was based on the duration of analgesia (mean and standard deviation) in both groups from previous studies. This was obtained after accepting an alfa error of 5% (95% confidence interval) and beta error of 20%. From this we calculated the sample size to be 30.
Data from all case records were transferred into Microsoft Excel™ for statistical analysis.
Statistical analysis: Statistical evaluation was performed by using SPSS 11.5 (SPSS Inc., Chicago, IL). Normally distributed continuous variables are expressed as mean (SD) and non-normally distributed data variables as median (range). Differences between groups were analyzed by Student’s unpaired ‘t’ test for normally distributed data. Chi-square test was used for categorical variables. The value of P < 0.05 was considered significant.
RESULTS
Demographic data in both the groups were comparable as shown in Table 1. There was no significant differences in baseline SBP and HRs, time of surgical incision or duration of surgery.
Table 1: Comparison of demographic profile of the 2 groups (Data presented as Mean ± SD)
* Time in min (from spinal injection to surgical incision)
No significant difference was found in newborn apgar scores at 1 and 5 min.
Table 2: Characteristics of intrathecal blocks in two groups (Mean ± SD)
*P value < 0.05 considered significant
The time taken to attain T10 and T6 sensory levels and time to 2-segment regression of sensory block are mentioned in Table 2. No significant differences were found between the groups regarding onset of motor block, duration of maximum motor block and regression of motor block. (Table 2).
The frequency of hypotension was significantly higher in Group B, compared to Group L [15 vs. 7 (p <0.05)] (Table 5). There was a drop in SBP at second (P = 0.001) and fourth minutes (P = 0.016) in Group B compared to Group L, which was statistically significant. Co-efficient of variation in SBP was more in Group B at 4, 10, 45 and 60 min. Difference was also found in the rest of values except in 0, 8 and 40th minute (Table 3; Figure 1). Baseline HR was comparable in both the groups (Table 4; Figure 2).
Table 3: Comparison of systolic blood pressure
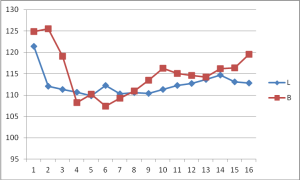 Figure 1: Comparison of systolic blood pressure
Figure 1: Comparison of systolic blood pressure
Table 4: Comparison of heart rate (beats / min)
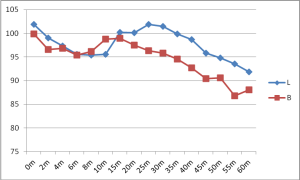
Figure 2: Comparison of heart rate
Only one patient experienced bradycardia in Group L compared to 4 patients in Group B. Nausea, vomiting and shivering were more frequent in Group B than in Group L (Table 5).
Table 5: Comparative side effects
DISCUSSION
Spinal anesthesia offers better quality of anesthesia for parturients undergoing elective cesarean section. Simplicity, rapid onset, dense neural block are its main advantages when compared to general anesthesia,1,2 however the rapid onset of sympathetic blockade may result in abrupt, severe hypotension.14 Many methods have been used to reduce hypotension, including dose reduction, use of prophylactic vasopressors, preloading with fluids and recently, use of cardiostable drugs like levobupivacaine and ropivacaine.15,16
The dose is decreased slightly for very short and obese patients, and it is increased slightly if the block is performed in the sitting position. A dosage between 7.5 - 15 mg of levobupivacaine has been used for cesarean section. Bremerich DH et al17 and Parpaglioni et al18 reported minimum effective intrathecal levobupivacaine dose to be 10 and 10.58 mg respectively in cesarean section which was similar to our observation. In our study we chose a dose of 10 mg of isobaric levobupivacaine and 10 mg of hyperbaric bupivacaine.
In our study, we did not find any significant differences in onset time, time to maximum sensory and motor block as well as duration of sensory and motor block between two groups. Similar results have been reported in earlier studies comprising of non-obstetric surgeries.19,20 Glaser et al21 compared 3.5 ml of isobaric levobupivacaine to 3.5 ml of isobaric bupivacaine in patients scheduled for elective hip replacement and found equal potency and hemodynamic stability between the two drugs. Similarly, Bay-Nielsen et al22 observed similar analgesic effects of 0.25% levobupivacaine and bupivacaine for infiltration analgesia in inguinal hernia repair. The apparent equipotency of bupivacaine and levobupivacaine reported in these studies may be explained by the large dose of local anesthetics used, which may have masked the differences in potencies.23
A potency hierarchy of intrathecal bupivacaine > levobupivacaine > ropivacaine in cesarean section patients has been confirmed in clinical studies.26,27 However, further studies regarding the efficacy and potency of local anesthetics are needed to confirm this in obstetric patients.
Besides hypotension, other common side effects like bradycardia, nausea, vomiting, shivering were more frequent in bupivacaine group compared to levobupivacaine group in our study.
LIMITATIONS
It was a retrospective study and we could not eliminate bias. Moreover, the sample size was small.
CONCLUSION
Isobaric levobupivacaine produces more hemodynamic stability when compared to hyperbaric bupivacaine, which makes it a preferable choice for spinal analgesia in cesarean sections. However, large, multi-center, prospective randomized studies are needed to establish its equipotency to confirm the differences or superiority of one drug over the other.
Conflict of interest: No sources of support and conflict of interest declared by the authors
Acknowledgement: We would like to thank Nagaraj Goud and Dr. M. Vinay, Department of Community Medicine, Mandya Institute of Medical Sciences for their kind help with statistical analysis.
Authors’ Contribution:
ABN: Concept and design of the study, retrieval and analysing the data, drafting the article, final approval of the manuscript
SG: Concept and design of the study, general supervision of the study
UNP: Retrieval and analysis of the data, drafting the manuscript
REFERENCES
1Senior Resident; 2Professor & HoD; 3Assistant Professor
Department of Anesthesiology, Mandya Institute of Medical Sciences, Mandya, 571401, Karnataka (India)
Correspondence: Dr. Archana B.N, Senior Resident, Department of Anesthesia, Mandya Institute of Medical Sciences, Mandya 571401, Karnataka (India); Phone:9902358965; E-mail: drarchanabn@yahoo.co.uk.
ABSTRACT
Aims: The aim of our study was to compare the onset and duration of sensory and motor block, hemodynamic effects, neonatal outcome and adverse effects of isobaric levobupivacaine and hyperbaric bupivacaine in parturients undergoing elective lower segment cesarean section.
Methodology: Clinical records of parturients, who had undergone elective cesarean section and who had received either isobaric levobupivacaine 2 ml or hyperbaric bupivacaine 2 ml, and fulfilled inclusion and exclusion criteria were reviewed retrospectively and sorted out in two groups of 30 each. Variables investigated included demographic profile, ASA grading, block characteristics, hemodynamic parameters, neonatal apgar score and any anesthesia related complications.
Results: One hundred and forty medical records were evaluated. Demographic profile, block characteristics and anesthesia related complications were similar in both of the groups and statistically insignificant. There was more drop in systolic blood pressure in bupivacaine group at second (p=0.001) and fourth minute (p=0.006), when compared to levobupivacaine group.
Conclusion: Isobaric levobupivacaine is a good alternative to hyperbaric bupivacaine for subarachnoid block due to its better hemodynamic stability in cesarean sections.
Key words: Apgar score; Bupivacaine; Cesarean section; Levobupivacaine; Retrospective Study; Anesthesia, Spinal
Citation: Narayanappa AB, Gurulingaswamy S, Prabhakaraiah UN. A retrospective comparison of intrathecal levobupivacaine with bupivacaine for elective lower segment cesarean section. Anaesth Pain & Intensive Care 2016;20(1):26-31.
INTRODUCTION
Although use of levobupivacaine for spinal and epidural anaesthesia has been well described in literature, very few studies have examined the effects of levobupivacaine in obstetric anaesthesia.10-13 Therefore, we undertook this study in patients undergoing elective cesarean section to compare the block characteristics, hemodynamic stability, adverse effects and neonatal outcome of intrathecal isobaric levobupivacaine with hyperbaric bupivacaine.
METHODOLOGY
Standard protocols of pre-anesthetic check-up, investigations, and preoperative orders were followed. Informed consent was taken prior to surgery. On the night of surgery parturients were premedicated with oral ranitidine 150 mg. Metoclopramide 10 mg and ranitidine 50 mg were given IV one hour prior to surgery. Basic monitoring consisted of electrocardiogram (ECG), non-invasive blood pressure (NIBP) and pulse oximetry (SpO2). All patients were preloaded with 10 ml/kg of ringer’s lactate solution. Spinal anesthesia was performed in left lateral position at L2-3 or L3-4 space using 25 G Quincke spinal needle. The patients were placed supine with a left lateral tilt following the subarachnoid block. Oxygen was administered through face mask. Oxytocin 10 IU in infusion and methylergonovine maleate 200 mg IM were given to all parturients after clamping of umbilical cord.
Sensory level was assessed by pinprick sensation using a blunt 25 G needle along the mid-clavicular line bilaterally. The time to reach T10 dermatome (onset time), the maximum sensory level achieved, time for two segment (the duration of sensory block) were recorded. The motor block was assessed according to the modified Bromage scale (0 = No paralysis, able to flex hips/knees/ankles; 1 = Able to move knees, unable to raise extended legs; 2 = Able to flex ankles, unable to flex knees; 3 = Unable to move any part of the lower limb). . For motor blockade, onset time was considered as time from spinal injection to achievement of Bromage 3, whereas duration was considered as time between Bromage 3 to Bromage 0. In the intraoperative period, vital parameters (HR, SBP and Spo2) were recorded immediately after the block, every 2 min for first 10 min and every 5 min till the end of surgery.
Any complication, e.g. hypotension, bradycardia, nausea, vomiting, shivering or headache were noted and treated accordingly. A drop in SBP, of > 20% from the baseline or < 90 mmHg, was considered as hypotension and was treated with bolus of mephentermine sulphate 6 mg. A drop of heart rate (HR) > 20% or less than 50 per min was considered as bradycardia and treated with atropine 0.6 mg IV. Neonatal outcome was assessed by the Apgar score at 1 and 5 min.
The sample size was based on the duration of analgesia (mean and standard deviation) in both groups from previous studies. This was obtained after accepting an alfa error of 5% (95% confidence interval) and beta error of 20%. From this we calculated the sample size to be 30.
Data from all case records were transferred into Microsoft Excel™ for statistical analysis.
Statistical analysis: Statistical evaluation was performed by using SPSS 11.5 (SPSS Inc., Chicago, IL). Normally distributed continuous variables are expressed as mean (SD) and non-normally distributed data variables as median (range). Differences between groups were analyzed by Student’s unpaired ‘t’ test for normally distributed data. Chi-square test was used for categorical variables. The value of P < 0.05 was considered significant.
RESULTS
Demographic data in both the groups were comparable as shown in Table 1. There was no significant differences in baseline SBP and HRs, time of surgical incision or duration of surgery.
Table 1: Comparison of demographic profile of the 2 groups (Data presented as Mean ± SD)
| Parameter | Group L
(N = 30) |
Group B
(N = 30) |
P value |
| Age | 23.57 ± 2.24 | 23.90 ±1.75 | 0.523 |
| Weight | 63.40 ± 6.44 | 62.80 ± 6.84 | 0.728 |
| 155.90 ± 3.60 | 155.97 ± 3.96 | 0.946 | |
| Baseline HR (beats per min) | 101.03 ± 18.87 | 96.73 ± 11.57 | 0.292 |
| Baseline SBP (mmHg) | 123.80 ± 13.01 | 126.83 ± 10.04 | 0.316 |
| Time of surgical incision* | 5.37 ± 0.99 | 5.43 ± 1.22 | 0.818 |
| Duration of surgery (min) | 49.63 ± 5.57 | 51.23 ±5.69 | 0.276 |
| Apgar score | 7.33 ± 0.71 | 7.62 ± 0.76 | 0.143 |
No significant difference was found in newborn apgar scores at 1 and 5 min.
Table 2: Characteristics of intrathecal blocks in two groups (Mean ± SD)
| Parameters | Group L | Group B | P value |
| Time to sensory block to T10 (min) | 1.73 ± 0.69 | 1.57 ± 0.57 | 0.312 |
| Time to sensory block to T6 (min) | 3.23 ± 0.73 | 3.03 ± 0.81 | 0.078 |
| Time to 2-Segment regression (min) | 61.97 ± 7.32 | 61.57 ± 7.70 | 0.453 |
| Regression to T10 (min) | 125.50 ± 7.35 | 126.50 ± 8.11 | 0.619 |
| Onset of Motor Block (B2) (min) | 3.33 ± 1.10 | 3.20 ± 0.85 | 0.599 |
| Max. motor block (B4) (min) | 4.30 ± 1.58 | 3.40 ± 1.07 | 0.781 |
| Time to regression of motor block (B0) (min) | 118.83 ± 12.26 | 128.33 ± 10.93 | 0.663 |
| Total duration of analgesia (min) | 129.00 ± 10.70 | 143.83 ± 10.72 | 0.453 |
The time taken to attain T10 and T6 sensory levels and time to 2-segment regression of sensory block are mentioned in Table 2. No significant differences were found between the groups regarding onset of motor block, duration of maximum motor block and regression of motor block. (Table 2).
The frequency of hypotension was significantly higher in Group B, compared to Group L [15 vs. 7 (p <0.05)] (Table 5). There was a drop in SBP at second (P = 0.001) and fourth minutes (P = 0.016) in Group B compared to Group L, which was statistically significant. Co-efficient of variation in SBP was more in Group B at 4, 10, 45 and 60 min. Difference was also found in the rest of values except in 0, 8 and 40th minute (Table 3; Figure 1). Baseline HR was comparable in both the groups (Table 4; Figure 2).
Table 3: Comparison of systolic blood pressure
| Time (min) | Group L
(Mean ± SD) |
Group B
(Mean ± SD) |
P value |
| 0 | 121.43 ± 10.42 | 124.87 ± 10.65 | 0.212 |
| 2 | 112.10 ± 14.30 | 125.50 ± 14.60 | 0.001 |
| 4 | 111.37 ± 13.84 | 119.10 ± 9.86 | 0.016 |
| 6 | 110.63 ± 14.64 | 108.27 ± 12.70 | 0.507 |
| 8 | 109.80 ± 14.75 | 110.20 ± 14.55 | 0.916 |
| 10 | 112.27 ± 10.39 | 107.43 ± 14.65 | 0.146 |
| 15 | 110.27 ± 12.00 | 109.30 ± 12.02 | 0.756 |
| 20 | 110.57 ± 10.95 | 110.97 ± 12.11 | 0.894 |
| 25 | 110.40 ± 9.88 | 113.47 ± 11.29 | 0.268 |
| 30 | 111.37 ± 9.97 | 116.30 ± 11.30 | 0.078 |
| 35 | 112.27 ± 9.04 | 115.10 ± 10.92 | 0.278 |
| 40 | 112.73 ± 9.26 | 114.60 ± 9.24 | 0.438 |
| 45 | 113.70 ± 7.26 | 114.23 ± 11.36 | 0.829 |
| 50 | 114.72 ± 6.85 | 116.20 ± 8.94 | 0.481 |
| 55 | 113.13 ± 6.63 | 116.41 ± 8.16 | 0.215 |
| 60 | 112.78 ± 6.70 | 119.57 ± 11.51 | 0.125 |
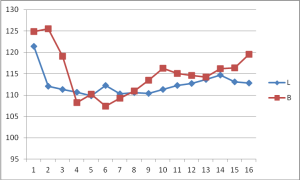 Figure 1: Comparison of systolic blood pressure
Figure 1: Comparison of systolic blood pressure
Table 4: Comparison of heart rate (beats / min)
| Time (min) | Group L
(Mean ± SD) |
Group B
(Mean ± SD) |
P value |
| 0 | 101.87 ± 21.34 | 99.87 ± 13.64 | 0.667 |
| 2 | 99.03 ± 17.54 | 96.57 ± 14.02 | 0.550 |
| 4 | 97.30 ± 18.25 | 96.83 ± 18.91 | 0.923 |
| 6 | 95.53 ± 19.75 | 95.40 ± 19.48 | 0.979 |
| 8 | 95.43 ± 20.06 | 96.17 ± 16.28 | 0.877 |
| 10 | 95.57 ± 17.93 | 98.77 ± 15.31 | 0.460 |
| 15 | 100.17 ± 16.43 | 98.93 ± 14.38 | 0.758 |
| 20 | 100.13 ± 16.67 | 97.50 ± 14.54 | 0.517 |
| 25 | 101.90 ± 15.69 | 96.33 ± 13.97 | 0.152 |
| 30 | 101.43 ± 16.37 | 95.80 ± 11.66 | 0.130 |
| 35 | 99.87 ± 15.16 | 94.53 ± 10.72 | 0.121 |
| 40 | 98.70 ± 16.06 | 92.67 ± 11.08 | 0.096 |
| 45 | 95.83 ± 15.16 | 90.43 ± 12.54 | 0.138 |
| 50 | 94.79 ± 15.39 | 90.57 ± 14.53 | 0.283 |
| 55 | 93.56 ± 17.38 | 86.76 ± 14.13 | 0.226 |
| 60 | 91.89 ± 19.56 | 88.07 ± 13.97 | 0.590 |
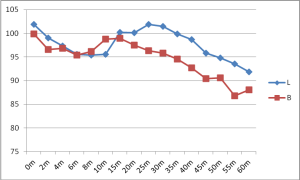
Figure 2: Comparison of heart rate
Only one patient experienced bradycardia in Group L compared to 4 patients in Group B. Nausea, vomiting and shivering were more frequent in Group B than in Group L (Table 5).
Table 5: Comparative side effects
| Side effects | Group L (n = 30) | Group B (n = 30) | ||
| Number | Percentage | Number | Percentage | |
| Hypotension | 7 | 26.6 | 15 | 50.0 |
| Bradycardia | 1 | 3.3 | 4 | 13.3 |
| Nausea /Vomiting | 5 | 16.6 | 8 | 26.6 |
| Shivering | 3 | 10.0 | 5 | 16.6 |
DISCUSSION
Spinal anesthesia offers better quality of anesthesia for parturients undergoing elective cesarean section. Simplicity, rapid onset, dense neural block are its main advantages when compared to general anesthesia,1,2 however the rapid onset of sympathetic blockade may result in abrupt, severe hypotension.14 Many methods have been used to reduce hypotension, including dose reduction, use of prophylactic vasopressors, preloading with fluids and recently, use of cardiostable drugs like levobupivacaine and ropivacaine.15,16
The dose is decreased slightly for very short and obese patients, and it is increased slightly if the block is performed in the sitting position. A dosage between 7.5 - 15 mg of levobupivacaine has been used for cesarean section. Bremerich DH et al17 and Parpaglioni et al18 reported minimum effective intrathecal levobupivacaine dose to be 10 and 10.58 mg respectively in cesarean section which was similar to our observation. In our study we chose a dose of 10 mg of isobaric levobupivacaine and 10 mg of hyperbaric bupivacaine.
In our study, we did not find any significant differences in onset time, time to maximum sensory and motor block as well as duration of sensory and motor block between two groups. Similar results have been reported in earlier studies comprising of non-obstetric surgeries.19,20 Glaser et al21 compared 3.5 ml of isobaric levobupivacaine to 3.5 ml of isobaric bupivacaine in patients scheduled for elective hip replacement and found equal potency and hemodynamic stability between the two drugs. Similarly, Bay-Nielsen et al22 observed similar analgesic effects of 0.25% levobupivacaine and bupivacaine for infiltration analgesia in inguinal hernia repair. The apparent equipotency of bupivacaine and levobupivacaine reported in these studies may be explained by the large dose of local anesthetics used, which may have masked the differences in potencies.23
A potency hierarchy of intrathecal bupivacaine > levobupivacaine > ropivacaine in cesarean section patients has been confirmed in clinical studies.26,27 However, further studies regarding the efficacy and potency of local anesthetics are needed to confirm this in obstetric patients.
Besides hypotension, other common side effects like bradycardia, nausea, vomiting, shivering were more frequent in bupivacaine group compared to levobupivacaine group in our study.
LIMITATIONS
It was a retrospective study and we could not eliminate bias. Moreover, the sample size was small.
CONCLUSION
Isobaric levobupivacaine produces more hemodynamic stability when compared to hyperbaric bupivacaine, which makes it a preferable choice for spinal analgesia in cesarean sections. However, large, multi-center, prospective randomized studies are needed to establish its equipotency to confirm the differences or superiority of one drug over the other.
Conflict of interest: No sources of support and conflict of interest declared by the authors
Acknowledgement: We would like to thank Nagaraj Goud and Dr. M. Vinay, Department of Community Medicine, Mandya Institute of Medical Sciences for their kind help with statistical analysis.
Authors’ Contribution:
ABN: Concept and design of the study, retrieval and analysing the data, drafting the article, final approval of the manuscript
SG: Concept and design of the study, general supervision of the study
UNP: Retrieval and analysis of the data, drafting the manuscript
REFERENCES
- Bucklin BA, Hawkins JL, Anderson JR, Ullrich FA. Obstetric anesthesia workforce survey: twenty year update. 2005 Sep;103(3):645–53.[PubMed] [Free full text]
- Yeoh SB, Leong SB, Heng AS. Anesthesia for lower-segment cesarean section: Changing perspectives. Indian J Anaesth. 2010 Sep;54(5):409–14.[PubMed] [Free full text] doi: 10.4103/0019-5049.71037
- Albright GA. Cardiac arrest following regional anaesthesia with etidocaine and Bupivacaine. Anaesthesiology. 1979 Oct;51(4):285-7. [PubMed] [Free full text]
- Scull TJ, Carli F. Cardiac arrest after Cesarean section under subarachnoid block. Br J Anaesth. 1996 Aug;77(2):274-6. [PubMed] [Free full text]
- Løvstad RZ, Granhus G, Hetland S. Bradycardia and asystolic cardiac arrest during spinal anaesthesia: a report of five cases. Acta Anaesthesiol Scand. 2000 Jan;44(1):48-52. [PubMed]
- Valenzuela C, Delpon E, Tamkun MM, Tamargo J,Snyders DJ. Stereoselective block of a human cardiac potassium channel (Kv5) by bupivacaine enantiomers. Biophys J. 1995 Aug;69(2):418–27. [PubMed] [Free full text]
- Valenzuela C, Snyders DJ, Bennett PB, Tamargo J,Hondeghem LM. Stereoselective block of cardiac sodium channels by bupivacaine in guinea pig ventricular myocytes. 1995 Nov 15;92(10):3014–24. [PubMed] [Free full text]
- Vanhouette F, Vereecke J, Verbeke N, Carmeliet E. Stereoselctive effects of the enantiomers of bupivacaine on the electrophysiological properties of the guinea-pig papillary muscle. Br J Pharmacol. 1991 May;103(1):1275–81. [PubMed] [Free full text]
- Bajwa SS, Kaur J. Clinical profile of Levobupivacaine in regional anesthesia: A systematic review. J Anaesthesiol Clin Pharmacol. 2013 Oct;29(4):530-9. [PubMed] [Free full text] doi: 10.4103/0970-9185.119172
- Casati A, Moizo E, Marchetti C, Vinciquerra F. A prospective, randomized,double-blind comparison of unilateral spinal anesthesia with hyperbaric bupivacaine, ropivacaine, or levobupivacaine for inguinal herniorrhaphy. Anesth Analg. 2004 Nov;99(5):1387–92. [PubMed]
- Kopacz DJ, Allen HW, Thompson GE. A comparison of epidural levobupivacaine 0.75% with racemic bupivacaine for lower abdominal surgery. Anesth Analg. 2000 Mar;90(3):642–8.[PubMed]
- Cox CR, Faccenda KA, Gilhooly C, Bannister J, Scott NB, Morrison LM. Extradural S-bupivacaine: comparison with racemic RS-bupivacaine. Br J Anaesth. 1998 Mar;80(3):289–93. [PubMed] [Free full text]
- Cox CR, Checketts MR, MacKenzie N, Scott NB, Bannister J. Comparison of S-bupivacaine with racemic (RS)-bupivacaine in supraclavicular brachial plexus block. Br J Anaesth. 1998 May;80(5):594–8. [PubMed] [Free full text]
- Krzysztof M. Kuczkowski,Laurence S. Reisner, Dennis Lin. Anaesthesia For Caesarean section, In Chestnut: Obstetric Anesthesia: Principles and Practice, 3rd edition, Chapter 25, Elsevier; 2008
- Huang YF, Pryor ME, Mather LE, Veering BT. Cardiovascular and central nervous system effects of intravenous levobupivacaine and bupivacaine in sheep. Anesth Analg. 1998 Apr;86(4):797-804. [PubMed]
- Morrison SG, Dominguez JJ, Frascarolo P, Reiz S. A comparison of the electrocardiographic cardiotoxic effects of racemic bupivacaine, levobupivacaine and ropivacaine in anesthetized swine. Anesth Analg. 2000 Jun;90(6):1308-1314.[PubMed]
- Bremerich DH, Kuschel S, Fetsch N, Zwissler B, Byhahn C, Meininger D. Levobupivacaine for parturients undergoing elective ceasarean delivery. A dose-finding investigation. Anaesthetist. 2007 Aug;56(8):772-9. [PubMed]
- Parpaglioni R, Frigo MG, Lemma A, Sebastiani M, Barbati G, Celleno D. Minimum local anaesthetic dose (MLAD) of intrathecal levobupivacaine and ropivacaine for Caesarean section. Anaesthesia. 2006 Feb;61(2):110-5. [PubMed]
- Fattorini F, Ricci Z, Rocco A, Romano R, Pascarella MA, Pinto G. Levobupivacaine versus racemic bupivacaine for spinal anaesthesia in orthopaedic major surgery. Minerva Anestesiol. 2006 Jul-Aug;72(7-8):637-44. [PubMed]
- Lee YY, Muchhal K, Chan CK. Levobupivacaine versus racemic bupivacaine in spinal anaesthesia for urological surgery. Anaesth Intensive Care. 2003 Dec;31(6):637-41. [PubMed]
- Glaser C, Marhofer P, Zimpfer G, Heinz MT, Sitzwohl C, Kapral S, et al. Levobupivacaine versus racemic bupivacaine for spinal anesthesia. Anesth Analg. 2002 Jan;94(1):194-8. [PubMed]
- Bay-Nielsen M, Klarskov B, Bech K, Anderson J, Kehlet H. Levobupivacaine vs bupivacaine as infiltration anaesthesia in inguinal herniorrhaphy. Br J Anaesth. 1999 Feb;82(2):280–2. [PubMed] [Free full text]
- Gautier P, De Kock M, Huberty L, Demir T, Izydorczic M, Vanderick B. Comparison of the effects of intrathecal ropivacaine, levobupivacaine,and bupivacaine for Caesarean section. Br J Anaesth. 2003 Nov;91(5):684-9. [PubMed] [Free full text]
- Guler G, Cakir G, Ulgey A, Ugur F, Bicer C, Gunes I, et al. A Comparison of spinal anesthesia with levobupivacaine and hyperbaric bupivacaine for cesarean sections: A randomized trial. Open.J Anesthesiol 2012;2:84-9.
- Turkmen A, Moralar DG, Ali A, Altan A. Comparison of the anesthetic effects of intrathecal levobupivacaine+fentanyl and bupivacaine+fentanyl during caesarean section. Middle East J Anesthesiol. 2012 Feb;21(4):577- [PubMed]
- Coppejans HC, Vercauteren MP, Spinal Levobupivacaine for cesarean section causes less hypotension and motor block than racemic bupivacaine. Int J Obstet Anaesth. 2004; 13: S16.
- Buyse I, Stockman W, Columb M, Vandermeersch E, Van de Velde M. Effect of sufentanil on minimum local analgesic concentrations of epidural bupivacaine, ropivacaine and levobupivacaine in nullipara in early labour. Int J Obstet Anesth. 2007 Jan;16(1):22- [PubMed]
- Carpenter RL, Caplan RA, Brown DL, Stephenson C, Wu R. Incidence and risk factors for side effects of spinal anesthesia. Anesthesiology. 1992 Jun;76(6):906–16. [PubMed] [Free full Text]