Kavita Jain, MD1, Surendra K. Sethi, MD2*, Neena Jain, MD1, Sunil Saini, MD3, Arvind Khare, MD4
1Professor; 2Assistant Professor; 3Ex PG Student, 4Associate Professor
Department of Anesthesiology, Jawaharlal Nehru Medical College, Muslim Mochi Mohalla, JLN Medical College Circle, Ajmer, Rajasthan 305001, (India)
Correspondence: Dr. Surendra Kumar Sethi, MD, Assistant Professor, Department of Anesthesiology, JLN Medical College, Muslim Mochi Mohalla, JLN Medical College Circle, Ajmer, Rajasthan 305001, (India); Phone: +919587150598; E-mail: drsurendrasethi80@gmail.com
ABSTRACT
Background: Rocuronium, a non-depolarizing neuromuscular blocking agent, has been used for rapid sequence induction and intubation, as it has rapid onset and acceptable intubating conditions at higher doses. Propofol, when used as an induction agent reduces cardiac output, thereby may decrease delivery of neuromuscular blocking agent at neuromuscular junction and thereby time of onset of action of rocuronium can be increased. Ephedrine has been described to speed up the onset of action of rocuronium and provide better intubating conditions during induction of anesthesia. We conducted this study to quantify the effect of ephedrine on intubation conditions and hemodynamic profile during induction of general anesthesia with propofol and rocuronium.
Methodology: Sixty adult patients of ASA Grade 1 and 2, aged between 18-55 years scheduled for various elective surgeries under general anesthesia, were randomly allocated into two groups with 30 patients in each group; Group A (n = 30) received inj ephedrine 70 µg/kg followed one minute later by propofol 2.5 mg/kg with rocuronium 0.6 mg/kg and Group B (n = 30) received normal saline followed one minute later by propofol 2.5 mg/kg and rocuronium 0.6 mg/kg. Intubating conditions and hemodynamic parameters were assessed in both groups.
Results: The demographic data and baseline hemodynamic parameters were comparable between the two groups, (P > 0.05). However, there was a significant difference in hemodynamic parameters after induction in both groups, (P < 0.05) but clinically the difference was insignificant. The intubating conditions were significantly better in Group A as compared to Group B, (P < 0.05).
Conclusion: The use of low dose ephedrine before induction with propofol and rocuronium (0.6 mg/kg) provided better intubating conditions as compared to induction with propofol and rocuronium alone at 60 seconds. The variations in hemodynamic parameters were found to be statistically significant but clinically insignificant from their baseline values.
Key words: Ephedrine; Propofol; Rocuronium; Intubation, Endotracheal; Endotracheal Anesthesia; Hemodynamics; Vasoconstriction; Vasodilatation
Citation: Jain K, Sethi SK, Jain N, Saini S, Khare A. Comparison of intubating conditions and hemodynamics during rapid sequence induction and intubation using propofol and rocuronium with low dose ephedrine and without ephedrine. Anaesth Pain & Intensive Care 2016;20(3):320-327
Received: 25 June 2016; Reviewed: 6 & 9 September 2016; Corrected: 12 September 2016; Accepted: 15 September 2016
INTRODUCTION
Succinylcholine, a depolarizing muscle relaxant, has been traditionally used as a drug of choice for endotracheal intubation during rapid sequence induction of anesthesia. However, it is associated with various adverse effects that warrants the search for an alternative neuromuscular blocking agent for rapid sequence induction and intubation.1,2 Rocuronium, a nondepolarizing neuromuscular blocking agent, is currently preferred as an alternative to succinylcholine as it has rapid onset and may provide intubating conditions in 60-90 sec depending on the dose administered, and is devoid of side effects including hyperkalemia and inducing malignant hyperpyrexia. The larger doses of rocuronium (0.9-1.2 mg/kg) may be associated with prolonged duration of action but provides equivalent intubating conditions as succinylcholine.1-3 So various methods or techniques were used to reduce the effective dose of rocuronium simultaneously not compromising its rapid onset and intubating conditions. The onset of action of rocuronium along with intubating conditions may be enhanced by using certain vasopressor or inotropic drugs like ephedrine, a sympathomimetic agent, which acts by increasing cardiac output and tissue perfusion during induction of anesthesia.1-9 So an optimal dose of ephedrine should be chosen to achieve rapid onset and better intubating conditions with minimal adverse hemodynamic effects like hypertension or tachycardia simultaneously reducing the duration of action of rocuronium using low dose (0.6 mg/kg) which is desirable in some surgeries with short duration.1-9 The previous studies have shown the reduction in onset time of rocuronium along with better intubating conditions when ephedrine was used at a low dose (70 µg/kg). However, they studied the comparative effects of different doses of ephedrine. So we hypothesized that low dose of ephedrine may reduce the risk of increased heart rate (HR) and mean arterial pressure (MAP) which can prove to be beneficial for the patients with limited cardiac reserve. The higher doses of ephedrine might be associated with adverse hemodynamic events, as reported by some studies.1,2,10-13 So the present study was undertaken for comparison of intubating conditions and hemodynamic changes with and without pretreatment with low dose ephedrine using propofol and rocuronium (0.6 mg/kg) in patients undergoing general anesthesia.
METHODOLOGY
After obtaining approval from local ethical committee, this prospective randomized double blind study was undertaken in the Department of Anesthesiology, JLN Medical College & Hospital, Ajmer and included 60 adult patients of either sex between ages 18-55 years planned for various elective surgeries under general anesthesia requiring endotracheal intubation. Patients of ASA Grade I and II, Mallampati grade I and II and with thyromental distance > 6 cm were included in the study.
Each patient was seen for detailed pre anesthetic evaluation a day before surgery, and necessary investigations (hemoglobin, fasting blood sugar, serum urea, serum creatinine, platelet count, chest x-ray, electrocardiogram) were checked. Demographic data were recorded and written informed consent was taken. Patients were advised overnight fasting.
Patients with cardiac problems, such as hypertension, coronary artery disease, heart failure and heart blocks, metabolic, neuromuscular and blood coagulation disorders, bronchial asthma, chronic obstructive pulmonary disease, diabetes mellitus, thyroid disorders and pregnancy were excluded. Patients on concurrent drug therapy with sympathetic active drugs, digitalis etc, or with history of allergic reaction to any of the drugs used in this study were also excluded.
All patients were randomly divided into two groups of 30 patients each using computer generated random number table and allocation concealment was done with closed sealed envelope technique.
After shifting patient to operating room intravenous access was secured. Preoperative baseline values of HR, blood pressure (NIBP) and oxygen saturation (SpO2) were recorded and crystalloid infusion was started. All the patients received inj. glycopyrrolate 0.005 mg/kg as premedication and inj. fentanyl 2 µg/kg. Group A (n = 30) patients were given inj ephedrine 70 µg/kg, and Group B (n = 30) patients received equal volume of normal saline. Anesthesia was induced with inj. propofol 2.5 mg/kg and inj. rocuronium 0.6 mg/kg. The study drug was prepared by a resident in anesthesiology who was not involved in the study.
After spontaneous breathing ceased intermittent positive pressure ventilation was started. Intubating conditions were assessed by jaw relaxation, vocal cord position, diaphragmatic response. The onset of rocuronium was defined as the time in seconds from the end of injection of rocuronium to complete jaw relaxation, absent vocal cord movement and absent diaphragmatic response.
Endotracheal intubation was done in all patients, using appropriate sized polyvinyl chloride oral cuffed tubes by a trained anesthesiologist who had 3 years of experience, was unaware with the study drug or group and also assessed the intubating conditions. HR, BP and oxygen saturation were monitored continuously and recorded at baseline, 1 min after ephedrine dosing, 1 min after induction, immediately after intubation and at 1, 3, 5, 10, 15 and 30 min after intubation. Complications if any were noted.
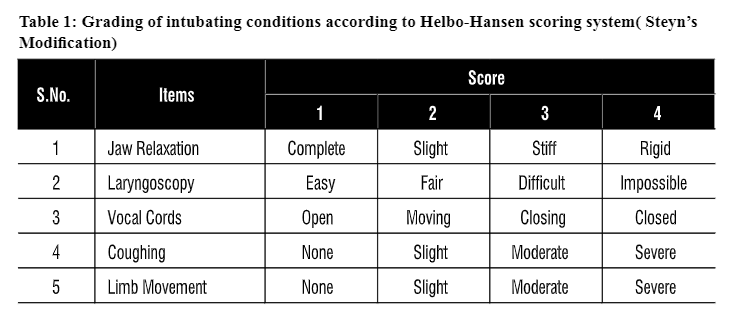
Tracheal intubating conditions were graded based on scoring system devised by Helbo-Hansen et al with Steyn’s modification,7 which includes five criteria graded on a four point scale (Table 1). Intubating conditions were considered acceptable when every item had a score less than or equal to two. The intubation was performed only when acceptable conditions were present otherwise intubation was denied and these patients were graded under poor or unacceptable intubating conditions.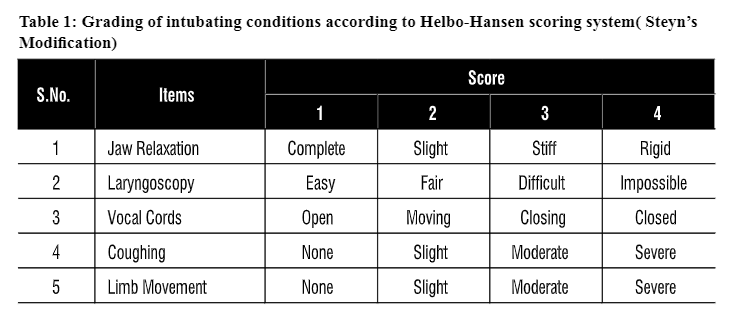 .
.
After intubation anesthesia was maintained with oxygen and nitrous oxide 40:60 in 0.6-0.8% halothane. Rocuronium 0.1 mg/kg was given at intervals of 20 min. Onset time of rocuronium, intubation time (time taken from insertion of laryngoscope into oral cavity till removal of laryngoscope), number of attempts for intubation, duration of surgery (time from surgical incision of skin till last skin suture), recovery time (time from end of anesthesia till eye opening) and extubation time (time from end of anesthesia till removal of tube) were recorded. After completion of surgery and resumption of spontaneous breathing effort, patients were reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. Extubation was done after adequate recovery of muscle power, reflexes and respiration.
Statistical Analysis: The sample size was calculated with an 80% power to detect the significant difference in intubating conditions between ephedrine and control groups and also based on previous studies. Statistical analysis of our study was performed using SPSS 20.0 (SPSS Inc, Chicago, IL, USA). The demographic data, intubating conditions and clinical significance of hemodynamic changes were analyzed using student’s t-test and chi square test or Fischer’s exact test, whichever appropriate. The comparison between two groups regarding hemodynamic parameters was done using student’s t-test and intragroup comparison was done with analysis of variance (ANOVA) while considering the baseline values as control. A P < 0.05 was considered to be statistically significant. The data were reported as mean ± SD and frequency.
RESULTS
The patients in both groups were comparable with respect to demographic profile e.g., age, sex and weight (P > 0.05) (Table 2).
Table 2: Comparison of demographic data between two groups
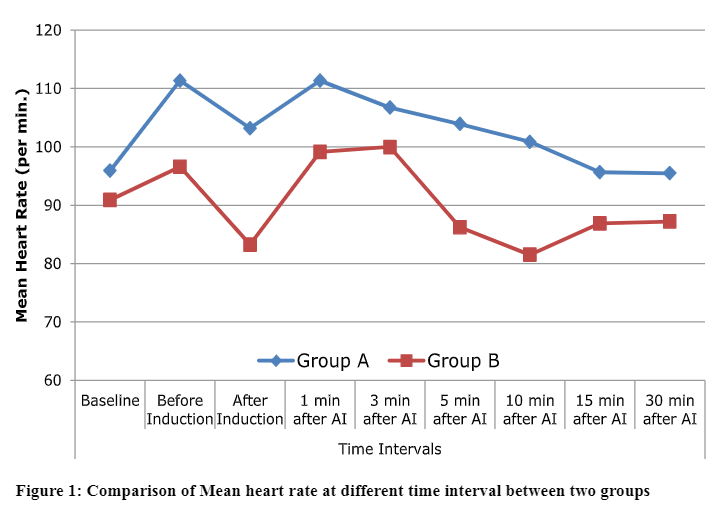
The baseline HR was comparable between the two groups (P = 0.3). However, there was significant increase in HR before induction i.e. one minute after administration of ephedrine in Group A as compared to Group B (111 ± 17 per min vs. 96 ± 22 per min) (P = 0.007). The mean HR was significantly different between the two groups after induction with propofol (P = 0.0001).
 .
.
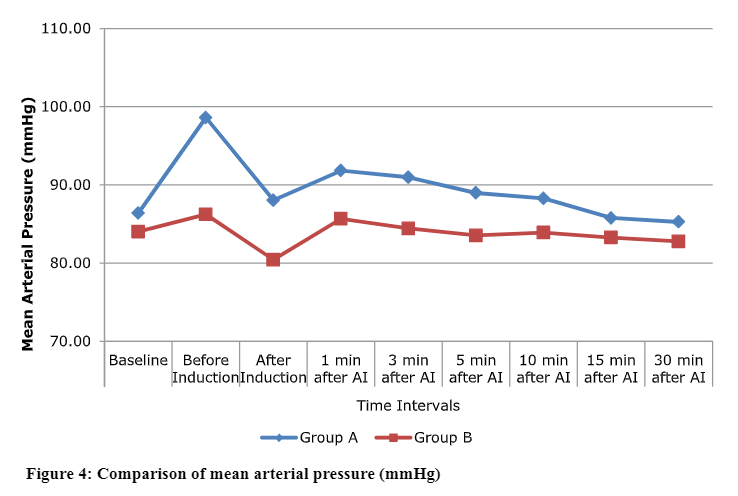
The reduction in HR was statistically more significant in Group B as compared to Group A (83 ± 16 vs. 103 ± 15 per min), but it remained above the baseline values in Group A after induction with propofol. The mean HR remained above the baseline values in Group A at 1, 3, 5 and 10 min after induction. A significant rise in HR was observed in both groups after intubation, (111 ± 14 vs. 99 ± 21 per min) in Group A and B respectively (p = 0.01). The mean HR returned to baseline values after 15 min in Group A whereas after 3 min in Group B which was statistically significant but clinically not significant (considering limits of 20% change from their baseline values) (Figure 1).
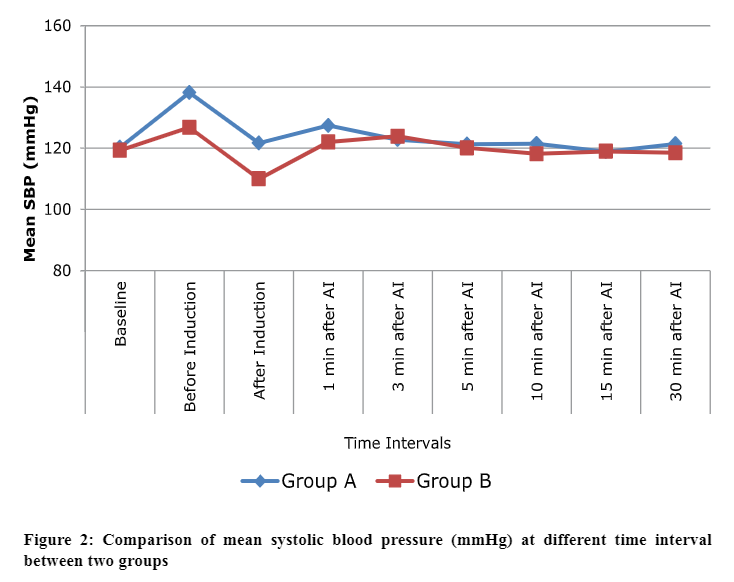
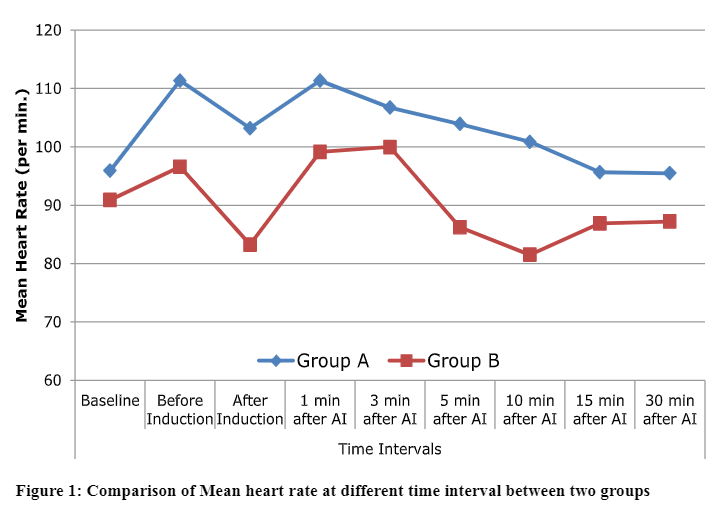
The baseline mean SBP was 120.3 ± 8.5 vs 119.3 ± 13.3 mmHg in Group A and Group B respectively, the difference was statistically insignificant between the two groups (P = 0.73) A significant rise in mean SBP was observed in both groups from their baseline values but more significant in Group A as compared to Group B (138.1 ± 9.2 vs. 126.7 ± 13.7 mmHg) (P = 0.0003). However, there was significant reduction in mean SBP in both groups from their pre-induction values after induction but comparable to the baseline values in Group A; whereas, there was significant reduction in SBP in Group B both from their baseline and pre-induction values. The mean SBP remained near to baseline values after 1 min in both groups except slight increase in SBP in Group A after intubation which was not statistically significant (P > 0.05) (Figure 2).
Table 3: Comparison of intubating conditions between two groups (Helbo-Hansen scoring system with Steyn’s modification)
P < 0.05 statistically significant
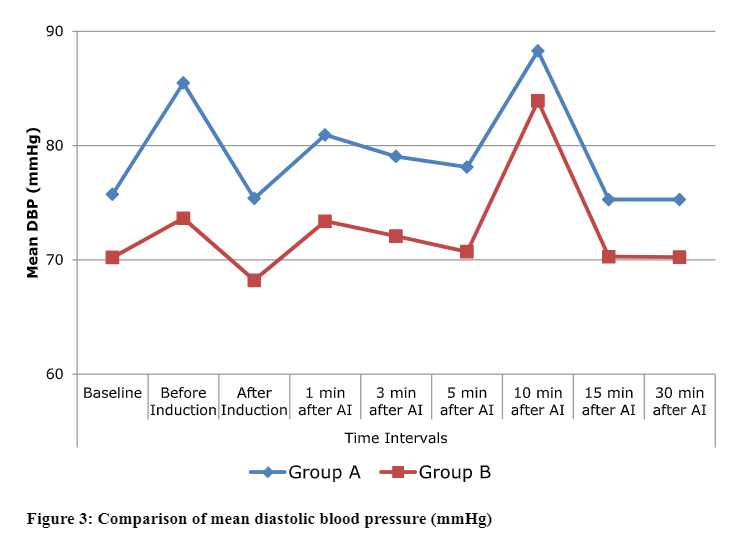
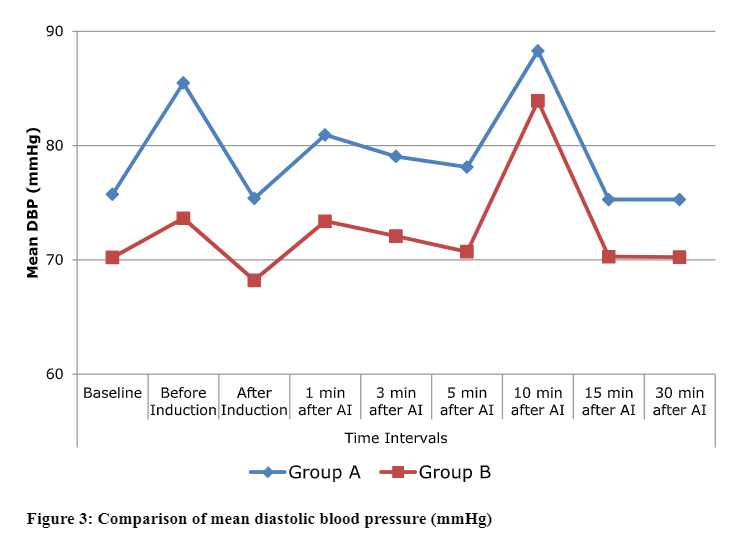
The baseline mean DBP was also comparable between the two groups, 86.4 ± 7.7 vs 84.0 ± 14.9 mmHg, in Group A and B respectively (P = 0.053). The mean DBP was statistically different between two groups before induction, after induction and up to 30 min (P < 0.05) but clinically not significant (Figure 3).
 .
.
 .
.
 .
.
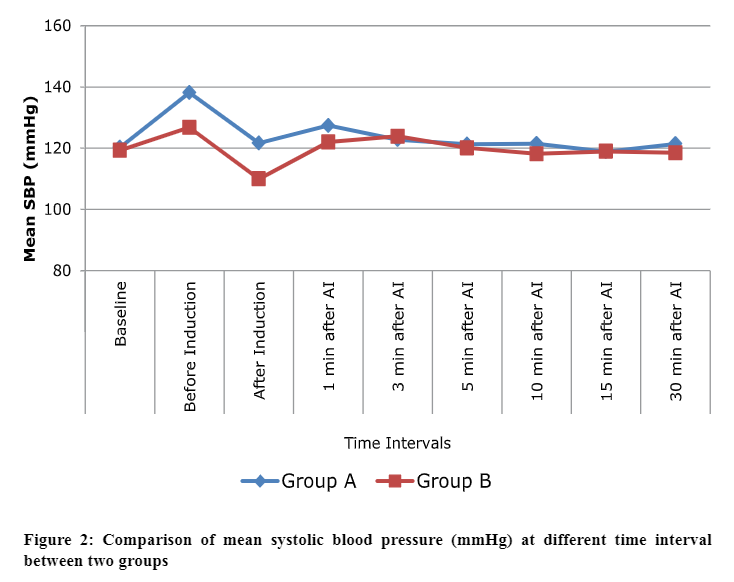
The baseline MAP was statistically insignificant between the two groups (P = 0.441), but the rise in MAP was observed in both groups before induction which was statistically significant between the two groups, 98.6 ± 8.05 vs 86.2 ± 14.4 mmHg, in Group A and B respectively, (P < 0.001). The increase in MAP was significantly more in Group A from their baseline values as compared to Group B. However, MAP returned to their baseline values in Group A and Group B after induction but significantly less from their preinduction values and remained stable throughout the study period i.e. up to 30 minutes but statistically significant difference was observed between two groups up to 5 min after induction (P < 0.05) (Figure 4). The mean SpO2 remained comparable and stable throughout the study period in both groups (P > 0.05).
The distribution of intubating conditions showed statistically significant difference between the two groups (P < 0.05). In Group A and B, none of the patients had ‘excellent’ intubating conditions but 25 patients had ‘good’ intubating conditions in Group A as compared to 12 patients in Group B. Six patients in Group A showed ‘poor’ intubating conditions as compared to 18 patients in Group B. None of the patients in both groups showed ‘bad’ intubating conditions assessed on the basis of scoring by various parameters. So 25 (84%) patients had acceptable intubating conditions in Group A as compared to 12 (40%) of patients in Group B which was statistically significant between the two groups (P < 0.05) (Table 3).
DISCUSSION
Various techniques have been described to improve the intubating conditions and time of onset of rocuronium during rapid sequence induction and intubation during general anesthesia. The onset time of a neuromuscular blocking agent depends on the cardiac output and muscle blood flow.1-3 Rocuronium, when used in a lower dose (0.6 mg/kg) for rapid sequence induction and intubation might not provide optimal intubating conditions due to slower onset of action caused by reduction in cardiac output and tissue perfusion with induction agents like propofol at laryngeal and diaphragmatic muscles.1 However, ephedrine at a low dose (70 µg/kg), because of its sympathomimetic action at alpha and beta adrenergic receptors, might shorten the time of onset with acceptable intubating conditions of rocuronium simultaneously providing better hemodynamic profile avoiding any adverse events.2,11
Our rationale to conduct this study was to find out whether 70 µg/kg of ephedrine can shorten the onset time of rocuronium (particularly at low dose) with acceptable intubating conditions with maintenance of hemodynamic status and to know whether it is effective in improving the intubating conditions using propofol as induction agent and rocuronium (0.6 mg/kg) as neuromuscular blocking agent. This low dose might reduce the beta adrenergic adverse effects associated with higher doses of ephedrine like hypertension and tachycardia. In our study, ephedrine improved the intubating conditions without significant effects on hemodynamic parameters. However, previous studies compared the different doses of ephedrine with different induction agents and they didn’t find ephedrine effective at higher doses (>100 µg/kg) and found it detrimental for patients with low cardiac reserve as far as hemodynamic parameters are concerned.1-4,12,18 So with above hypothesis we only studied to find out the optimal low dose of ephedrine along with low dose of rocuronium which might be desirable in some situations.
In our study, we compared the intubating conditions between the ephedrine and control groups. Intubating condition is the principal qualitative measure for rapid sequence induction and intubation as it indicates whether the patient’s airway can be safely secured or not. The intubating conditions were significantly better in ephedrine group (Group A) as compared to saline group (Group B) (P < 0.05). The ephedrine group had acceptable intubating conditions in 84% of patients as compared to 40% of patients in saline group which concurs with the study done by Tan CH et al6 who found that intubating conditions were excellent (acceptable) in 84% of patients in propofol-ephedrine group as compared to 32% in propofol alone group. The improved intubating conditions were achieved at lower doses of rocuronium (0.6 mg/kg) at 60 seconds which is generally achieved using higher doses of rocuronium (0.9 mg/kg) in 60-90 seconds showed that ephedrine pretreatment reduced the onset time even at lower doses of rocuronium with acceptable intubating conditions. Our findings were also similar to the studies done by earlier researchers,1,2,12,14 who observed that intubating conditions were better in patients pretreated with ephedrine before induction and rapid tracheal intubation as they had used the similar doses of ephedrine and rocuronium and achieved acceptable intubating conditions in 60 seconds.9,15-17 However some authors had used different doses of ephedrine (70 – 210 µg/kg) in their studies and they found more better intubating conditions at higher doses of ephedrine even in 30 seconds but at the cost of significant hemodynamic variations which might be detrimental for patients with low cardiac reserve.4,18
In our study, the baseline HR were comparable between the two groups. The significant difference in mean HR was observed before induction (1 min after ephedrine pretreatment), after induction and after intubation (P < 0.05), but clinically it was not significant (within 20% change from their baseline values). In Group A, the increase in HR before induction was associated with ephedrine action, however, in Group B glycopyrrolate used as premedication may increase the HR but it was more significant in ephedrine group due to synergistic effect of ephedrine and glycopyrrolate.1,8,9 A significant reduction in HR was observed after induction in both groups (P<0.05), but more in saline group which can be due to induction with propofol alone. The HR again increased after intubation in both groups and persisted at higher values from their baseline values up to 10 min after induction in ephedrine group and up to 3 min in saline group. Again the action of ephedrine and intubation response might cause increase in HR significantly in ephedrine group but clinically not significant. Our findings were similar to the study done by Gopalkrishna et al1 who compared the effect of ephedrine on hemodynamic conditions in rapid induction of anesthesia with propofol and rocuronium and found favorable hemodynamic conditions during intubation and no significant difference among the ephedrine group; however, results were different and significant at higher doses of ephedrine. Our results also concurred with the findings of Karampal singh et al12 and Madhusudan et al.2,9,19
A significant rise in SBP before induction could be explained by pretreatment with ephedrine which increases cardiac output and after intubation, and due to stress response induced by laryngoscopy and intubation. However, after induction both groups showed significant decrease in SBP (P < 0.05) but more in saline group. This may be due to counter effect of ephedrine on propofol which leads to less reduction in SBP in ephedrine group as compared to saline group. The laryngoscopy and intubation induced increase in SBP was at its peak after 1 min in ephedrine group and remained stable thereafter and statistically insignificant between two groups throughout the study period.1,2 Our results were supported by the study done by Michelson et al7 who concluded that prophylactic injection of ephedrine significantly attenuated but did not completely abolish the decrease in blood pressure associated with induction of anesthesia with propofol and fentanyl. Similarly Gopalkrishna et al1 also found that pretreatment with ephedrine is effective in preventing hypotension after induction of anesthesia .However Masjedi et al20 reported that high dose of ephedrine (0.15 mg/kg) may have significant effect in preventing hypotension and bradycardia after induction with propofol and remifentanil which may be due to higher dose of ephedrine used in their study.
The MAP showed significant increase before induction (after ephedrine pretreatment) in ephedrine group from their baseline values (P < 0.05), which was statistically significant but clinically in acceptable range. The MAP remained near to baseline values after intubation in both groups and but statistically significant between two groups up to 5 min after intubation. The increase in MAP was on account of pretreatment with ephedrine as it was more pronounced in ephedrine group as compared to saline group but clinically insignificant (considering limits of 20% change from their baseline values). The MAP showed similar trends as SBP and found to be similar to the study done by Michelson et al, Gopalkrishna et al and Madhusudan et al found similar results in their study as they have used similar dose of ephedrine as we have used. The mean SpO2 remained comparable between two groups at all time intervals (P > 0.05).1,2,7-9
Limitations: Neuromuscular monitoring and cardiac output monitoring would make strong evidence to support our results while assessing intubating conditions, but we didn’t had these facilities at our institute.
CONCLUSION
The low dose ephedrine (70 µg/kg) and propofol combination before induction provides significantly better intubating conditions as compared to propofol alone, used with rocuronium. This combination allows rapid onset with acceptable intubating conditions even in one minute at low dose of rocuronium as higher doses (0.9-1.2 mg/kg) may be associated with prolonged duration of action which may be undesirable in various surgeries. The hemodynamic parameters were statistically different between two groups but clinically they were in acceptable range considering the limits of 20% change from their baseline values. No significant hypertension or tachycardia were observed but ephedrine prevents hypotension and bradycardia associated with propofol induction. However, precautions should always be taken in patients with limited cardiac reserve.
Declarations: No funding from any external source was used for the conduct of this study.
Ethical approval: Obtained from local institutional ethical committee.
Authors’ contribution: KJ: Concepts, literature review, manuscript editing and review
SKS: Literature search and review, manuscript preparation and editing
NJ: Concepts and design, manuscript review
SS: Literature search, conduction of study work
AK: Concepts, manuscript review
REFERENCES
1Professor; 2Assistant Professor; 3Ex PG Student, 4Associate Professor
Department of Anesthesiology, Jawaharlal Nehru Medical College, Muslim Mochi Mohalla, JLN Medical College Circle, Ajmer, Rajasthan 305001, (India)
Correspondence: Dr. Surendra Kumar Sethi, MD, Assistant Professor, Department of Anesthesiology, JLN Medical College, Muslim Mochi Mohalla, JLN Medical College Circle, Ajmer, Rajasthan 305001, (India); Phone: +919587150598; E-mail: drsurendrasethi80@gmail.com
ABSTRACT
Background: Rocuronium, a non-depolarizing neuromuscular blocking agent, has been used for rapid sequence induction and intubation, as it has rapid onset and acceptable intubating conditions at higher doses. Propofol, when used as an induction agent reduces cardiac output, thereby may decrease delivery of neuromuscular blocking agent at neuromuscular junction and thereby time of onset of action of rocuronium can be increased. Ephedrine has been described to speed up the onset of action of rocuronium and provide better intubating conditions during induction of anesthesia. We conducted this study to quantify the effect of ephedrine on intubation conditions and hemodynamic profile during induction of general anesthesia with propofol and rocuronium.
Methodology: Sixty adult patients of ASA Grade 1 and 2, aged between 18-55 years scheduled for various elective surgeries under general anesthesia, were randomly allocated into two groups with 30 patients in each group; Group A (n = 30) received inj ephedrine 70 µg/kg followed one minute later by propofol 2.5 mg/kg with rocuronium 0.6 mg/kg and Group B (n = 30) received normal saline followed one minute later by propofol 2.5 mg/kg and rocuronium 0.6 mg/kg. Intubating conditions and hemodynamic parameters were assessed in both groups.
Results: The demographic data and baseline hemodynamic parameters were comparable between the two groups, (P > 0.05). However, there was a significant difference in hemodynamic parameters after induction in both groups, (P < 0.05) but clinically the difference was insignificant. The intubating conditions were significantly better in Group A as compared to Group B, (P < 0.05).
Conclusion: The use of low dose ephedrine before induction with propofol and rocuronium (0.6 mg/kg) provided better intubating conditions as compared to induction with propofol and rocuronium alone at 60 seconds. The variations in hemodynamic parameters were found to be statistically significant but clinically insignificant from their baseline values.
Key words: Ephedrine; Propofol; Rocuronium; Intubation, Endotracheal; Endotracheal Anesthesia; Hemodynamics; Vasoconstriction; Vasodilatation
Citation: Jain K, Sethi SK, Jain N, Saini S, Khare A. Comparison of intubating conditions and hemodynamics during rapid sequence induction and intubation using propofol and rocuronium with low dose ephedrine and without ephedrine. Anaesth Pain & Intensive Care 2016;20(3):320-327
Received: 25 June 2016; Reviewed: 6 & 9 September 2016; Corrected: 12 September 2016; Accepted: 15 September 2016
INTRODUCTION
Succinylcholine, a depolarizing muscle relaxant, has been traditionally used as a drug of choice for endotracheal intubation during rapid sequence induction of anesthesia. However, it is associated with various adverse effects that warrants the search for an alternative neuromuscular blocking agent for rapid sequence induction and intubation.1,2 Rocuronium, a nondepolarizing neuromuscular blocking agent, is currently preferred as an alternative to succinylcholine as it has rapid onset and may provide intubating conditions in 60-90 sec depending on the dose administered, and is devoid of side effects including hyperkalemia and inducing malignant hyperpyrexia. The larger doses of rocuronium (0.9-1.2 mg/kg) may be associated with prolonged duration of action but provides equivalent intubating conditions as succinylcholine.1-3 So various methods or techniques were used to reduce the effective dose of rocuronium simultaneously not compromising its rapid onset and intubating conditions. The onset of action of rocuronium along with intubating conditions may be enhanced by using certain vasopressor or inotropic drugs like ephedrine, a sympathomimetic agent, which acts by increasing cardiac output and tissue perfusion during induction of anesthesia.1-9 So an optimal dose of ephedrine should be chosen to achieve rapid onset and better intubating conditions with minimal adverse hemodynamic effects like hypertension or tachycardia simultaneously reducing the duration of action of rocuronium using low dose (0.6 mg/kg) which is desirable in some surgeries with short duration.1-9 The previous studies have shown the reduction in onset time of rocuronium along with better intubating conditions when ephedrine was used at a low dose (70 µg/kg). However, they studied the comparative effects of different doses of ephedrine. So we hypothesized that low dose of ephedrine may reduce the risk of increased heart rate (HR) and mean arterial pressure (MAP) which can prove to be beneficial for the patients with limited cardiac reserve. The higher doses of ephedrine might be associated with adverse hemodynamic events, as reported by some studies.1,2,10-13 So the present study was undertaken for comparison of intubating conditions and hemodynamic changes with and without pretreatment with low dose ephedrine using propofol and rocuronium (0.6 mg/kg) in patients undergoing general anesthesia.
METHODOLOGY
After obtaining approval from local ethical committee, this prospective randomized double blind study was undertaken in the Department of Anesthesiology, JLN Medical College & Hospital, Ajmer and included 60 adult patients of either sex between ages 18-55 years planned for various elective surgeries under general anesthesia requiring endotracheal intubation. Patients of ASA Grade I and II, Mallampati grade I and II and with thyromental distance > 6 cm were included in the study.
Each patient was seen for detailed pre anesthetic evaluation a day before surgery, and necessary investigations (hemoglobin, fasting blood sugar, serum urea, serum creatinine, platelet count, chest x-ray, electrocardiogram) were checked. Demographic data were recorded and written informed consent was taken. Patients were advised overnight fasting.
Patients with cardiac problems, such as hypertension, coronary artery disease, heart failure and heart blocks, metabolic, neuromuscular and blood coagulation disorders, bronchial asthma, chronic obstructive pulmonary disease, diabetes mellitus, thyroid disorders and pregnancy were excluded. Patients on concurrent drug therapy with sympathetic active drugs, digitalis etc, or with history of allergic reaction to any of the drugs used in this study were also excluded.
All patients were randomly divided into two groups of 30 patients each using computer generated random number table and allocation concealment was done with closed sealed envelope technique.
After shifting patient to operating room intravenous access was secured. Preoperative baseline values of HR, blood pressure (NIBP) and oxygen saturation (SpO2) were recorded and crystalloid infusion was started. All the patients received inj. glycopyrrolate 0.005 mg/kg as premedication and inj. fentanyl 2 µg/kg. Group A (n = 30) patients were given inj ephedrine 70 µg/kg, and Group B (n = 30) patients received equal volume of normal saline. Anesthesia was induced with inj. propofol 2.5 mg/kg and inj. rocuronium 0.6 mg/kg. The study drug was prepared by a resident in anesthesiology who was not involved in the study.
After spontaneous breathing ceased intermittent positive pressure ventilation was started. Intubating conditions were assessed by jaw relaxation, vocal cord position, diaphragmatic response. The onset of rocuronium was defined as the time in seconds from the end of injection of rocuronium to complete jaw relaxation, absent vocal cord movement and absent diaphragmatic response.
Endotracheal intubation was done in all patients, using appropriate sized polyvinyl chloride oral cuffed tubes by a trained anesthesiologist who had 3 years of experience, was unaware with the study drug or group and also assessed the intubating conditions. HR, BP and oxygen saturation were monitored continuously and recorded at baseline, 1 min after ephedrine dosing, 1 min after induction, immediately after intubation and at 1, 3, 5, 10, 15 and 30 min after intubation. Complications if any were noted.
Tracheal intubating conditions were graded based on scoring system devised by Helbo-Hansen et al with Steyn’s modification,7 which includes five criteria graded on a four point scale (Table 1). Intubating conditions were considered acceptable when every item had a score less than or equal to two. The intubation was performed only when acceptable conditions were present otherwise intubation was denied and these patients were graded under poor or unacceptable intubating conditions.
 .
.After intubation anesthesia was maintained with oxygen and nitrous oxide 40:60 in 0.6-0.8% halothane. Rocuronium 0.1 mg/kg was given at intervals of 20 min. Onset time of rocuronium, intubation time (time taken from insertion of laryngoscope into oral cavity till removal of laryngoscope), number of attempts for intubation, duration of surgery (time from surgical incision of skin till last skin suture), recovery time (time from end of anesthesia till eye opening) and extubation time (time from end of anesthesia till removal of tube) were recorded. After completion of surgery and resumption of spontaneous breathing effort, patients were reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. Extubation was done after adequate recovery of muscle power, reflexes and respiration.
Statistical Analysis: The sample size was calculated with an 80% power to detect the significant difference in intubating conditions between ephedrine and control groups and also based on previous studies. Statistical analysis of our study was performed using SPSS 20.0 (SPSS Inc, Chicago, IL, USA). The demographic data, intubating conditions and clinical significance of hemodynamic changes were analyzed using student’s t-test and chi square test or Fischer’s exact test, whichever appropriate. The comparison between two groups regarding hemodynamic parameters was done using student’s t-test and intragroup comparison was done with analysis of variance (ANOVA) while considering the baseline values as control. A P < 0.05 was considered to be statistically significant. The data were reported as mean ± SD and frequency.
RESULTS
The patients in both groups were comparable with respect to demographic profile e.g., age, sex and weight (P > 0.05) (Table 2).
Table 2: Comparison of demographic data between two groups
| Parameter | Group A
(n = 30) |
Group B
(n = 30) |
P value |
| Age ( years) Mean+SD | 38.8+13.34 | 38.23+17.12 | >0.05 |
| Weight (kg) Mean+SD | 52.3+9.20 | 54.07+15.07 | |
| Sex (M/F) (n) | 12/18 | 13/17 |
 .
.The reduction in HR was statistically more significant in Group B as compared to Group A (83 ± 16 vs. 103 ± 15 per min), but it remained above the baseline values in Group A after induction with propofol. The mean HR remained above the baseline values in Group A at 1, 3, 5 and 10 min after induction. A significant rise in HR was observed in both groups after intubation, (111 ± 14 vs. 99 ± 21 per min) in Group A and B respectively (p = 0.01). The mean HR returned to baseline values after 15 min in Group A whereas after 3 min in Group B which was statistically significant but clinically not significant (considering limits of 20% change from their baseline values) (Figure 1).
The baseline mean SBP was 120.3 ± 8.5 vs 119.3 ± 13.3 mmHg in Group A and Group B respectively, the difference was statistically insignificant between the two groups (P = 0.73) A significant rise in mean SBP was observed in both groups from their baseline values but more significant in Group A as compared to Group B (138.1 ± 9.2 vs. 126.7 ± 13.7 mmHg) (P = 0.0003). However, there was significant reduction in mean SBP in both groups from their pre-induction values after induction but comparable to the baseline values in Group A; whereas, there was significant reduction in SBP in Group B both from their baseline and pre-induction values. The mean SBP remained near to baseline values after 1 min in both groups except slight increase in SBP in Group A after intubation which was not statistically significant (P > 0.05) (Figure 2).
Table 3: Comparison of intubating conditions between two groups (Helbo-Hansen scoring system with Steyn’s modification)
| Group | Intubating Conditions | P value | |
| Acceptable
Good (6-10) |
Not acceptable
Poor (11-15) |
||
| A | 25 (84%) | 5 (16%) | <0.05 |
| B | 12 (40%) | 18 (60%) | |
The baseline mean DBP was also comparable between the two groups, 86.4 ± 7.7 vs 84.0 ± 14.9 mmHg, in Group A and B respectively (P = 0.053). The mean DBP was statistically different between two groups before induction, after induction and up to 30 min (P < 0.05) but clinically not significant (Figure 3).
 .
. .
.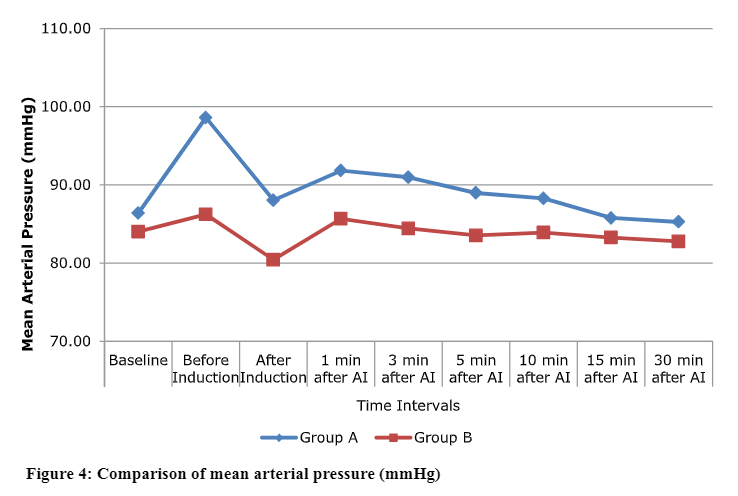 .
.The baseline MAP was statistically insignificant between the two groups (P = 0.441), but the rise in MAP was observed in both groups before induction which was statistically significant between the two groups, 98.6 ± 8.05 vs 86.2 ± 14.4 mmHg, in Group A and B respectively, (P < 0.001). The increase in MAP was significantly more in Group A from their baseline values as compared to Group B. However, MAP returned to their baseline values in Group A and Group B after induction but significantly less from their preinduction values and remained stable throughout the study period i.e. up to 30 minutes but statistically significant difference was observed between two groups up to 5 min after induction (P < 0.05) (Figure 4). The mean SpO2 remained comparable and stable throughout the study period in both groups (P > 0.05).
The distribution of intubating conditions showed statistically significant difference between the two groups (P < 0.05). In Group A and B, none of the patients had ‘excellent’ intubating conditions but 25 patients had ‘good’ intubating conditions in Group A as compared to 12 patients in Group B. Six patients in Group A showed ‘poor’ intubating conditions as compared to 18 patients in Group B. None of the patients in both groups showed ‘bad’ intubating conditions assessed on the basis of scoring by various parameters. So 25 (84%) patients had acceptable intubating conditions in Group A as compared to 12 (40%) of patients in Group B which was statistically significant between the two groups (P < 0.05) (Table 3).
DISCUSSION
Various techniques have been described to improve the intubating conditions and time of onset of rocuronium during rapid sequence induction and intubation during general anesthesia. The onset time of a neuromuscular blocking agent depends on the cardiac output and muscle blood flow.1-3 Rocuronium, when used in a lower dose (0.6 mg/kg) for rapid sequence induction and intubation might not provide optimal intubating conditions due to slower onset of action caused by reduction in cardiac output and tissue perfusion with induction agents like propofol at laryngeal and diaphragmatic muscles.1 However, ephedrine at a low dose (70 µg/kg), because of its sympathomimetic action at alpha and beta adrenergic receptors, might shorten the time of onset with acceptable intubating conditions of rocuronium simultaneously providing better hemodynamic profile avoiding any adverse events.2,11
Our rationale to conduct this study was to find out whether 70 µg/kg of ephedrine can shorten the onset time of rocuronium (particularly at low dose) with acceptable intubating conditions with maintenance of hemodynamic status and to know whether it is effective in improving the intubating conditions using propofol as induction agent and rocuronium (0.6 mg/kg) as neuromuscular blocking agent. This low dose might reduce the beta adrenergic adverse effects associated with higher doses of ephedrine like hypertension and tachycardia. In our study, ephedrine improved the intubating conditions without significant effects on hemodynamic parameters. However, previous studies compared the different doses of ephedrine with different induction agents and they didn’t find ephedrine effective at higher doses (>100 µg/kg) and found it detrimental for patients with low cardiac reserve as far as hemodynamic parameters are concerned.1-4,12,18 So with above hypothesis we only studied to find out the optimal low dose of ephedrine along with low dose of rocuronium which might be desirable in some situations.
In our study, we compared the intubating conditions between the ephedrine and control groups. Intubating condition is the principal qualitative measure for rapid sequence induction and intubation as it indicates whether the patient’s airway can be safely secured or not. The intubating conditions were significantly better in ephedrine group (Group A) as compared to saline group (Group B) (P < 0.05). The ephedrine group had acceptable intubating conditions in 84% of patients as compared to 40% of patients in saline group which concurs with the study done by Tan CH et al6 who found that intubating conditions were excellent (acceptable) in 84% of patients in propofol-ephedrine group as compared to 32% in propofol alone group. The improved intubating conditions were achieved at lower doses of rocuronium (0.6 mg/kg) at 60 seconds which is generally achieved using higher doses of rocuronium (0.9 mg/kg) in 60-90 seconds showed that ephedrine pretreatment reduced the onset time even at lower doses of rocuronium with acceptable intubating conditions. Our findings were also similar to the studies done by earlier researchers,1,2,12,14 who observed that intubating conditions were better in patients pretreated with ephedrine before induction and rapid tracheal intubation as they had used the similar doses of ephedrine and rocuronium and achieved acceptable intubating conditions in 60 seconds.9,15-17 However some authors had used different doses of ephedrine (70 – 210 µg/kg) in their studies and they found more better intubating conditions at higher doses of ephedrine even in 30 seconds but at the cost of significant hemodynamic variations which might be detrimental for patients with low cardiac reserve.4,18
In our study, the baseline HR were comparable between the two groups. The significant difference in mean HR was observed before induction (1 min after ephedrine pretreatment), after induction and after intubation (P < 0.05), but clinically it was not significant (within 20% change from their baseline values). In Group A, the increase in HR before induction was associated with ephedrine action, however, in Group B glycopyrrolate used as premedication may increase the HR but it was more significant in ephedrine group due to synergistic effect of ephedrine and glycopyrrolate.1,8,9 A significant reduction in HR was observed after induction in both groups (P<0.05), but more in saline group which can be due to induction with propofol alone. The HR again increased after intubation in both groups and persisted at higher values from their baseline values up to 10 min after induction in ephedrine group and up to 3 min in saline group. Again the action of ephedrine and intubation response might cause increase in HR significantly in ephedrine group but clinically not significant. Our findings were similar to the study done by Gopalkrishna et al1 who compared the effect of ephedrine on hemodynamic conditions in rapid induction of anesthesia with propofol and rocuronium and found favorable hemodynamic conditions during intubation and no significant difference among the ephedrine group; however, results were different and significant at higher doses of ephedrine. Our results also concurred with the findings of Karampal singh et al12 and Madhusudan et al.2,9,19
A significant rise in SBP before induction could be explained by pretreatment with ephedrine which increases cardiac output and after intubation, and due to stress response induced by laryngoscopy and intubation. However, after induction both groups showed significant decrease in SBP (P < 0.05) but more in saline group. This may be due to counter effect of ephedrine on propofol which leads to less reduction in SBP in ephedrine group as compared to saline group. The laryngoscopy and intubation induced increase in SBP was at its peak after 1 min in ephedrine group and remained stable thereafter and statistically insignificant between two groups throughout the study period.1,2 Our results were supported by the study done by Michelson et al7 who concluded that prophylactic injection of ephedrine significantly attenuated but did not completely abolish the decrease in blood pressure associated with induction of anesthesia with propofol and fentanyl. Similarly Gopalkrishna et al1 also found that pretreatment with ephedrine is effective in preventing hypotension after induction of anesthesia .However Masjedi et al20 reported that high dose of ephedrine (0.15 mg/kg) may have significant effect in preventing hypotension and bradycardia after induction with propofol and remifentanil which may be due to higher dose of ephedrine used in their study.
The MAP showed significant increase before induction (after ephedrine pretreatment) in ephedrine group from their baseline values (P < 0.05), which was statistically significant but clinically in acceptable range. The MAP remained near to baseline values after intubation in both groups and but statistically significant between two groups up to 5 min after intubation. The increase in MAP was on account of pretreatment with ephedrine as it was more pronounced in ephedrine group as compared to saline group but clinically insignificant (considering limits of 20% change from their baseline values). The MAP showed similar trends as SBP and found to be similar to the study done by Michelson et al, Gopalkrishna et al and Madhusudan et al found similar results in their study as they have used similar dose of ephedrine as we have used. The mean SpO2 remained comparable between two groups at all time intervals (P > 0.05).1,2,7-9
Limitations: Neuromuscular monitoring and cardiac output monitoring would make strong evidence to support our results while assessing intubating conditions, but we didn’t had these facilities at our institute.
CONCLUSION
The low dose ephedrine (70 µg/kg) and propofol combination before induction provides significantly better intubating conditions as compared to propofol alone, used with rocuronium. This combination allows rapid onset with acceptable intubating conditions even in one minute at low dose of rocuronium as higher doses (0.9-1.2 mg/kg) may be associated with prolonged duration of action which may be undesirable in various surgeries. The hemodynamic parameters were statistically different between two groups but clinically they were in acceptable range considering the limits of 20% change from their baseline values. No significant hypertension or tachycardia were observed but ephedrine prevents hypotension and bradycardia associated with propofol induction. However, precautions should always be taken in patients with limited cardiac reserve.
Declarations: No funding from any external source was used for the conduct of this study.
Ethical approval: Obtained from local institutional ethical committee.
Authors’ contribution: KJ: Concepts, literature review, manuscript editing and review
SKS: Literature search and review, manuscript preparation and editing
NJ: Concepts and design, manuscript review
SS: Literature search, conduction of study work
AK: Concepts, manuscript review
REFERENCES
- Gopalakrishna MD, Krishna HM, Shenoy UK. The effect of ephedrine on intubating conditions and haemodynamics during rapid tracheal intubation using propofol and rocuronium. Br J Anaesth. 2007 Aug;99(2):191-4. [PubMed] [Free full text]
- Madhusudan M, Rao MH, Reddy AKS, Kadiyala V, Samantaray A, Hemanth N, et al. Comparison of intubating conditions and haemodynamic responses during rapid tracheal intubation using either suxamethonium or rocuronium with ephedrine pretreatment. J Clin Sci Res. 2014;3:174-80.
- Gangaiah Y, Rao DG, Merrill S, Chandra SB. Hemodynamic changes during tracheal intubation using propofol and rocuronium after pre-treatment with ephedrine in adult patients. J Exp Integr Med. 2015;5(4):193-99. [Free full text]
- Magorian T, Flannery KB, Miller RD. Comparison of rocuronium, succinylcholine and vecuronium for rapid sequence induction of anesthesia in adult patients. Anesthesiology 1993; 79: 913–8. [PubMed] [Free full text]
- Muñoz HR, González AG, Dagnino JA, González JA, Pérez AE. The effect of ephedrine on the onset time of rocuronium. Anesth Analg. 1997 Aug;85(2):437-40. [PubMed]
- Tan CH, Onisong MK, Chiu WK. The influence of induction technique on intubating conditions 1 min after rocuronium administration: a comparison of a propofol-ephedrine combination and propofol. Anaesthesia. 2002;57:223–226. [PubMed] [Free full text]
- Michelsen I, Helbo-Hansen HS, Køhler F, Lorenzen AG, Rydlund E, Bentzon MW. Prophylactic ephedrine attenuates the hemodynamic response to propofol in elderly female patients. Anesth Analg 1998; 86: 477–81. [PubMed]
- Gamlin F, Freeman J, Winslow L, Berridge J, Vucevic M. The haemodynamic effects of propofol in combination with ephedrine in elderly patients (ASA groups 3 and 4). Anaesth Intensive Care 1999; 27: 477–8. [PubMed] [Free full text]
- Gamlin F, Vucevic M, Winslow L, Berridge J. The haemodynamic effects of propofol in combination with ephedrine. Anaesthesia 1996; 51: 488–91. [PubMed] [Free full text]
- Ittichaikulthol W, Sriswasdi S, Nualon S, Hongpuang S, Sornil A. The effect of ephedrine on the onset time of rocuronium in Thai patients. J Med Assoc Thai. 2004;87:264-9. [PubMed]
- Ezri T, Szmuk P, Warters RD, Gebhard RE, Pivalizza EG, Katz J. Changes in onset time of rocuronium in patients pretreated with ephedrine and esmolol—the role of cardiac output. Acta Anaesthesiol Scand. 2003 Oct;47(9):1067-72. [PubMed]
- Singh K, Singhal S, Raghove P. A study to evaluate effect of ephedrine on intubating conditions and haemodynamic parameters using low doses rocuronium with different induction agents. Int J Pharmacol and Clin Sci. 2013;2:9-13. [Free full text]
- Han DW, Chun DH, Kweon TD, Shin YS. Significance of the injection timing of ephedrine to reduce the onset time of rocuronium. Anaesthesia. 2008 Aug;63(8):856-60. doi: 10.1111/j.1365-2044.2008.05497.x. [PubMed] [Free full text]
- Leykin Y, Pellis T, Lucca M, Gullo A. Effects of ephedrine on intubating conditions following priming with rocuronium. Acta anaesthesiol Scand 2005;49:792-7. [PubMed]
- Albert F, Hans P, Bitar Y, Brichant JF, De-wandre PY, Lamy M. Effects of ephedrine on the onset time of neuromuscular block and intubating conditions after cisatracurium: preliminary results. Acta Anaesthesiol Belg. 2000;51:167-71. [PubMed]
- Iqbal U, Ali K, Khan A, Sheikh F, Shafique F. The Effect of Bolus Dose of Ephedrine on the Onset Time of Vecuronium. Pak J Med Health Sci. 2012;6(4):1038-42.
- Alim SMA, Hossain MM, Khatun UHS. Effect of ephedrine on rapid intubation and haemodynamics using propofol and rocuronium: A randomized controlled trial.J Bangla Soc Anaesth. 2009;22(1):16-20.
- Sparr HJ, Giesinger S, Ulmer H, Hollenstein-Zacke M, Luger TJ. Influence of induction technique on intubating conditions after rocuronium in adults: comparison with rapid-sequence induction using thiopentone and suxamethonium. Br J Anaesth.1996 Sep;77(3):339-42. [PubMed] [Free full text]
- Chow MYH, Sim KM, Sia AT, Chan YW. Haemodynamic effects of adding ephedrine to propofol and alfentanil. Can J Anaesth. 1998 Jun;45(6):597-8.. [PubMed]
- Masjedi M, Zand F, Kazemi AP, Hoseinipour A. Prophylactic effect of ephedrine to reduce hemodynamic changes associated with anesthesia induction with propofol and remifentanil. J Anaesthesiol Clin Pharmacol. 2014 Apr;30(2):217-21. doi: 10.4103/0970-9185.130024. [PubMed] [Free full text]