Renu Bala1, Arjun Pirkad2, Savita Saini3, Arnab Banerjee2
1Associate Professor; 2Resident; 3Professor
Department of Anesthesiology & Critical care, Pt BD Sharma PGIMS, Rohtak, Haryana.
Correspondence: Dr. Arjun Pirkad, Department of Anesthesiology & Critical Care, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences (PGIMS), Medical Rd, Rohtak, Haryana 124001 (India); E-mail: dr.arnab77@gmail.com
ABSTRACT
Though the condition Eisenmenger syndrome (ES) is quite rare, the patients may present for incidental surgeries. The anesthetic management is quite daunting in such patients since the physiological changes occurring during anesthesia may adversely affect the shunt. The perioperative mortality is quite high and ranges from 4% to 30%. The choice of anesthesia remains a controversial subject and the best technique is still not defined. We herein report a 23year old male patient who was a known case of ES scheduled to undergo inguinal hernia repair. We planned the surgery under local anesthetic infiltration at the site and ilioinguinal nerve block. However the desired effect of local anesthetics was not obtained and the further anesthetic management of the patient was very challenging task.
Key words: Eisenmenger syndrome; Inguinal hernia; Surgery; Anesthesia,
Citation: Bala R, Pirkad A, Saini S, Banerjee A. Anesthetic management of a patient with Eisenmenger syndrome: What next when one technique fails? Anaesth Pain & Intensive Care 2016;20(3):327-329
Received: 25 June 2016; Reviewed: 6 & 9 September 2016; Corrected: 12 September 2016; Accepted: 15 September 2016
INTRODUCTION
Eisenmenger syndrome (ES) was first described by Victor Eisenmenger in1897 but the term was coined by Wood in 1958. The ES consists of pulmonary hypertension (PHT) with a reversed or bidirectional shunt at the atrio-ventricular or aorto-pulmonary level.1 These patients may survive into adulthood and thus the prospects of incidental surgeries are increasing. Their compromised cardiovascular system is particularly vulnerable to alteration in hemodynamics induced by anesthetics or surgery. The mortality rate is understandably high and may reach upto 30%.2
Different anesthetic techniques including general and regional have been employed in these patients but the best technique is still controversial.3 We hereby report a patient who was a known case of ES and scheduled to undergo hernioplasty of inguinal hernia. The surgery was planned under local anesthetic infiltration and ilioinguinal nerve block. But the desired effect of anesthesia was not achieved turning it a true conundrum.
CASE REPORT
A 23 year old male patient with a BMI -21 and ASA-class-III, was admitted for elective inguinal hernioplasty. He was a known case of Eisenmenger syndrome diagnosed 8months back and was on tablet sildenafil 50mg 8hrly since 15days. There were complaints of exertional dyspnea (NYHA Grade=II), metabolic equivalent task (MET) score was 3. Physical examination revealed clubbing and peripheral cyanosis. Jugular venous pressure was not raised and there was no pedal edema. His vitals were BP-100/54mmHg, Pulse-54bpm, and Spo2(on room air) was 89%. On auscultation the lungs were clear and there was loud P2 with pansystolic murmur over left sternal border. Hemoglobin was 15gm/dl with hematocrit 50% and rest of the hematological and biochemical investigations were unremarkable. Arterial blood gases revealed pH 7.43, PaO2 52.3 mmHg, PaCO2 42.6 mmHg, HCO3 18, BE -4, SaO2 80%. Echocardiographic findings were left ventricular ejection fraction (LVEF) 38%, severe tricuspid regurgitation, severe pulmonary hypertension, dilated right atrium and right ventricle, pulmonary artery dilatation, large muscular ventricular septal defect (VSD) 2 cm in size with reverse of shunt R→L, and no clots (Figure 1). Chest x-ray showed left atrial dilatation and mild cardiomegaly (Figure 2).
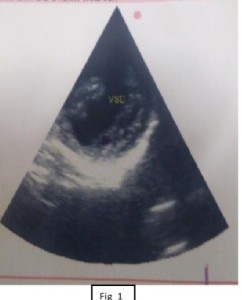
Figure 1: Echocardiographic findings were left ventricular ejection fraction 38%, severe tricuspid regurgitation, severe pulmonary hypertension, dilated right atrium and right ventricle, pulmonary artery dilatation, large muscular ventricular septal defect and reverse shunt R→L.

Figure 2: Chest x-ray showing left atrial dilatation and mild cardiomegaly
Preoperative fasting was prescribed after midnight and premedication was given in the form of tablet ranitidine150mg and tablet alprazolam 0.25mg orally the night before surgery. Infective endocarditis prophylaxis was also administered. In the operating room routine monitors including heart rate (HR), ECG, non-invasive blood pressure (NIBP), pulse-oximetry and temperature (axillary) probe were attached. Ilioinguinal nerve block was given using landmark technique. 10 ml of 0.25% bupivacaine was injected and additional 15 ml was infiltrated at the local site by the surgeons. Injection midazolam 1mg was given intravenously to allay anxiety and oxygen administered via nasal prongs with a facility to monitor end-tidal carbon dioxide. The desired effect of anesthetics was not obtained and the patient complained of pain when the surgical incision was made. It was supplemented with injection fentanyl 50mcg intravenously but the patient still had pain (VAS=7). His heart rate increased to 112 bpm, BP was 150/100 mmHg, the ECG showed occasional ectopic beats and SpO2 was 96%. The next line of management was a dilemma as the cocktail of further drugs could have been detrimental.
General anesthesia was induced with sleep dose of inj. thiopentone (150 mg) administered slowly followed by vecuronium 4mg intravenously for neuromuscular relaxation. Proseal LMA of size 4 was inserted successfully. Maintenance of anesthesia was done with oxygen and sevoflurane; fentanyl 50 µg was repeated for analgesia. The surgery took 45 min during which 750 ml of ringer lactate was infused and the patient remained hemodynamically stable. The rest of the intraoperative period and recovery was uneventful. The patient was observed in recovery room for half an hour and kept in high dependency unit (HDU) overnight. He was discharged asymptomatic on 4th postoperative day.
DISCUSSION
The anesthetic management of patients with ES pose unique and difficult challenge for the anesthesiologist. The main anesthetic goal remains the avoidance of fall in arterial blood pressure by maintaining both the cardiac output and systemic vascular resistance (SVR).4 Traditionally general anesthesia was considered as a method of choice since blockade of sympathetic nerve fibres associated with regional blockade (spinal anesthesia and epidural anesthesia) may result in decrease in SVR and subsequently worsening of shunt. However general anesthesia and positive pressure ventilation too can lead to decrease in vascular resistance and cardiac output.5 A review noted that mortality rate was significantly higher in patients receiving general anesthesia but the authors commented that the risk is related to the surgical disease and the surgery itself and probably not the anesthetics.3
Hernioplasty can be performed under various anesthetic techniques, and local anesthetic infiltration along with ilioinguinal and iliohypogastric nerve block is considered as a safe, simple and effective technique.6,7 Moreover, side effects of general anesthetics can be avoided. The failure of block left us stranded. Probably ultrasound guided nerve block might have been a better option but the lack of expertise was the main deterrent. Though ketamine is preferred in these patients, and our patient already had tachycardia and sympathetic stimulation can lead to increased pulmonary hypertension.8 Titrated doses of thiopentone were used as induction agent to prevent fall in BP. Use of supraglottic airway device produces less sympathetic stimulation than direct laryngoscopy and intubation. All intravenous lines were carefully flushed to prevent air embolism. It was prudent to avoid nitrous oxide due to its added effect on pulmonary vascular resistance. Prevention of hypoxia, hypercarbia, acidosis and hypothermia are very crucial. Hypovolemia needs to be prevented, therefore fasting and intraoperative fluid were carefully planned.1
Both invasive and noninvasive monitoring has been advocated in similar patients. One should weigh the risks and benefits. Intra-arterial blood pressure monitoring has the advantage of continuous BP reading, but there are risks of thrombosis due to hyperviscosity.9 Moreover, fluid shifts were not expected in our patient, so we preferred NIBP monitoring which was adjusted to record every 3 minutes.
Sildenafil is considered to be very effective in decreasing pulmonary hypertension since it inhibits degradation of cyclic guanosine monophosphate (cGMP) which is instrumental in relaxing smooth muscles of pulmonary vasculature thereby decreasing pulmonary hypertension. L-arginine, inhaled nitric oxide, and newer agents like epoprostenol and bosentan are also considered beneficial in such patients.1
CONCLUSION
Our case report adds to the fact that adequate and meticulous planning is the cornerstone of successful management of such high risk patients. It is conceivable that one should have an alternate plan of anesthetic management which can be embarked upon if needed. It will prevent plethora of events such as hemodynamic alterations which can prove detrimental to a compromised heart.
Conflict of interest: None declared by the authors
Author contribution: All authors have contributed equally for this case report.
REFERENCES
1Associate Professor; 2Resident; 3Professor
Department of Anesthesiology & Critical care, Pt BD Sharma PGIMS, Rohtak, Haryana.
Correspondence: Dr. Arjun Pirkad, Department of Anesthesiology & Critical Care, Pandit Bhagwat Dayal Sharma Post Graduate Institute of Medical Sciences (PGIMS), Medical Rd, Rohtak, Haryana 124001 (India); E-mail: dr.arnab77@gmail.com
ABSTRACT
Though the condition Eisenmenger syndrome (ES) is quite rare, the patients may present for incidental surgeries. The anesthetic management is quite daunting in such patients since the physiological changes occurring during anesthesia may adversely affect the shunt. The perioperative mortality is quite high and ranges from 4% to 30%. The choice of anesthesia remains a controversial subject and the best technique is still not defined. We herein report a 23year old male patient who was a known case of ES scheduled to undergo inguinal hernia repair. We planned the surgery under local anesthetic infiltration at the site and ilioinguinal nerve block. However the desired effect of local anesthetics was not obtained and the further anesthetic management of the patient was very challenging task.
Key words: Eisenmenger syndrome; Inguinal hernia; Surgery; Anesthesia,
Citation: Bala R, Pirkad A, Saini S, Banerjee A. Anesthetic management of a patient with Eisenmenger syndrome: What next when one technique fails? Anaesth Pain & Intensive Care 2016;20(3):327-329
Received: 25 June 2016; Reviewed: 6 & 9 September 2016; Corrected: 12 September 2016; Accepted: 15 September 2016
INTRODUCTION
Eisenmenger syndrome (ES) was first described by Victor Eisenmenger in1897 but the term was coined by Wood in 1958. The ES consists of pulmonary hypertension (PHT) with a reversed or bidirectional shunt at the atrio-ventricular or aorto-pulmonary level.1 These patients may survive into adulthood and thus the prospects of incidental surgeries are increasing. Their compromised cardiovascular system is particularly vulnerable to alteration in hemodynamics induced by anesthetics or surgery. The mortality rate is understandably high and may reach upto 30%.2
Different anesthetic techniques including general and regional have been employed in these patients but the best technique is still controversial.3 We hereby report a patient who was a known case of ES and scheduled to undergo hernioplasty of inguinal hernia. The surgery was planned under local anesthetic infiltration and ilioinguinal nerve block. But the desired effect of anesthesia was not achieved turning it a true conundrum.
CASE REPORT
A 23 year old male patient with a BMI -21 and ASA-class-III, was admitted for elective inguinal hernioplasty. He was a known case of Eisenmenger syndrome diagnosed 8months back and was on tablet sildenafil 50mg 8hrly since 15days. There were complaints of exertional dyspnea (NYHA Grade=II), metabolic equivalent task (MET) score was 3. Physical examination revealed clubbing and peripheral cyanosis. Jugular venous pressure was not raised and there was no pedal edema. His vitals were BP-100/54mmHg, Pulse-54bpm, and Spo2(on room air) was 89%. On auscultation the lungs were clear and there was loud P2 with pansystolic murmur over left sternal border. Hemoglobin was 15gm/dl with hematocrit 50% and rest of the hematological and biochemical investigations were unremarkable. Arterial blood gases revealed pH 7.43, PaO2 52.3 mmHg, PaCO2 42.6 mmHg, HCO3 18, BE -4, SaO2 80%. Echocardiographic findings were left ventricular ejection fraction (LVEF) 38%, severe tricuspid regurgitation, severe pulmonary hypertension, dilated right atrium and right ventricle, pulmonary artery dilatation, large muscular ventricular septal defect (VSD) 2 cm in size with reverse of shunt R→L, and no clots (Figure 1). Chest x-ray showed left atrial dilatation and mild cardiomegaly (Figure 2).
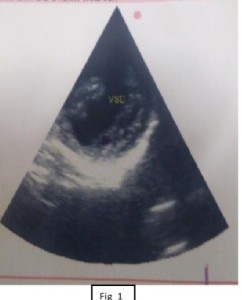
Figure 1: Echocardiographic findings were left ventricular ejection fraction 38%, severe tricuspid regurgitation, severe pulmonary hypertension, dilated right atrium and right ventricle, pulmonary artery dilatation, large muscular ventricular septal defect and reverse shunt R→L.

Figure 2: Chest x-ray showing left atrial dilatation and mild cardiomegaly
Preoperative fasting was prescribed after midnight and premedication was given in the form of tablet ranitidine150mg and tablet alprazolam 0.25mg orally the night before surgery. Infective endocarditis prophylaxis was also administered. In the operating room routine monitors including heart rate (HR), ECG, non-invasive blood pressure (NIBP), pulse-oximetry and temperature (axillary) probe were attached. Ilioinguinal nerve block was given using landmark technique. 10 ml of 0.25% bupivacaine was injected and additional 15 ml was infiltrated at the local site by the surgeons. Injection midazolam 1mg was given intravenously to allay anxiety and oxygen administered via nasal prongs with a facility to monitor end-tidal carbon dioxide. The desired effect of anesthetics was not obtained and the patient complained of pain when the surgical incision was made. It was supplemented with injection fentanyl 50mcg intravenously but the patient still had pain (VAS=7). His heart rate increased to 112 bpm, BP was 150/100 mmHg, the ECG showed occasional ectopic beats and SpO2 was 96%. The next line of management was a dilemma as the cocktail of further drugs could have been detrimental.
General anesthesia was induced with sleep dose of inj. thiopentone (150 mg) administered slowly followed by vecuronium 4mg intravenously for neuromuscular relaxation. Proseal LMA of size 4 was inserted successfully. Maintenance of anesthesia was done with oxygen and sevoflurane; fentanyl 50 µg was repeated for analgesia. The surgery took 45 min during which 750 ml of ringer lactate was infused and the patient remained hemodynamically stable. The rest of the intraoperative period and recovery was uneventful. The patient was observed in recovery room for half an hour and kept in high dependency unit (HDU) overnight. He was discharged asymptomatic on 4th postoperative day.
DISCUSSION
The anesthetic management of patients with ES pose unique and difficult challenge for the anesthesiologist. The main anesthetic goal remains the avoidance of fall in arterial blood pressure by maintaining both the cardiac output and systemic vascular resistance (SVR).4 Traditionally general anesthesia was considered as a method of choice since blockade of sympathetic nerve fibres associated with regional blockade (spinal anesthesia and epidural anesthesia) may result in decrease in SVR and subsequently worsening of shunt. However general anesthesia and positive pressure ventilation too can lead to decrease in vascular resistance and cardiac output.5 A review noted that mortality rate was significantly higher in patients receiving general anesthesia but the authors commented that the risk is related to the surgical disease and the surgery itself and probably not the anesthetics.3
Hernioplasty can be performed under various anesthetic techniques, and local anesthetic infiltration along with ilioinguinal and iliohypogastric nerve block is considered as a safe, simple and effective technique.6,7 Moreover, side effects of general anesthetics can be avoided. The failure of block left us stranded. Probably ultrasound guided nerve block might have been a better option but the lack of expertise was the main deterrent. Though ketamine is preferred in these patients, and our patient already had tachycardia and sympathetic stimulation can lead to increased pulmonary hypertension.8 Titrated doses of thiopentone were used as induction agent to prevent fall in BP. Use of supraglottic airway device produces less sympathetic stimulation than direct laryngoscopy and intubation. All intravenous lines were carefully flushed to prevent air embolism. It was prudent to avoid nitrous oxide due to its added effect on pulmonary vascular resistance. Prevention of hypoxia, hypercarbia, acidosis and hypothermia are very crucial. Hypovolemia needs to be prevented, therefore fasting and intraoperative fluid were carefully planned.1
Both invasive and noninvasive monitoring has been advocated in similar patients. One should weigh the risks and benefits. Intra-arterial blood pressure monitoring has the advantage of continuous BP reading, but there are risks of thrombosis due to hyperviscosity.9 Moreover, fluid shifts were not expected in our patient, so we preferred NIBP monitoring which was adjusted to record every 3 minutes.
Sildenafil is considered to be very effective in decreasing pulmonary hypertension since it inhibits degradation of cyclic guanosine monophosphate (cGMP) which is instrumental in relaxing smooth muscles of pulmonary vasculature thereby decreasing pulmonary hypertension. L-arginine, inhaled nitric oxide, and newer agents like epoprostenol and bosentan are also considered beneficial in such patients.1
CONCLUSION
Our case report adds to the fact that adequate and meticulous planning is the cornerstone of successful management of such high risk patients. It is conceivable that one should have an alternate plan of anesthetic management which can be embarked upon if needed. It will prevent plethora of events such as hemodynamic alterations which can prove detrimental to a compromised heart.
Conflict of interest: None declared by the authors
Author contribution: All authors have contributed equally for this case report.
REFERENCES
- Joyce JA. Update for anesthetists.Eisenmenger syndrome: An anesthetic conundrum. AANA J. 2006 Jun;74(3):233-9. [PubMed]
- Selby DS, Sugden JC. Epidural anaesthesia for bilateral inguinal herniorrhaphy in Eisenmenger’s syndrome. Anaesthesia. 1989 Feb;44(2):130-2. [PubMed]
- Amnash NM, Connolly HM, Abel MD, Warnes CA. Noncardiac surgery in Eisenmenger syndrome. J Am Coll Cardiol. 1999 Jan;33(1):222-7. [PubMed] [Free full text]
- Saxena A, Chand T, Arya SK, Mittal A, Parimal. Total intravenous anaesthesia in a patient with Eisenmenger syndrome: Case report. J Anesth Clin Res. 2012;3:10. [Free full text]
- Martin JT, Tautz TJ, Antognini JF. Safety of regional anesthesia in Eisenmenger’s syndrome. Reg Anesth Pain Med. 2002 Sep-Oct;27(5):509-13. [PubMed]
- Sanjay P, Woodward A. Inguinal hernia repair: Local or general anaesthesia. Ann R Coll Surg Engl. 2007 Jul;89(5):497-503. [PubMed] [Free full text]
- Andersen FH, Nielsen K, Kehlet H. Combined ilioinguinal blockade and local infilteration anaesthesia for groin hernia repair-a double-blind randomized study. Br J 2005 Apr;94(4):520-3. [PubMed]. [Free full text]
- Khan ZH, Zeinaloo AA, Khan RH, Rasouli MR. Cardiac decompensation in a patient with Eisenmenger syndrome undergoing T5-T7 levels laminectomy in the sitting position. Turk Neurosurg. 2009;19:86–90. [PubMed] [Free full text]
- Gupta N, Kaur S, Goila A, Pawar M. Anaesthetic management of a patient with Eisenmenger syndrome and β-thalassemia major for splenectomy. Indian J Anaesth. 2011 Mar;55(2):187-9. doi: 10.4103/0019-5049.79892. [PubMed] [Free full text]