Anil K. Paswan*1, Shalini Gupta2, Shashi Prakash3, Rajeev K. Dubey4, Sandeep Khuba5, Virendra Rastogi6
1Associate Professor; 2Senior Resident; 3Assistant Professor; 6Professor
Department of Anesthesia, Institute of Medical Science, Banaras Hindu University, Varanasi, Uttar Pradesh 221005, (India)
4Associate Professor; 5Assistant Professor
Department of Anesthesia, Dr. Ram Manohar Lohia Institute of Medical Sciences, Gomti Nagar - Lucknow, Uttar Pradesh, (India)
*Correspondence: Dr. Anil K Paswan, C/6 New Medical Enclave, Banaras Hindu University, Varanasi, Uttar Pradesh 221005, (India); Cell: +919794855871; E-mail-dranil1973@gmail.com
ABSTRACT
Background: A variety of minimally invasive techniques (chemonucleolysis, laser, automated percutaneous discectomy, percutaneous manual nucleotomy) have been invented over the years, as treatment of low back pain related to disc disease. Automated percutaneous lumbar dissectomy (APLD), being one of these techniques, is a modality in which removal of nucleus pulposus, reduces intradiscal pressure thus relieves the nerve root compression and subsequently reduces radicular pain. This technique was introduced by Onik in 1985, referred to as ‘automated’ since it involves a mechanical probe, working by a ‘suction and cutting action for removal of the nucleus pulposus.
Methodology: After meeting the inclusion criteria, minimal invasive procedure - APLD, performed in between 2012 to 2015 on 120 patients on outdoor basis. Radicular discogenic pain was confirmed by MRI and clinical finding, procedure is being performed using nucleotome under fluoroscopic guidance.
Result: Based on patient satisfaction, 72 (60%) patients had excellent pain relief (75 – 100%), 34 (28.3%) had good pain relief (51–74%) whereas 14 (11.7%) patients had poor pain relief. Two (1.6%) patient developed discitis, which was the only complication and it resolved within fifteen days without sequelae.
Conclusion: Percutaneous decompression (APLD) techniques for intervertebral disc herniation are safe and cost-effective techniques with significant and long lasting results concerning pain reduction and mobility improvement. They can be proposed as initial treatment or attractive alternatives prior to major surgery.
Key words: Lumbar Prolapsed Intervertebral Disc; Nucleotome; discectomy; Intradiscal pressure; Lumbar radicular pain.
Received: 7 Jan 2016; Reviewed: 3 May, 7 Jul 2016; Corrected: 5 May, 12 May 2016; Accepted: 4 Nov 2016
INTRODUCTION
Back pain or radiculopathy related to herniated discs is an extremely common and a frequent cause of chronic disability. Symptoms of lumbar disc herniation (LDH) may start as low back pain (LBP), which then develops to radicular pain. A variety of minimally invasive techniques have been invented over the years as treatment of low back pain related to disc disease. Automated Percutaneous Lumbar Discectomy (APLD), being one of these techniques, is a modality in which removal of nucleus pulposus reduces intradiscal pressure and relieves the nerve root compression, subsequently reduce radicular pain. However , Maroon and Allen1 stated that the removal of an average of 2.5 grams of nucleus pulposus material from the disc ranging from one gram to 8 grams with no correlation with the outcomes. Percutaneous lumbar discectomy (PELD) was first described by Hijikata [2 in 1975 and represented a revolutionary concept in the semi invasive treatment of vertebral pain. APLD is an attractive method of treatment because of the minimally invasive nature and therefore the assumed that decrease in risk of structural damage to the nerves, muscles, bone, and ligaments. Hence the patients are expected to have day care procedure, less back pain, cost-effectiveness, minimal or no blood loss, and a shorter reconvalescence period than with conventional surgery. The actual relief of low back and radicular pain, might take more time slightly longer period to full recovery than after conventional.
METHODOLOGY
After approval of institutional research ethical, this prospective, descriptive study was conducted at a Pain Medicine Clinic, Department of Anesthesia, Institute of Medical Science, BHU, Varanasi, India, from February 2012 to May 2015.
The patients were first treated with conservative management, including medications and physical therapy. When conservative treatment proved unsuccessful, they were recommended treatment of APLD. Patients who met the inclusion criteria signed and informed written consent were taken from one hundred twenty patients with radicular and axial pain were included in this prospective, single-arm, observational study. Patient presenting with low back ache of discogenic origin to our Department were enrolled in the study. We included patients between 20 years to 65 years of age, presenting with low backache of discogenic origin with evidence on MRI, with disc protrusion < 6 mm. Other criteria were the axial back pain, radicular leg pain and lack of response to conservative management including medications and/or physical therapy.
Patients with spondylolisthesis and spinal fractures, infections or tumors, and for open discectomy, patients having sequestered disc having bladder and bowel involvement, with decreased height of disc (≤ 50%) on x-ray, patient having pain of other origin (including tuberculosis, facet joint arthropathy and severe bony stenosis, disc protrusion > 5 mm or sequestration, unstable spinal fracture or spinal instability, were also excluded. Other exclusion criteria were; pregnancy, infection at the injection site, coagulopathy and patients unable to provide informed consent.
All patients underwent magnetic resonance imaging (MRI) of the lumbosacral spine.
The procedure was monitored fluoroscopically, with the use of a C-arm. Once confirmed, the trocar can be safely advanced into the center of the disc using this anteroposterior view. The fluoroscope was then repositioned to obtain a lateral view, allowing the surgeon to confirm that the trocar's tip is correctly placed on both anteroposterior and lateral views. Once the trocar is in the correct position, the dilator and cannula are placed over the trocar and advanced until the annulus was reached. The dilator was then removed, and the cannula was pushed the extra few millimeters to rest on the annulus. The nucleotome was then placed into the disc. Once the aspiration probe was seen to be in the correct position in anteroposterior and lateral views, the port of the instrument was rotated toward the area of the herniation, the nucleotome console (Figure 1) was turned on, the footswitch pressed, and the disc aspiration was initiated (Figure 2).

Figure 1: Nucleotome console
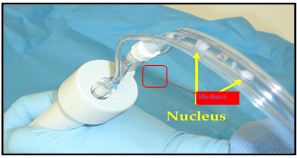

Figure 2: Intraoperative images taken after insertion of nucleotome, nucleus pulposus is seen within tube
Since the disc was avascular, the fluid flowing from the aspiration line should not be bloody. If the fluid has a red tinge, the most likely explanation was the presence of a gap between the cannula and the annulus that allows blood to be sucked into the disc from the surrounding soft tissues. It was likely the good results of APLD for discogenic pain are achieved by lowering the pressure within the disc. Duration of aspiration averages 15–20 minutes, and was stopped when the amount of nuclear material coming from the probe clearly decreases or when a blood tinged material starts coming, indicate that that the vascularized discovertebral cartilage was denuded. Probe was withdrawn into the cannula once no more material can be aspirated and Injected 20 mg methylprednisolone acetate and 1 ml bupivacaine 0.5% within the disc through 22 G aspiration needle. Patient will be followed for immediate and long term relief of pain, straight leg raising test, spinal tenderness, and improvement in neurological deficit if any. Patient will also be followed for immediate and long term complication including discitis, neurological deficit, bladder and bowel involvement. Technique-related complications include nerve root injury, osteomyelitis, cellulitis, uncontrolled bleeding, dural puncture, annular injury, and vertebral endplate injury were noted.
Postoperative care: After procedure patients remained under observation for 3-4 hours then sent back home with prescription of nonsteroidal anti-inflammatory agent, and gabapentin at bedtime for 2 weeks and encouraged to move, stand, and walk for few step on day five. Repetitive forward flexion/backward extension, prolonged car driving, prolonged sitting, and lifting heavy weights was prohibited for 3–4 weeks. Limb pain resolution may take weeks, owing to remodeling of the disc and regression of inflammation at the surgical site. Progressive return to heavy activities or sports is usually possible at 5-6 week.
RESULTS
Out of 120 patients, 75-85% patients were satisfied with this procedure. Blood loss was very minimal or no loss. Patients were operated as day care cases and discharge after 3-4 hours of post discectomy. The patients were observed for immediate and long term relief of pain and complications. In present study, all degrees of pain relief is shown in Table 1.
Table 1: Showing overall relief of pain
The mean pain score was 6.53 ± 1.112, in immediate post procedure period a slight decrease in mean pain score by 1.09 was observed on day one, but as the time passed a consistent decrease in pain scores, visual analogue score (VAS) was observed and at 6 months interval mean pain score was 2.10 ± 1.998 as compared to 6.53 ± 1.112 pre procedure which was statistically significant (p < 0.001) (Table 2).
Table 2: Comparison of VAS at different time interval
Fischer Exact test: p = 0.0249.
Seventy five percent patients in younger age group(20 – 29 years) showed excellent relief as compared to 40% patients in 30 – 49 years age group and 31.2% patients in ≥ 50 years age group as shown in Table 3.
Table 3: Influence of different factors on pain relief achieved
The patients presenting with acute pain (≤ 3 months duration) showed excellent pain relief in 71.4% patients as compared to 24% patients presenting with chronic pain (≥ 3 months duration) as shown in Table 3.
Best results were seen in patients with protruded central disc, as 65% (52 out of 80) patients showed excellent pain relief , whereas patients presenting with extruded disc with wide neck showed poor results , as 6 patients out of 36 (16.7%) could only demonstrate excellent relief. Substantial relief of pain (≥ 75%) was present in nearly 90% of patients with protruded disc as compared to 66.7% of patients with extruded disc (Table 3).
The influence of number of disc undergoing discectomy on pain relief is shown in Table 6. Best results (substantial pain relief) 96.77% were seen in patients with disc prolapse at one level as compared to 86.96% at two levels and worst 66.67% in patients with disc prolapse at more than two levels (Table 3).
Histopathology revealed degenerated disc in 66 patients contains fibrosed tissue, infiltrated WBCs and macrophages without an evidence of an infection; in the remaining 54 patients disc was normal (Figures 3 & 4).
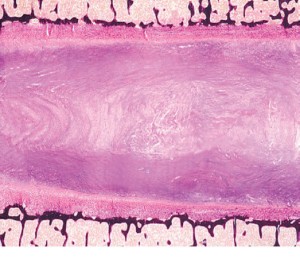
Figure 3: Normal disc on histopathological examination
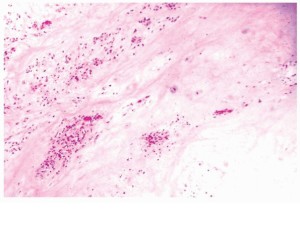
Figure. 4: Degenerated Disc with fibrosed tissue and infiltrated WBCs on histopathological examination
Patients with normal disc demonstrated excellent relief in 85.2% patients as compared to 21.2% patients with degenerated disc as shown in Table 3.
Oswestry disability index (ODI) showed a statistically significant (p < 0.001) decrease from its pre procedure level as shown in Table 4 at 3 months interval.
Table 4: Comparison of pre- and post-procedure (3 months) Oswestry disability index.
Fischer Exact test: p = 0.0249.
The incidence of discitis following APLD was observed in 2 (1.7%) patient, which responded to rest and antibiotic therapy (cap amoxycillin 500 mg 8 hourly for 2 weeks). Bladder dysfunction as evidenced by retention of urine was observed in 4 patients with L5/S1 extruded disc following APLD, which was recovered within three weeks after conservative treatment.
DISCUSSION
Often Patients respond well to non-operative management with acute lumbar disc herniation with the help of bed rest, analgesics, anti-inflammatory drugs, muscle relaxants.3 Those Patients who do not respond to conservative treatment or who have frequent recurrences that severely affect their quality of life are considered for surgical intervention like elective lumbar discectomy. The surgical technique is associated with high risk for developing approach-related complications. The overall results of standard discectomy range from 60 to 95% in different series.4 More than 3,00,000 lumbar discectomy procedures and 70,000 spinal fusion procedures are performed in the United States annually. The costs associated with the management of patients with various lumbar disorders have been estimated to exceed £16 Million per year in UK.5,6 Researchers all over the world are investigating and developing an alternate solutions, for example disc arthroplasty, nucleus pulposus replacement and biological therapies. There are several percutaneous options to remove disc material like APLD, nucleoplasty, RF discectomy, hydrodiscectomy and laser/endoscopy discectomy. The specific surgical goals are: to maintain a minimal annulotomy, to reach as many zones of the disc as possible and getting as much nuclear material out as possible and to avoid damage to the bony endplates, nerve, ligaments, and taking too much annulus fibrosus tissue.
The present study was done on 120 patients of either sex suffering from low backache of discogenic origin requiring automated percutaneous lumbar discectomy (APLD). The patients were followed for immediate and long term relief of pain and complications. The influence of various factors affecting the ultimate outcome like age, chronicity and duration of pain, neurological symptoms, radiological features and histopathology of disc were studied.
In this study overall substantial relief of pain was observed in 88.3% of patients undergoing APLD and was similar to other workers,7-9 where relief of pain ranges from 75% - 85% as shown in Table 1. It is clearly evident from these observations that the APLD when used in selected patients results in relief of pain in more than four fifth of patients, with minimal or no complications. However, some of the earlier workers10,11 reported a poor success rate [29% - 37% following APLD, but these reports of poor outcomes has been criticized especially for poor patient’s selection and becoming biased to the APLD procedures. The poor outcome might correlate poorly with the volume of disc material aspirated, and that failure is more likely with larger disc herniation. On the other hand Teng et al.12 and Maroon & Allen1 reported more than 80% of substantial pain relief.
A statistically significant (p < 0.001) pain relief as evidenced by decrease in VAS score from pre-procedure level at 6 months interval was observed following APLD. Similar observations were observed by earlier worker Alò KM13 who reported a mean reduction of VAS score by 60.2% at 6 month interval. Oswestry Disability Index (ODI) showed (Table 4) significantly decreases (19.60 ± 7.66) at 3 months interval from its pre procedure level (38.55 ± 11.57) which was better than observed by Grevitt et al.14 at 55 months interval, this discrepancy in the observation may be because of longer follow up of 55 months as compared to 6 months in our study.
Patients in age group of < 50 years reported 93.1% pain relief as compared to 50% pain relief in elderly patients (≥ 50 years) which was statistically significant (p < 0.0249). The increasing age results in poor outcome which was also reported by Teng et al.12 Maroon and Allen1, Bernd et al.15 and Bonaldi et al.8 However, Marks16 failed to observe a significant influence of age in pain relief which contradicts our observations.
There is definite influence of chronicity of pain in patients with low back ache of discogenic origin undergoing APLD (Table 3). Nearly 94.3% of patients showed substantial relief of pain with acute or subacute onset (< 3 months) as compared to 60% of the patients having pain of chronic onset (≥ 3 months ) and the difference was statistically significant (p < 0.072) .
The pathogenesis of low back ache as evidenced on radiology (MRI) and histopathology of disc certainly influence the outcome. Patients with protruded disc showed 90.5% pain relief as compared to 66.7% with extruded disc. Similar observations were also made by Teng et al (12) who reported 86% success rate in protruded disc as compared to 72% in extruded disc patients. From these observations it seems that the protruded disc is definitely an indication for APLD. In this series two third of patients with extruded disc with wider neck demonstrated substantial pain relief. If the number of disc involved is ≥ 2 the outcome is poor (33.3% pain relief) in comparison to 96% pain relief when one disc is involved and the difference was statistically significant (p < 0.020). The degenerated disc as evidenced by histopathology were associated with poor outcome (51.5% pain relief) as compared to patients having normal disc (96.3% pain relief) which was statistically significant (p < 0.001).
In our series two (1.7%) patients reported discitis following APLD, which responded to rest and antibiotic therapy and was similar to observations reported by earlier worker.17,18 However, Teng et al.12 reported 0.06% incidence of discitis following APLD which is definitely less than that observed in our series. Bladder dysfunction as evidenced by retention of urine was observed in four patients with L5/S1 extruded disc following APLD which was recovered within three week. None of the patients in this series had hematoma as compared to 0.2% by Onik et al.7 and 0.09% by Maroon & Allen.1 which was primarily related to technique.
Limitations of study: First, this study incorporates a prospective design and study should be randomized double blind manner. Sample size was very small and this technique can’t be applied in any type of lumbar disc herniation. Additionally, this is relatively a short-term follow-up study. We need further studies with long-term follow-up.
CONCLUSION
In our case series, this technique was shown to be safe and cost effective, low morbidity and can be performed under local anesthesia on an outpatient basis. Patients returned to work significantly sooner after percutaneous discectomy than after microdiscectomy or laminectomy. The operating time was significantly shorter and there were no approach-related complications, such as dural tear and/or permanent nerve root injury. Automated percutaneous lumbar discectomy is an effective minimally invasive surgical treatment alternative in patients with symptomatic contained disc herniation.
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
1Associate Professor; 2Senior Resident; 3Assistant Professor; 6Professor
Department of Anesthesia, Institute of Medical Science, Banaras Hindu University, Varanasi, Uttar Pradesh 221005, (India)
4Associate Professor; 5Assistant Professor
Department of Anesthesia, Dr. Ram Manohar Lohia Institute of Medical Sciences, Gomti Nagar - Lucknow, Uttar Pradesh, (India)
*Correspondence: Dr. Anil K Paswan, C/6 New Medical Enclave, Banaras Hindu University, Varanasi, Uttar Pradesh 221005, (India); Cell: +919794855871; E-mail-dranil1973@gmail.com
ABSTRACT
Background: A variety of minimally invasive techniques (chemonucleolysis, laser, automated percutaneous discectomy, percutaneous manual nucleotomy) have been invented over the years, as treatment of low back pain related to disc disease. Automated percutaneous lumbar dissectomy (APLD), being one of these techniques, is a modality in which removal of nucleus pulposus, reduces intradiscal pressure thus relieves the nerve root compression and subsequently reduces radicular pain. This technique was introduced by Onik in 1985, referred to as ‘automated’ since it involves a mechanical probe, working by a ‘suction and cutting action for removal of the nucleus pulposus.
Methodology: After meeting the inclusion criteria, minimal invasive procedure - APLD, performed in between 2012 to 2015 on 120 patients on outdoor basis. Radicular discogenic pain was confirmed by MRI and clinical finding, procedure is being performed using nucleotome under fluoroscopic guidance.
Result: Based on patient satisfaction, 72 (60%) patients had excellent pain relief (75 – 100%), 34 (28.3%) had good pain relief (51–74%) whereas 14 (11.7%) patients had poor pain relief. Two (1.6%) patient developed discitis, which was the only complication and it resolved within fifteen days without sequelae.
Conclusion: Percutaneous decompression (APLD) techniques for intervertebral disc herniation are safe and cost-effective techniques with significant and long lasting results concerning pain reduction and mobility improvement. They can be proposed as initial treatment or attractive alternatives prior to major surgery.
| Citation: Paswan AK, Gupta S, Prakash S, Dubey RK, Khuba S, Rastogi V. Automated percutaneous lumbar discectomy in patients suffering from prolapsed intervertebral disc: a prospective study. Anaesth Pain & Intensive Care 2016;20(4):429-435 |
Received: 7 Jan 2016; Reviewed: 3 May, 7 Jul 2016; Corrected: 5 May, 12 May 2016; Accepted: 4 Nov 2016
INTRODUCTION
Back pain or radiculopathy related to herniated discs is an extremely common and a frequent cause of chronic disability. Symptoms of lumbar disc herniation (LDH) may start as low back pain (LBP), which then develops to radicular pain. A variety of minimally invasive techniques have been invented over the years as treatment of low back pain related to disc disease. Automated Percutaneous Lumbar Discectomy (APLD), being one of these techniques, is a modality in which removal of nucleus pulposus reduces intradiscal pressure and relieves the nerve root compression, subsequently reduce radicular pain. However , Maroon and Allen1 stated that the removal of an average of 2.5 grams of nucleus pulposus material from the disc ranging from one gram to 8 grams with no correlation with the outcomes. Percutaneous lumbar discectomy (PELD) was first described by Hijikata [2 in 1975 and represented a revolutionary concept in the semi invasive treatment of vertebral pain. APLD is an attractive method of treatment because of the minimally invasive nature and therefore the assumed that decrease in risk of structural damage to the nerves, muscles, bone, and ligaments. Hence the patients are expected to have day care procedure, less back pain, cost-effectiveness, minimal or no blood loss, and a shorter reconvalescence period than with conventional surgery. The actual relief of low back and radicular pain, might take more time slightly longer period to full recovery than after conventional.
METHODOLOGY
After approval of institutional research ethical, this prospective, descriptive study was conducted at a Pain Medicine Clinic, Department of Anesthesia, Institute of Medical Science, BHU, Varanasi, India, from February 2012 to May 2015.
The patients were first treated with conservative management, including medications and physical therapy. When conservative treatment proved unsuccessful, they were recommended treatment of APLD. Patients who met the inclusion criteria signed and informed written consent were taken from one hundred twenty patients with radicular and axial pain were included in this prospective, single-arm, observational study. Patient presenting with low back ache of discogenic origin to our Department were enrolled in the study. We included patients between 20 years to 65 years of age, presenting with low backache of discogenic origin with evidence on MRI, with disc protrusion < 6 mm. Other criteria were the axial back pain, radicular leg pain and lack of response to conservative management including medications and/or physical therapy.
Patients with spondylolisthesis and spinal fractures, infections or tumors, and for open discectomy, patients having sequestered disc having bladder and bowel involvement, with decreased height of disc (≤ 50%) on x-ray, patient having pain of other origin (including tuberculosis, facet joint arthropathy and severe bony stenosis, disc protrusion > 5 mm or sequestration, unstable spinal fracture or spinal instability, were also excluded. Other exclusion criteria were; pregnancy, infection at the injection site, coagulopathy and patients unable to provide informed consent.
All patients underwent magnetic resonance imaging (MRI) of the lumbosacral spine.
The procedure was monitored fluoroscopically, with the use of a C-arm. Once confirmed, the trocar can be safely advanced into the center of the disc using this anteroposterior view. The fluoroscope was then repositioned to obtain a lateral view, allowing the surgeon to confirm that the trocar's tip is correctly placed on both anteroposterior and lateral views. Once the trocar is in the correct position, the dilator and cannula are placed over the trocar and advanced until the annulus was reached. The dilator was then removed, and the cannula was pushed the extra few millimeters to rest on the annulus. The nucleotome was then placed into the disc. Once the aspiration probe was seen to be in the correct position in anteroposterior and lateral views, the port of the instrument was rotated toward the area of the herniation, the nucleotome console (Figure 1) was turned on, the footswitch pressed, and the disc aspiration was initiated (Figure 2).

Figure 1: Nucleotome console
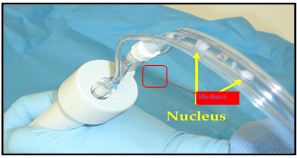

Figure 2: Intraoperative images taken after insertion of nucleotome, nucleus pulposus is seen within tube
Since the disc was avascular, the fluid flowing from the aspiration line should not be bloody. If the fluid has a red tinge, the most likely explanation was the presence of a gap between the cannula and the annulus that allows blood to be sucked into the disc from the surrounding soft tissues. It was likely the good results of APLD for discogenic pain are achieved by lowering the pressure within the disc. Duration of aspiration averages 15–20 minutes, and was stopped when the amount of nuclear material coming from the probe clearly decreases or when a blood tinged material starts coming, indicate that that the vascularized discovertebral cartilage was denuded. Probe was withdrawn into the cannula once no more material can be aspirated and Injected 20 mg methylprednisolone acetate and 1 ml bupivacaine 0.5% within the disc through 22 G aspiration needle. Patient will be followed for immediate and long term relief of pain, straight leg raising test, spinal tenderness, and improvement in neurological deficit if any. Patient will also be followed for immediate and long term complication including discitis, neurological deficit, bladder and bowel involvement. Technique-related complications include nerve root injury, osteomyelitis, cellulitis, uncontrolled bleeding, dural puncture, annular injury, and vertebral endplate injury were noted.
Postoperative care: After procedure patients remained under observation for 3-4 hours then sent back home with prescription of nonsteroidal anti-inflammatory agent, and gabapentin at bedtime for 2 weeks and encouraged to move, stand, and walk for few step on day five. Repetitive forward flexion/backward extension, prolonged car driving, prolonged sitting, and lifting heavy weights was prohibited for 3–4 weeks. Limb pain resolution may take weeks, owing to remodeling of the disc and regression of inflammation at the surgical site. Progressive return to heavy activities or sports is usually possible at 5-6 week.
RESULTS
Out of 120 patients, 75-85% patients were satisfied with this procedure. Blood loss was very minimal or no loss. Patients were operated as day care cases and discharge after 3-4 hours of post discectomy. The patients were observed for immediate and long term relief of pain and complications. In present study, all degrees of pain relief is shown in Table 1.
Table 1: Showing overall relief of pain
| Pain relief | n (%) |
| Excellent (75 – 100 %) | 72 (60) |
| Good (51 – 74%) | 34 (28.3) |
| Poor ( ≤ 50% ) | 14 (11.7) |
| Total | 120 (100) |
Table 2: Comparison of VAS at different time interval
| Time interval | Mean ± SD | Median (IQR) | p-value |
| Pre procedure | 6.53 ± 1.112 | 7 (6-7) | - |
| Post procedure | 5.44 ± 1.027 | 6 (5-6) | < 0.001 |
| Day 1 | 4.68 ± 1.376 | 5 (4-6) | < 0.001 |
| Day 15 | 4.06 ± 1.657 | 4 (3-5) | < 0.001 |
| 1 month | 3.45 ± 1.660 | 4 (2.5-4.5) | < 0.001 |
| 3 month | 2.60 ± 1.429 | 3 (2-3) | < 0.001 |
| 6 month | 2.10 ± 1.998 | 2 (0-3) | < 0.001 |
Seventy five percent patients in younger age group(20 – 29 years) showed excellent relief as compared to 40% patients in 30 – 49 years age group and 31.2% patients in ≥ 50 years age group as shown in Table 3.
Table 3: Influence of different factors on pain relief achieved
| Parameter | Excellent
n (%) |
Good
n (%) |
Poor
n (%) |
Total
n=120 |
|
| Age | 20-29 | 36 (75) | 12 (25) | 0 (0) | 48 |
| 30-49 | 16 (40) | 18 (45) | 6 (15) | 40 | |
| ≥50 | 10 (31.2) | 6 (18.8) | 16 (50) | 32 | |
| Chronicity | Acute(≤ 3 months) | 50 (71.4) | 16 (22.8) | 4 (5.7) | 70 |
| Chronic(≥ 3 months) | 12 (24) | 18 (36) | 20 (40) | 50 | |
| MRI findings | Protruded central | 52 (65) | 20 (25) | 8 (10) | 80 |
| Protruded paracentral | 2 (50) | 2 (50) | 0 (0) | 4 | |
| Extruded wide neck | 6 (16.7) | 18 (50) | 12 (33.3) | 36 | |
| No. of lumbar vertebral levels involved | 1 | 40 (64.5) | 20 (32.2) | 2 (3.2) | 62 |
| 2 | 26 (56.5) | 14 (30.4) | 6 (13) | 46 | |
| > 2 | 4 (33.3) | 0 | 8 (66.7) | 12 | |
| Biopsy findings | Normal | 46 (85.2) | 6 (11.1) | 2 (3.7) | 54 |
| Degenerated | 14 (21.2) | 20 (30.3) | 32 (48.5) | 66 | |
The patients presenting with acute pain (≤ 3 months duration) showed excellent pain relief in 71.4% patients as compared to 24% patients presenting with chronic pain (≥ 3 months duration) as shown in Table 3.
Best results were seen in patients with protruded central disc, as 65% (52 out of 80) patients showed excellent pain relief , whereas patients presenting with extruded disc with wide neck showed poor results , as 6 patients out of 36 (16.7%) could only demonstrate excellent relief. Substantial relief of pain (≥ 75%) was present in nearly 90% of patients with protruded disc as compared to 66.7% of patients with extruded disc (Table 3).
The influence of number of disc undergoing discectomy on pain relief is shown in Table 6. Best results (substantial pain relief) 96.77% were seen in patients with disc prolapse at one level as compared to 86.96% at two levels and worst 66.67% in patients with disc prolapse at more than two levels (Table 3).
Histopathology revealed degenerated disc in 66 patients contains fibrosed tissue, infiltrated WBCs and macrophages without an evidence of an infection; in the remaining 54 patients disc was normal (Figures 3 & 4).
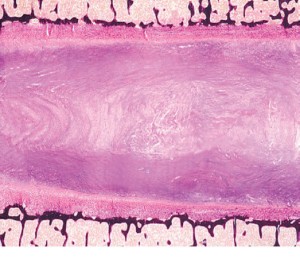
Figure 3: Normal disc on histopathological examination
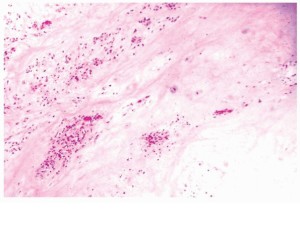
Figure. 4: Degenerated Disc with fibrosed tissue and infiltrated WBCs on histopathological examination
Patients with normal disc demonstrated excellent relief in 85.2% patients as compared to 21.2% patients with degenerated disc as shown in Table 3.
Oswestry disability index (ODI) showed a statistically significant (p < 0.001) decrease from its pre procedure level as shown in Table 4 at 3 months interval.
Table 4: Comparison of pre- and post-procedure (3 months) Oswestry disability index.
| Period | ODI (Mean ± SD) | p-value |
| Preoperative | 38.55 ± 11.57 | < 0.001 |
| Postoperative (3 months) | 19.60 ± 7.66 |
The incidence of discitis following APLD was observed in 2 (1.7%) patient, which responded to rest and antibiotic therapy (cap amoxycillin 500 mg 8 hourly for 2 weeks). Bladder dysfunction as evidenced by retention of urine was observed in 4 patients with L5/S1 extruded disc following APLD, which was recovered within three weeks after conservative treatment.
DISCUSSION
Often Patients respond well to non-operative management with acute lumbar disc herniation with the help of bed rest, analgesics, anti-inflammatory drugs, muscle relaxants.3 Those Patients who do not respond to conservative treatment or who have frequent recurrences that severely affect their quality of life are considered for surgical intervention like elective lumbar discectomy. The surgical technique is associated with high risk for developing approach-related complications. The overall results of standard discectomy range from 60 to 95% in different series.4 More than 3,00,000 lumbar discectomy procedures and 70,000 spinal fusion procedures are performed in the United States annually. The costs associated with the management of patients with various lumbar disorders have been estimated to exceed £16 Million per year in UK.5,6 Researchers all over the world are investigating and developing an alternate solutions, for example disc arthroplasty, nucleus pulposus replacement and biological therapies. There are several percutaneous options to remove disc material like APLD, nucleoplasty, RF discectomy, hydrodiscectomy and laser/endoscopy discectomy. The specific surgical goals are: to maintain a minimal annulotomy, to reach as many zones of the disc as possible and getting as much nuclear material out as possible and to avoid damage to the bony endplates, nerve, ligaments, and taking too much annulus fibrosus tissue.
The present study was done on 120 patients of either sex suffering from low backache of discogenic origin requiring automated percutaneous lumbar discectomy (APLD). The patients were followed for immediate and long term relief of pain and complications. The influence of various factors affecting the ultimate outcome like age, chronicity and duration of pain, neurological symptoms, radiological features and histopathology of disc were studied.
In this study overall substantial relief of pain was observed in 88.3% of patients undergoing APLD and was similar to other workers,7-9 where relief of pain ranges from 75% - 85% as shown in Table 1. It is clearly evident from these observations that the APLD when used in selected patients results in relief of pain in more than four fifth of patients, with minimal or no complications. However, some of the earlier workers10,11 reported a poor success rate [29% - 37% following APLD, but these reports of poor outcomes has been criticized especially for poor patient’s selection and becoming biased to the APLD procedures. The poor outcome might correlate poorly with the volume of disc material aspirated, and that failure is more likely with larger disc herniation. On the other hand Teng et al.12 and Maroon & Allen1 reported more than 80% of substantial pain relief.
A statistically significant (p < 0.001) pain relief as evidenced by decrease in VAS score from pre-procedure level at 6 months interval was observed following APLD. Similar observations were observed by earlier worker Alò KM13 who reported a mean reduction of VAS score by 60.2% at 6 month interval. Oswestry Disability Index (ODI) showed (Table 4) significantly decreases (19.60 ± 7.66) at 3 months interval from its pre procedure level (38.55 ± 11.57) which was better than observed by Grevitt et al.14 at 55 months interval, this discrepancy in the observation may be because of longer follow up of 55 months as compared to 6 months in our study.
Patients in age group of < 50 years reported 93.1% pain relief as compared to 50% pain relief in elderly patients (≥ 50 years) which was statistically significant (p < 0.0249). The increasing age results in poor outcome which was also reported by Teng et al.12 Maroon and Allen1, Bernd et al.15 and Bonaldi et al.8 However, Marks16 failed to observe a significant influence of age in pain relief which contradicts our observations.
There is definite influence of chronicity of pain in patients with low back ache of discogenic origin undergoing APLD (Table 3). Nearly 94.3% of patients showed substantial relief of pain with acute or subacute onset (< 3 months) as compared to 60% of the patients having pain of chronic onset (≥ 3 months ) and the difference was statistically significant (p < 0.072) .
The pathogenesis of low back ache as evidenced on radiology (MRI) and histopathology of disc certainly influence the outcome. Patients with protruded disc showed 90.5% pain relief as compared to 66.7% with extruded disc. Similar observations were also made by Teng et al (12) who reported 86% success rate in protruded disc as compared to 72% in extruded disc patients. From these observations it seems that the protruded disc is definitely an indication for APLD. In this series two third of patients with extruded disc with wider neck demonstrated substantial pain relief. If the number of disc involved is ≥ 2 the outcome is poor (33.3% pain relief) in comparison to 96% pain relief when one disc is involved and the difference was statistically significant (p < 0.020). The degenerated disc as evidenced by histopathology were associated with poor outcome (51.5% pain relief) as compared to patients having normal disc (96.3% pain relief) which was statistically significant (p < 0.001).
In our series two (1.7%) patients reported discitis following APLD, which responded to rest and antibiotic therapy and was similar to observations reported by earlier worker.17,18 However, Teng et al.12 reported 0.06% incidence of discitis following APLD which is definitely less than that observed in our series. Bladder dysfunction as evidenced by retention of urine was observed in four patients with L5/S1 extruded disc following APLD which was recovered within three week. None of the patients in this series had hematoma as compared to 0.2% by Onik et al.7 and 0.09% by Maroon & Allen.1 which was primarily related to technique.
Limitations of study: First, this study incorporates a prospective design and study should be randomized double blind manner. Sample size was very small and this technique can’t be applied in any type of lumbar disc herniation. Additionally, this is relatively a short-term follow-up study. We need further studies with long-term follow-up.
CONCLUSION
In our case series, this technique was shown to be safe and cost effective, low morbidity and can be performed under local anesthesia on an outpatient basis. Patients returned to work significantly sooner after percutaneous discectomy than after microdiscectomy or laminectomy. The operating time was significantly shorter and there were no approach-related complications, such as dural tear and/or permanent nerve root injury. Automated percutaneous lumbar discectomy is an effective minimally invasive surgical treatment alternative in patients with symptomatic contained disc herniation.
Source of Support: Nil
Conflict of Interest: None.
Acknowledgements: We would like to thanks the OR staff, specially Mr. Shasikant Panday and Pain Management team for their work in making this trial possible.
Authors’ contribution: All of the authors took part in the conduction of the study, data search and manuscript preparation.REFERENCES
- Maroon JC, Allen AC. A retrospective study of 1,054 APLD cases: A twenty month clinical follow-up at 35 US centers. J Neurol Orthop Med Surg. 1989;10:335-337.
- Hijikata S, Yamagishi M, Nakayama T, Oomori K. Percutaneous nucleotomy: a treatment method for lumbar disk herniation. J Toden Hosp. 1975;5:39.
- Manchikanti L, Abdi S, Atluri S, Balog CC, Benyamin RM, Boswell MV, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2 – Guidance. Pain Physician. 2012 Jul;15(suppl 6):S67-S116. [PubMed]
- Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long term outcomes of standard discectomy for lumbar disc herniation: a follow up study of more than 10 years. Spine (Phila Pa 1976). 2001 Mar;26(6):652–7.[PubMed]
- Manchikanti L, Pampati V, Falco FJ, Hirsch JA. Growth of spinal interventional pain management techniques: analysis of utilization trends and Medicare expenditures 2000 to 2008. Spine (Phila Pa 1976). 2013 Jan 15;38(2):157-168. doi: 10.1097/BRS.0b013e318267f463. [PubMed]
- Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000 Jan;84(1):95-103. [PubMed]
- Onik G, Helms C, Ginsburg L, Hoaglund FT, Morris J. Percutaneous lumbar diskectomy using a new aspiration probe. AJR Am J Roentgenol, 1985;144(6):1137-40. [PubMed]
- Bonaldi G. Automated percutaneous lumbar discectomy: Technique, indications, and clinical follow-up in over 1,000 patients. Neuroradiology 2003;45:735-743. [PubMed]
- Gill K, Blumenthal SL. Automated percutaneous discectomy. Long-term clinical experience with the Nucleotome system. Acta Orthop Scand Suppl 1993;251:30-33. [PubMed]
- Chatterjee S, Foy PM, Findlay GF. Report of a controlled clinical trial comparing automated percutaneous lumbar discectomy and microdiscectomy in the treatment of contained lumbar disc herniation. Spine (Phila Pa 1976). 1995 Mar 15;20(6):734-738. [PubMed]
- Haines SJ, Jordan N, Boen JR, Nyman JA, Oldridge NB, Lindgren BR; LAPDOG/ LEAPDOG Investigators. Discectomy strategies for lumbar disc herniation: Results of the LAPDOG trial. J Clin Neurosci. 2002 Jul;9(4):411-417. [PubMed]
- Teng GJ, Jeffery RF, Guo JH, He SC, Zhu HZ, Wang XH, et al. Automated percutaneous lumbar discectomy: A prospective multi-institutional study. J Vasc Interv Radiol. 1997 May-Jun;8(3):457-463. [PubMed]
- Grevitt MP, McLaren A, Shackleford IM, Mulholland RC. Automated percutaneous lumbar discectomy. An outcome study. J Bone Joint Surg Br. 1995 Jul;77(4):626- 629. [PubMed]
- Bernd L, Schiltenwolf M, Mau H, Schindele S. No indications for percutaneous lumbar discectomy? Int Orthop. 1997;21(3):164-168. [PubMed] [Free full text]
- Marks RA. Transcutaneous lumbar diskectomy for internal disk derangement: A new indication. South Med J. 2000 Sep;93(9):885-890. [PubMed]
- Gebhard JS, Brugman JL. Percutaneous discectomy for the treatment of bacterial discitis. Spine (Phila Pa 1976). 1994 Apr 1;19(7):855-857. [PubMed]
- Fouquet B, Goupille P, Jattiot F, Cotty P, Lapierre F, Valat JP, et al. Discitis after lumbar disc surgery: features of aseptic and septic forms. Spine. 1992 Mar;17(3):356-358. [PubMed]