Anastasios Petrou, MD, PhD*1, Petros Tzimas, MD, PhD1, Georgios Papadopoulos, Dr, Med Habil2
1Assistant professor; 2Professor
Department of Anesthesiology and Postoperative Intensive Care, Faculty of Medicine, School of Health Sciences, University of Ioannina, P.O. Box 1186, 45110, Ioannina, (Greece)
Correspondence: Anastasios Petrou, MD, PhD, Department of Anesthesiology and Postoperative Intensive Care, Faculty of Medicine, School of Health Sciences, University of Ioannina, P.O. Box 1186, 45110, Ioannina, (Greece); Tel: +306972728149; Fax: +302651007887; E-mail: apetrou@cc.uoi.gr
ABSTRACT
Neuropathic pain is a common cause of chronic pelvic pain. Its resistance to treatment, often challenges patient’s cooperation to prolonged and sometimes interventional schemes and necessitates constant search for alternative or complementary interventions.
In this case series, one elderly male patient who presented with persistent chronic pelvic pain after multiple abdominal operations did not respond to conventional medical treatment and acupuncture and requested discontinuation of treatment. Electro-acupuncture was applied as a last resort therapy and proved very effective in reducing pelvic pain; it permitted significant reduction in anti-depressant medication doses. A second case study refers to a young female patient who developed chronic pelvic pain after giving birth to a child. Various treatments proved unsuccessful in alleviation her pain. She eventually responded to electro-acupuncture at multiple trigger points in the abdominal wall.
Key words: Pain; Chronic pelvic pain; Electro-acupuncture; Adult
Citation: Petrou A, Tzimas P, Papadopoulos G. Electro-acupuncture for chronic pelvic pain; two interesting cases. Anaesth Pain & Intensive Care 2016;20(4):484-487
Received: 28 Nov 2016; Reviewed: 6 Dec 2016; Corrected: 7 Dec 2016; Accepted: 10 Dec 2016
INTRODUCTION
Chronic pelvic pain (CPP) is a benign pain syndrome of continuous or relapsing pain that derives from the pelvic cavity and persists for more than six months. Its association with intercourse or menstruation is possible but not causative. It affects approximately one in seven women and in some studies comprises almost 10% of all referrals to gynecologists.1,2
Various diseases generate CPP, which has multiple clinical manifestations but an obscure etiology.3,4
The clinical approach is based upon detailed patient history, meticulous physical examination and appropriate laboratory evaluation. Treatment interventions are phased, starting with less invasive methods and escalating to more aggressive techniques, according to well established algorithms.5
We present two cases of complicated CPP which recently presented to our pain clinic and were successfully treated.
CASE REPORT 1
An 80 years old male patient presented with severe pelvic pain His surgical patient history included a trans-urethral prostate resection 6 months prior to his visit with subsequent diagnosis of prostate cancer (clinical stage T1a-N0-M0 at presentation). He was on gonadotropin-releasing hormone agonists and non-steroid anti-androgens. A few years ago, he had a partial hepatectomy for liver cancer, endoscopic large bowel polyps resection and an inguinal hernia repair. His medical history was significant for arterial hypertension, coronary artery disease and an abdominal aortic aneurysm managed medically.
His analgesia included paracetamol 1 g thrice daily orally and tramadol drops 400 mg once daily orally.
The patient had severe pelvic and back pain, rated at 10 out of 10 on Numeric Rating Scale (NRS, calibrated as 0 = no pain, 10 = worst imaginable pain) and episodes of caustic pain originating from the outer urethral meatus and referred to the lower hypogastrium and the lumbar region (Figure 1).
Figure 1: Pencil sketches localizing pain (shaded areas) of both of the patients
Quality of life was graded as 3 out of 8 using the Instrumental Activities of Daily Life scale (IADL). The patient was clearly on a moderate depression state grade 20 on Beck Depression Inventory scale [(BDI-II), 0-13: minimal, 14-19: mild, 20-28: moderate, 29-63: severe].
Acupuncture was begun using acupoints BL 31+, BL 32+, BL 33+, BL 34+, SP 6, KI 3, CV 6, GB 28+, ST 29+, CV 4 (for pelvic inflammation and pain) plus BL 23+, CV 2, CV 4, BL 40, KI 5, KI 7 (for the urinary bladder pain) with 0.25 X 25 mm needles without tonification or dispersion (Figure 2
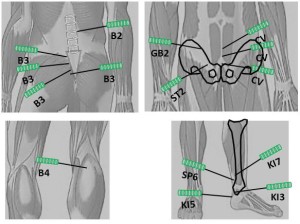
Figure 2: Acupoints used in patient No. 1
The intervention lasted 30 min but failed to alleviate pain and the patient denied further sessions. A per os regimen of venlafaxine (a selective serotonin and norepinephrine reuptake inhibitor) 37.5 mg twice daily, titrated to 75 mg twice daily, pregabalin 75 mg once daily, titrated to 300 mg twice daily and tramadol/acetaminophen 2 x (37.5 mg + 325 mg) four times daily decreased pain by approximately 50% but offered no relief of the urethral pain. The patient was bedridden, disheveled, dizzy, and somnolent and requested discontinuation of medical treatment. After extensive discussion with the pain team, he consented for a series of electro-acupuncture sessions as a last resort option accompanied by tapering of medications to the lowest indicated doses.
Electro-acupuncture was administered sequentially at the same acupoints as in the initial trial (6 mA, 2 Hz, 220 ms, Pointer Excel II, TENS PLUS IND.CO. Hong Kong). The point stimulation was applied for 30-60 sec and the session lasted more than 90 min. The patient exhibited immediate and complete regression of pain at the pelvis and the lumbar region and significant relief of the urethral meatus pain by the first session. After 8 weekly electro-acupuncture sessions he was free of pain in the pelvis and the lumbar region but still had recurring micturition pain (NRS 3). He discontinued tramadol, acetaminophen and pregabalin, reduced his venlafaxine dose, started socializing out of the home; his depression fading and his appearance was decent again.
At follow up at 72 months later he was happy and only complained about micturition pain (VAS 3).
CASE REPORT 2
A young (38 years old) woman 18 months after giving birth to her second child, developed a temporally increasing pain in the pelvis, lumbar back and left thigh (Figure 1). Subsequently diagnosed with endometriosis, she was treated with endoscopic ablation combined with excision of an ovary cyst, but the pain was worsened after the operation. Then, the patient received medical treatment for suspected irritable bowel syndrome, but it failed to relieve her pain symptoms.
At presentation she had a painful facial expression and a left, forward bending of the torso, like protecting the left pelvic area. She complained of devastating pain (NRS 10) at the left hypogastrium, referred to the inner surface of the left thigh, the left labium majus and the left lower lumbar region and lower bowel distension. The pain was constant during the day and was aggravating during the night, preventing sleep in either supine or prone positions. She also reported a burning pain in her inner, left thigh.
At physical examination, the hypogastrium was very sensitive and painful. Palpation of the left rectus abdominis muscle below the umbilicus as well the left lateral margin of the hypogastrium (external oblique muscle) with a balsam oil lubricated thumb revealed multiple pin point nodes that triggered very intense pain and averted reporting of its radiation.
The application of 30-60 second sequential electro-acupuncture (6 mA, 2 Hz, 220 ms, AS Super4, Pointer Excel II, TENS PLUS IND.CO. Hong Kong) at more than 30 identified trigger points resulted in complete reversal of spontaneous and palpation induced pain. The sense of abdominal distention disappeared and the patient could sleep peacefully in any desired posture. The electro-acupuncture scheme was repeated at 12 and 24 hours and the patient was started on venlafaxine that was escalated up to 75 mg twice daily during the following weeks. Three months later, venlafaxine was reduced gradually and was discontinued six months after the electro-acupuncture session.
Two years later, the patient has no pain and does not receive medical treatment.
DISCUSSION
We reported two diverse cases of CPP - one had classic neuropathic pain (NP) and was resistant to medical treatment and the other had myofascial syndrome of the abdominal wall muscles; both were treated with electro-acupuncture. The intervention was judged successful with long standing effects.
Chronic pelvic pain is a quite common, multifactorial clinical entity. Aside from gynecologic origin in women, it is important for the clinician to seek for other possible causes including NP and neuromuscular pelvic system disorders.
Acupuncture was proposed by World Health Organization (WHO) in 1982 as a potential treatment for NP.6 In our case, we chose a standardized protocol that is considered appropriate for CPP and is potentially equally effective to personalized approaches.7,8
Acupuncture and electro-acupuncture convey their analgesic effect through release of endogenous endorphins, encephalins, dynorphins, prostaglandins, serotonin and ACTH at the central nervous system. Activation of the autonomous sympathetic system and the gate mechanism at the substantia gelatinosa is thought to cancel propagation of painful stimuli to the sensory cortex.9,10 The success of electro-acupuncture trial (case 1), despite the failure of acupuncture six months earlier, could be attributed to the re-balancing of chi and the facilitating effect of the anti-epileptic and anti-depressant medications. Quality of life improvement can also be credited to both anti-depressant medications and the resolution of persistent pain.
The outcome of case 2 reveals the significance of painful points on the rectus abdominis and external oblique muscles as important triggers of CPP.11-13
Myofascial syndrome are actually a subset of neuropathic pain and refers to a regional, neuromuscular disorder with particular neurophysiologic origins and distinct diagnostic criteria.14,15 It predominantly affects women of any age.1 Muscle trigger points evolve in superficial and deep pelvic muscle groups during high energy demand (e.g., strenuous and protracted training, bad sitting or standing posture) that results in defective blood supply in certain muscle foci, disruption of sarcoplasmic reticulum and spillover of algogenic substances. Referred pain from trigger points can sometimes be misleading as it can arise even in the contralateral side of the abdomen or in quite distant areas of the body.15
Therapeutic interventions focus on the de-activation of trigger points. Medical treatment consists of weak analgesics, muscle relaxants, anti-inflammatory preparations in combination with physiotherapy, local anesthetic infiltrations, dry needling or ultrasonic treatment16 and non-interventional options like TENS, laser and repetitive magnetic stimulation (rMS).16,17 Chronic cases can be benefitted by anti-depressants and botulin toxin.13
CONCLUSION
In our cases, electro-acupuncture proved effective in successfully suppressing both CPP cases. Clinicians should persistently urge to deliver effective treatments based on scientific evidence and judicious consideration. Further research is needed to confirm if electro-acupuncture can be a reasonable option for neuropathic CPP treatment.
Conflict of interest: No author has any competing interest with the material presented in the manuscript.
Authors’ contributions:
AP & PT: literature search, drafting, review and final preparation of manuscript.
GP: literature search, drafting and final review of manuscript.
REFERENCES
1Assistant professor; 2Professor
Department of Anesthesiology and Postoperative Intensive Care, Faculty of Medicine, School of Health Sciences, University of Ioannina, P.O. Box 1186, 45110, Ioannina, (Greece)
Correspondence: Anastasios Petrou, MD, PhD, Department of Anesthesiology and Postoperative Intensive Care, Faculty of Medicine, School of Health Sciences, University of Ioannina, P.O. Box 1186, 45110, Ioannina, (Greece); Tel: +306972728149; Fax: +302651007887; E-mail: apetrou@cc.uoi.gr
ABSTRACT
Neuropathic pain is a common cause of chronic pelvic pain. Its resistance to treatment, often challenges patient’s cooperation to prolonged and sometimes interventional schemes and necessitates constant search for alternative or complementary interventions.
In this case series, one elderly male patient who presented with persistent chronic pelvic pain after multiple abdominal operations did not respond to conventional medical treatment and acupuncture and requested discontinuation of treatment. Electro-acupuncture was applied as a last resort therapy and proved very effective in reducing pelvic pain; it permitted significant reduction in anti-depressant medication doses. A second case study refers to a young female patient who developed chronic pelvic pain after giving birth to a child. Various treatments proved unsuccessful in alleviation her pain. She eventually responded to electro-acupuncture at multiple trigger points in the abdominal wall.
Key words: Pain; Chronic pelvic pain; Electro-acupuncture; Adult
Citation: Petrou A, Tzimas P, Papadopoulos G. Electro-acupuncture for chronic pelvic pain; two interesting cases. Anaesth Pain & Intensive Care 2016;20(4):484-487
Received: 28 Nov 2016; Reviewed: 6 Dec 2016; Corrected: 7 Dec 2016; Accepted: 10 Dec 2016
INTRODUCTION
Chronic pelvic pain (CPP) is a benign pain syndrome of continuous or relapsing pain that derives from the pelvic cavity and persists for more than six months. Its association with intercourse or menstruation is possible but not causative. It affects approximately one in seven women and in some studies comprises almost 10% of all referrals to gynecologists.1,2
Various diseases generate CPP, which has multiple clinical manifestations but an obscure etiology.3,4
The clinical approach is based upon detailed patient history, meticulous physical examination and appropriate laboratory evaluation. Treatment interventions are phased, starting with less invasive methods and escalating to more aggressive techniques, according to well established algorithms.5
We present two cases of complicated CPP which recently presented to our pain clinic and were successfully treated.
CASE REPORT 1
An 80 years old male patient presented with severe pelvic pain His surgical patient history included a trans-urethral prostate resection 6 months prior to his visit with subsequent diagnosis of prostate cancer (clinical stage T1a-N0-M0 at presentation). He was on gonadotropin-releasing hormone agonists and non-steroid anti-androgens. A few years ago, he had a partial hepatectomy for liver cancer, endoscopic large bowel polyps resection and an inguinal hernia repair. His medical history was significant for arterial hypertension, coronary artery disease and an abdominal aortic aneurysm managed medically.
His analgesia included paracetamol 1 g thrice daily orally and tramadol drops 400 mg once daily orally.
The patient had severe pelvic and back pain, rated at 10 out of 10 on Numeric Rating Scale (NRS, calibrated as 0 = no pain, 10 = worst imaginable pain) and episodes of caustic pain originating from the outer urethral meatus and referred to the lower hypogastrium and the lumbar region (Figure 1).
Figure 1: Pencil sketches localizing pain (shaded areas) of both of the patients
Quality of life was graded as 3 out of 8 using the Instrumental Activities of Daily Life scale (IADL). The patient was clearly on a moderate depression state grade 20 on Beck Depression Inventory scale [(BDI-II), 0-13: minimal, 14-19: mild, 20-28: moderate, 29-63: severe].
Acupuncture was begun using acupoints BL 31+, BL 32+, BL 33+, BL 34+, SP 6, KI 3, CV 6, GB 28+, ST 29+, CV 4 (for pelvic inflammation and pain) plus BL 23+, CV 2, CV 4, BL 40, KI 5, KI 7 (for the urinary bladder pain) with 0.25 X 25 mm needles without tonification or dispersion (Figure 2
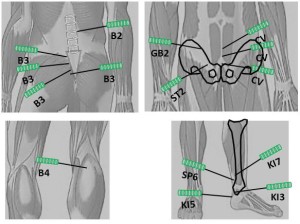
Figure 2: Acupoints used in patient No. 1
The intervention lasted 30 min but failed to alleviate pain and the patient denied further sessions. A per os regimen of venlafaxine (a selective serotonin and norepinephrine reuptake inhibitor) 37.5 mg twice daily, titrated to 75 mg twice daily, pregabalin 75 mg once daily, titrated to 300 mg twice daily and tramadol/acetaminophen 2 x (37.5 mg + 325 mg) four times daily decreased pain by approximately 50% but offered no relief of the urethral pain. The patient was bedridden, disheveled, dizzy, and somnolent and requested discontinuation of medical treatment. After extensive discussion with the pain team, he consented for a series of electro-acupuncture sessions as a last resort option accompanied by tapering of medications to the lowest indicated doses.
Electro-acupuncture was administered sequentially at the same acupoints as in the initial trial (6 mA, 2 Hz, 220 ms, Pointer Excel II, TENS PLUS IND.CO. Hong Kong). The point stimulation was applied for 30-60 sec and the session lasted more than 90 min. The patient exhibited immediate and complete regression of pain at the pelvis and the lumbar region and significant relief of the urethral meatus pain by the first session. After 8 weekly electro-acupuncture sessions he was free of pain in the pelvis and the lumbar region but still had recurring micturition pain (NRS 3). He discontinued tramadol, acetaminophen and pregabalin, reduced his venlafaxine dose, started socializing out of the home; his depression fading and his appearance was decent again.
At follow up at 72 months later he was happy and only complained about micturition pain (VAS 3).
CASE REPORT 2
A young (38 years old) woman 18 months after giving birth to her second child, developed a temporally increasing pain in the pelvis, lumbar back and left thigh (Figure 1). Subsequently diagnosed with endometriosis, she was treated with endoscopic ablation combined with excision of an ovary cyst, but the pain was worsened after the operation. Then, the patient received medical treatment for suspected irritable bowel syndrome, but it failed to relieve her pain symptoms.
At presentation she had a painful facial expression and a left, forward bending of the torso, like protecting the left pelvic area. She complained of devastating pain (NRS 10) at the left hypogastrium, referred to the inner surface of the left thigh, the left labium majus and the left lower lumbar region and lower bowel distension. The pain was constant during the day and was aggravating during the night, preventing sleep in either supine or prone positions. She also reported a burning pain in her inner, left thigh.
At physical examination, the hypogastrium was very sensitive and painful. Palpation of the left rectus abdominis muscle below the umbilicus as well the left lateral margin of the hypogastrium (external oblique muscle) with a balsam oil lubricated thumb revealed multiple pin point nodes that triggered very intense pain and averted reporting of its radiation.
The application of 30-60 second sequential electro-acupuncture (6 mA, 2 Hz, 220 ms, AS Super4, Pointer Excel II, TENS PLUS IND.CO. Hong Kong) at more than 30 identified trigger points resulted in complete reversal of spontaneous and palpation induced pain. The sense of abdominal distention disappeared and the patient could sleep peacefully in any desired posture. The electro-acupuncture scheme was repeated at 12 and 24 hours and the patient was started on venlafaxine that was escalated up to 75 mg twice daily during the following weeks. Three months later, venlafaxine was reduced gradually and was discontinued six months after the electro-acupuncture session.
Two years later, the patient has no pain and does not receive medical treatment.
DISCUSSION
We reported two diverse cases of CPP - one had classic neuropathic pain (NP) and was resistant to medical treatment and the other had myofascial syndrome of the abdominal wall muscles; both were treated with electro-acupuncture. The intervention was judged successful with long standing effects.
Chronic pelvic pain is a quite common, multifactorial clinical entity. Aside from gynecologic origin in women, it is important for the clinician to seek for other possible causes including NP and neuromuscular pelvic system disorders.
Acupuncture was proposed by World Health Organization (WHO) in 1982 as a potential treatment for NP.6 In our case, we chose a standardized protocol that is considered appropriate for CPP and is potentially equally effective to personalized approaches.7,8
Acupuncture and electro-acupuncture convey their analgesic effect through release of endogenous endorphins, encephalins, dynorphins, prostaglandins, serotonin and ACTH at the central nervous system. Activation of the autonomous sympathetic system and the gate mechanism at the substantia gelatinosa is thought to cancel propagation of painful stimuli to the sensory cortex.9,10 The success of electro-acupuncture trial (case 1), despite the failure of acupuncture six months earlier, could be attributed to the re-balancing of chi and the facilitating effect of the anti-epileptic and anti-depressant medications. Quality of life improvement can also be credited to both anti-depressant medications and the resolution of persistent pain.
The outcome of case 2 reveals the significance of painful points on the rectus abdominis and external oblique muscles as important triggers of CPP.11-13
Myofascial syndrome are actually a subset of neuropathic pain and refers to a regional, neuromuscular disorder with particular neurophysiologic origins and distinct diagnostic criteria.14,15 It predominantly affects women of any age.1 Muscle trigger points evolve in superficial and deep pelvic muscle groups during high energy demand (e.g., strenuous and protracted training, bad sitting or standing posture) that results in defective blood supply in certain muscle foci, disruption of sarcoplasmic reticulum and spillover of algogenic substances. Referred pain from trigger points can sometimes be misleading as it can arise even in the contralateral side of the abdomen or in quite distant areas of the body.15
Therapeutic interventions focus on the de-activation of trigger points. Medical treatment consists of weak analgesics, muscle relaxants, anti-inflammatory preparations in combination with physiotherapy, local anesthetic infiltrations, dry needling or ultrasonic treatment16 and non-interventional options like TENS, laser and repetitive magnetic stimulation (rMS).16,17 Chronic cases can be benefitted by anti-depressants and botulin toxin.13
CONCLUSION
In our cases, electro-acupuncture proved effective in successfully suppressing both CPP cases. Clinicians should persistently urge to deliver effective treatments based on scientific evidence and judicious consideration. Further research is needed to confirm if electro-acupuncture can be a reasonable option for neuropathic CPP treatment.
Conflict of interest: No author has any competing interest with the material presented in the manuscript.
Authors’ contributions:
AP & PT: literature search, drafting, review and final preparation of manuscript.
GP: literature search, drafting and final review of manuscript.
REFERENCES
- Mathias SD, Kuppermann M, Liberman RF, Lipschutz RC, Steege JF. Chronic pelvic pain: prevalence, health-related quality of life, and economic correlates. Obstet Gynecol. 1996 Mar;87(3):321-7. [PubMed]
- Reiter RC. A profile of women with chronic pelvic pain. Clin Obstet Gynecol. 1990 Mar;33(1):130-6. [PubMed]
- Anothaisintawee T, Attia J, Nickel JC, Thammakraisorn S, Numthavaj P, McEvoy M, et al. Management of chronic prostatitis/ chronic pelvic pain syndrome: a systematic review and network meta-analysis. JAMA. 2011;305(1):78-86. doi: 10.1001/jama.2010.1913. [PubMed] [Free full text]
- Latthe P, Mignini L, Gray R, Hills R, Khan K. Factors predisposing women to chronic pelvic pain: systematic review. BMJ. 2006;332(7544):749-55. [PubMed] [Free full text]
- Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010 Jan;57(1):35-48. doi: 10.1016/j.eururo.2009.08.020 [PubMed]
- Lin J-G, Chen W-L. Acupuncture analgesia: a review of its mechanisms of actions. Am J Chin Med. 2008;36(4):635-45. [PubMed]
- Zhao ZQ. Neural mechanism underlying acupuncture analgesia. Prog Neurobiol. 2008; 85(4): p. 355-375. doi: 10.1016/j.pneurobio.2008.05.004. [PubMed]
- Zhang X. Acupuncture: Review and analysis of reports on controlled clinical trials. WHO, (EDM) DoEDaMP; 2003. p. 1-81. [Free full text]
- Richards D. Simple Health Maintenance. 2nd ed. St Georges, SA: Superior Health Products PTY Ltd; 1991. p. 172.
- Lathia AT, Jung SM, Chen LX. Efficacy of acupuncture as a treatment for chronic shoulder pain. J Altern Complement Med. 2009 Jun;15(6):613-8. doi: 10.1089/acm.2008.0272. [PubMed]
- Benjamin-Pratt A, Howard F. Management of chronic pelvic pain. Minerva Ginecol. 2010;62(5):447-65. [PubMed]
- Tu FF, As-Sanie S, Steege JF. Musculoskeletal causes of chronic pelvic pain: a systematic review of diagnosis: part I. Obstet Gynecol Surv. 2005 Jun;60(6):379-85. [PubMed]
- Jarrell JF, Vilos GA, Allaire C, Burgess S, Fortin C, Gerwin R, et al. Consensus guidelines for the management of chronic pelvic pain. J Obstet Gynaecol Can. 2005;27(9):869-910. [PubMed]
- Task Force on Taxonomy of the International Association for the Study of Pain. Classification of chronic pain, descriptions of chronic pain syndromes and definitions of pain terms. . 2nd ed. Merskey HD, Bogduk N, editors. Seattle: IASP Press; 2002. [Free full text]
- Gerwin RD. Classification, epidemiology, and natural history of myofascial pain syndrome. Curr Pain Headache Rep. 2001. 5(5):412-20. [PubMed]
- Papadopoulos G, Liarmakopoulou A. The myofascial syndrome. 1st ed. Ioannina, Hellas: EFYRA; 2008. p: 4-111
- FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, et al. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. J Urol. 2012 Jun;187(6):2113-8. doi: 10.1016/j.juro.2012.01.123. [PubMed