Cobra Ghasemi1, Ali Amiri2, Javad Sarrafzadeh3, Mehdi Dadgoo2, Nader Maroufi3
1- PhD (Physiotherapy), Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
2- Assistant Professor, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
3- Associate Professor, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
*Correspondence: Ali Amiri, Assistant Professor, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran; E-mail: aliamiri12@protonmail.com; Phone: +989123658547
Abstract
Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
Keywords: Low Back Pain; Craniosacral Therapy; Muscle Energy Technique; Sensorimotor Training
Abbreviations: CST - Craniosacral therapy; MET - Muscle energy technique; SMT - Sensorimotor training; NCLBP - Non-specific chronic low back pain; ODQ - Oswestry functional disability questionnaire; 36-SF - 36-item short form health survey; BDI - Beck depression inventory; ROM - Range of motion
Citation: Ghasemi C, Amiri A, Sarrafzadeh J, Dadgoo M, Maroufi N. Comparison of the effects of craniosacral therapy, muscle energy technique, and sensorimotor training on non-specific chronic low back pain. Anaesth. pain intensive care 2020;24(5):532-543
Received: 21 July 2020, Reviewed: 14 August 2020, Revised: 15 August 2020, Accepted: 15 August 2020
DOI: https://doi.org/10.35975/apic.v24i5.1362
Introduction
Non-specific chronic low back pain (NCLBP) is a low back pain which is not attributable to a distinguishable, recognized certain pathology.1 Low back pain is estimated to be one of the important reasons of disability adjusted life years (DALYs).2 Non-specific Chronic low back pain (NCLBP) is a common problem.1 The lifetime occurrence of low back pain is informed to be 84%, and the frequency of chronic low back pain is around 23%, and about 11-12% of the people being disabled by low back pain.1 NCLBP is the most prevalent form of low back pain. NCLBP is mostly common at the age of 35 to 55 y.3 Hence, low back pain has a severe influence on the workforce and lead to a significant socioeconomic effects.3
Muscle Energy Technique (MET) is a multipurpose method conventionally used to address muscular tension, pain, and joint dysfunction and to develop range of motion (ROM).4 MET is a method in that the patient supplies the curative force, rather than the care giver.5 It was shown that MET is effective in decreasing lumbopelvic pain,6 decreasing disability in acute LBP,7 and Improving lumbar and cervical ROM in asymptomatic people.8 Recently, it is shown that MET is effective in the treatment of LBP, nevertheless it requires to be compared with other manual therapy methods.9
Craniosacral therapy (CST) is an alternative and complementary therapy which claimed to release the tension of the muscles, ligaments, and fascia in the sacral area.10 CST seems activate central pain inhibitory centers.11 CST is suggested for all musculoskeletal conditions particularly back pain 10, 11. It was shown that CST has effect on non-specific chronic low back pain,12 pelvic pain,13 chronic neck pain,14 and acute lower back pain.15
Recent research has indicated that proprioceptive sense is related to back pain and these individuals have weaker proprioceptive sense.16 It is demonstrated that Sensorimotor Training (SMT) can improve the proprioceptive sense. Studies have shown the effect of SMT on chronic low back pain control.17-19
NCLBP has become of the main public health issues throughout the world.1 The prevalence of chronic NCLBP is considerable and a percentage of the population being disabled by it 1. Also, it has a severe effect on the workforce and cause a significant socioeconomic effects3 Therefore, finding an effective method for treatment is important. Craniosacral therapy as a soft tissue manipulation leading to increased parasympathetic activity, which provides comfort and facilitation and cognitive processes.20 It removes pressure patterns which regulating the cycle of the brain, rhythm of the craniosacral, and accelerating the circulation of the CSF,21 thereby affecting the entire body. CST decreases the muscle tone and causes relaxation and mood improvement in individuals.22 Therefore, the hypothesis of this study is that whether CST has more effect on NCLBP rather than met and Smt. although there are studies that evaluated the effect of MET, SMT, or CST methods on NCLBP patients, no study compared the effect of these three methods on NCLBP. The aim of the present study is to assess the effectiveness of MET, CST, and CST on pain control, disability, depression, and quality of life of patients with NCLBP.
Methodology
In this randomized clinical trial (IRCT20170117032020N3) study 45 patients with NCLBP who referred to physiotherapy clinic of School of Rehabilitation of Iran University of Medical Sciences from September 2016 until November 2017 were participated. The sampling method was non-random. The number of samples was calculated through G-Power software and based on the studies of Volpe et al.23 and Salavati et al.24 and the following sample size was obtained:
In this study, α (probability of error of the first type) is equal to 0.05 and β (probability of error of the second type) is equal to 80%, based on which the effect size = 1. Therefore, currently the number of people studied in each of the 3 groups of 15 people is considered.
The NCLBP were defined as a localized pain in the lumbar region (from the twelfth rib to the gluteal fold) for 3 months continuously or repeatedly for more than six months and with an intensity of less than 6 to at least 3 based on the visual scale of the pain and it is defined by a specialist. The inclusion criteria were having low back pain below the costal margin and above inferior gluteal folds and suffering from low back pain (LBP) for more than 6 months; having the age range of 20 to 40 y old, and the disability level of more than 14% and less than 50% according to Oswestry questionnaire; and the exclusion criteria were pregnancy, history of neurologic disorder, infection, seizure, inflammatory diseases, tumor, lumbar fracture, and lumbar surgery. The eligible subjects were randomly divided in three groups including CST (n =15), SMT (n = 15), and MET (n = 15). Patients were matched for age, sex and body mass index in all groups. The study was approved by ethical committee of Iran University of Medical Sciences (IR.IUMS.REC139509211342216). Written consent was obtained from all participants. The interventions were performed as follow in 3 groups:
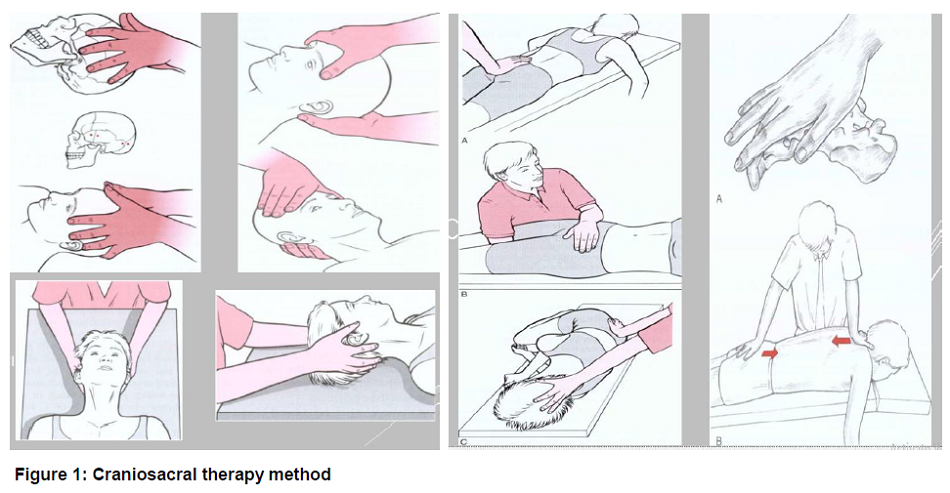
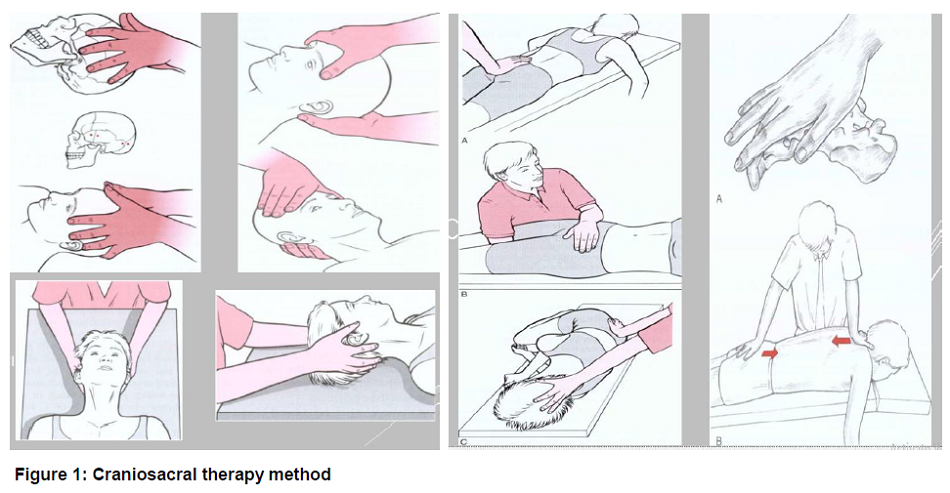
An experienced craniosacral therapist carried out the CST. Modified therapeutic protocol by Upledger and Vredevoogd was used for CST.25 Patients received 10 session of CST in 5 weeks (2 sessions per week) and each session lasts 45 minutes. A session contains 4 phases including in prone position, in side-lying position behind the therapist, in side-lying in front of the therapist, and in supine position (Figure 1); Patients were in each position for 10 minutes. To feel and follow craniosacral movements, craniosacral therapist put her both hands on two regions or bones.25
In MET group 10 sessions of muscle energy technique in 5 weeks (2 sessions per week) 26 were performed for treatment of posterior rotation of the right or left innominate (to restore anterior rotation) and anterior rotation of the right or left innominate (to restore posterior rotation) dysfunctions (with regard to the side of the dysfunction) which were done 3-5 times per session with 5-10 sec time of hold for each position, and correction of a sacroiliac joint up slip which was done 12 times each session27 (Figure 2). Dysfunctions were determined using the following tests: Standing flexion test, Gillet test or Stork test (sacral fixation test), supine to sit test, and sitting flexion test.
In SMT group, patients received 10 sessions of balance training in 5 weeks (2 sessions per week) based on global approach by Page (2006). According to this approach, patients’ progress evaluated through three stages of static, dynamic, and functional during 10 sessions.28 In each stage, patients experience different postures and base of support and their center of gravity is being challenged (Figure 3). To determine the pain intensity a 10 cm visual analogue scale (VAS) was used. VAS contains 0 to 10 degree which 0 represents “no pain” and 10 represent “worst imaginable pain”. This scale is a reliable and valid measurement tool for pain assessment in NCLBP.29 Participants were asked to score their pain at the test time.
The Persian version of Oswestry functional disability questionnaire (ODQ) was used to assess the functional disability of patients (16). ODQ includes 10 items, each scored from 0 to 5 and the highest score is 50 which should be doubled to show the percentage. The higher Oswestry disability index (ODI) scores shows the higher level of disability. According to the Baradaran et al. study, Infraclass correlation coefficient (ICC) for each item ranged from 0.43 to 0.80 that shows a good reliability and reproducibility of each item. Cronbach's α coefficient was 0.69 that shows a good internal consistency for Persian version of ODQ.30
To evaluate the depression in patients the Beck depression inventory-II (BDI-II) was used. BDI-II contains 21 questions. Each question has 4 sentences describing the patient’s situation. BDI-II score ranges from 0 to 63 and the higher scores designates the higher level of depression.31 Ghassemzadeh et al. showed that the BDI-II Persian version had high internal consistency (Cronbach’s α = 0.87) and acceptable test-retest reliability (r = 0.74).32
The Persian version of 36-item short form health survey (SF-36) was used to measure the quality of life of patients.33 This questionnaire has 8 domains including physical function, body pain, social functioning, general health, role physical, vitality, role emotional and mental health. Each domain is scored from 0 to 100 scale that the higher scores specify the better health condition. Montazeri et al. revealed that the internal consistency for all eight SF-36 scales met the minimum reliability standard, the Cronbach's alpha coefficients was ranged from 0.77 to 0.90 except for the vitality scale that was 0.65.33
Patients were asked to report the VAS score and fill the ODQ, BDI-II, and SF-36 questioners before the treatment, after the last session of treatment, and after 2 months follow up.
SPSS version 16 was used to analyze the data. ANOVA and Tukey post hoc tests used to compare the data. Repeated measures of analysis of variance (ANOVA, Wilks' Lambda test) was used to assess the effects of group, time and their interaction for VAS,
In MET group 10 sessions of muscle energy technique in 5 weeks (2 sessions per week)26 were performed for treatment of posterior rotation of the right or left innominate (to restore anterior rotation) and anterior rotation of the right or left innominate (to restore posterior rotation) dysfunctions (with regard to the side of the dysfunction) which were done 3-5 times per


ODI, BDI-II and SF-36. Values were significant at p < 0.001. Flowchart of study is shown in Figure 4.
Results
The results of repeated measure of ANOVA test showed that VAS changes were significant at all 3 times in each of the SMT, CST and MET groups (p < 0.001, p < 0.001, and p < 0.001). The result of the ANOVA test showed that the VAS variable in the baseline time was not significantly different between the groups, but in after treatment and post-follow up, there was a significant difference (p = 0.137, p < 0.001, p < 0.001). The result of the Tukey's post hoc test showed that VAS changes in post-treatment and follow-up time in the CST group were significantly different in

Table 1: Comparing VAS scores at Base time, Post-treatment and in follow-up time with the results of repeated measures of ANOVA (Mean ± SD)
* Significant differences compared to SMT group, # significant differences compared to CST group, P01: Comparison of Post-treatment with base time, P02: Comparison of follow up with base time, P12: Comparison of Follow up by Post-treatment




that ODI changes in post-treatment and follow-up time in the CST group were significantly different in comparison to SMT group, and the changes in ODI at after treatment and follow-up times in the CST group compared with the MET group had a significant difference (Table 2; Figure 2). The results of repeated measure of ANOVA test showed that BDI changes were significant at 3 readings in each of the SMT, CST and MET groups (p < 0.001, p < 0.001, p < 0.001). The result of the ANOVA test showed that the BDI variable in the baseline time was not significantly different between 3 groups, but in after treatment and post-follow up, there was a significant difference (p = 0.579, p <0.001, p <0.001). The result of the Tukey's post hoc test showed that BDI changes in post-treatment and follow-up time in the CST group were significantly different in comparison to SMT group, and the changes in BDI at after treatment and follow-up times in the CST group compared with the MET group had a significant difference (Table 3; Figure 3). The results of repeated measure of ANOVA test showed that SF-36 changes were significant at 3 readings in each of the SMT, CST and MET groups (p < 0.001, p < 0.001, p < 0.001). The result of the ANOVA test showed that the SF-36 variable in the baseline time was not significantly different between 3 groups, but after treatment and post-follow up, there was a significant difference (p = 0.707, p < 0.001, p < 0.001). The result of the Tukey's post hoc test showed that BDI changes in post-treatment and follow-up time in the CST group were significantly different in comparison to SMT group, and the changes in SF-36 at after treatment and follow-up times in the CST group compared with the group MET had a significant difference (Table 4; Figure 4).
.
* Significant differences compared to SMT group, # significant differences compared to CST group, P01: Comparison of Post-treatment with base time, P02: Comparison of follow up with base time, P12: Comparison of Follow up by Post-treatment
Table 4: Comparing SF-36 scores at base time, post-treatment and in follow-up time with the results of repeated measures of ANOVA
.
Table 5: Comparing the scores of SF-36 questionnaire domains at base time, post-treatment and in follow-up time with the results of repeated measures of ANOVA
* Significant differences compared to SMT group, # significant differences compared to CST group, P01: Comparison of Post-treatment with base time, P02: Comparison of follow up with base time, P12: Comparison of Follow up by Post-treatment
In Table 5 the scores of SF-36 questionnaire domains was compared in three methods at Base time, Post-treatment and in follow-up time with the results of repeated measures of ANOVA. The results of Table 5 demonstrated that all three methods of CST, SMT, and MET was effective in all domains of SF-36 questionnaire including physical function, role physical, body pain, general health, vitality, social functioning, role emotional, total physical health, and total mental health except mental health that MET was not effective on it. CST was more effective than MET and SMT in control of variables of quality of life post-treatment and in follow up. In addition, in CST group this result continued during follow-up period.
Discussion
Based on the results of the present study, all three methods were significantly effective in post-treatment pain control, post-treatment disability, and improving depression after treatment, but CST was significantly more effective than SMT and MET. Also, the pain control process and the depression improvement were continued in the CST group after follow-up, but not in the other groups. Based on the results of the SF-36 questionnaire, all three methods have been effective in improving the quality of life after treatment. CST was more effective in controlling the quality of life post-treatment and in follow up than other methods. In addition, all 3 methods were effective to improve all domains in the quality of life questionnaire (SF-36) including physical activity, physical role, body pain, general health, vitality, social function, emotional role, total physical health and total health mental health after the treatment, except for mental health that MET was not effective. CST was more effective in controlling the domains of quality of life after treatment and in follow up than 2 other methods. Also, the improvement in quality of life domains in the CST group continued after follow-up.
In the Castro-Sánchez study on NCLBP patients, 10 sessions of CST led to a significant reduction in pain intensity.12 In the study of Elden et al., the effect of CST on pelvic pain was investigated in pregnant women. The results showed a significant decrease in morning pain in these subjects.13 In a study by Białoszewski et al., patients with NCLBP were treated with CST and trigger point therapy. In both methods the severity and frequency of pain were reduced in both ways.34 In Haller's study, 8-week CST was performed for people with chronic neck pain. In comparison with the sham treated group in the craniosacral group, the severity of pain significantly improved after treatment and follow-up. In that study, CST was indicated to improve the quality of life of patients with chronic neck pain.14 Few studies have shown CST is effective in improving functional disability and acute lower back pain.13,14,15 Studies showed that the level of depression decreased after CST, although this difference was not significant.14,35 An improvement in quality of life after CST was demonstrated in patients with fibromyalgia35 and multiple sclerosis.36 Morone, Paolucci, and Nazarzadeh also referred to the effect of SMT on pain relief in their studies, which was consistent with the results of this study.17-19 Additionally, some studies showed that MET was effective in reducing pain in patients.6,7,37-39 The incapacity rate was improved by MET.7,37-40
The mechanism of action of CST can be explained as follow; it is a method for the removal of facial constraints between cranium and sacrum.11 The craniosacral system involves the structures of the central nervous system, including skull, cranial sutures, CSF, as well as brain and spinal cord membranes. It is affected by the musculoskeletal system,41 and is also thought to be related to the vascular system, endocrine, and the sympathetic and parasympathetic nervous systems.42 In the craniosacral theory, fascial constraints in the craniosacral system lead to abnormal arrhythmic movement CSF. There is an evidence that fascia is involved in reducing pain. In case of increase in the activity of fascial nociceptors in restricted connective tissue, tissue stiffness, muscle tension and pain increase, and CST decreases the pain by reduction of fascial restrictions.10,42
The effect of CST on reducing depression can be explained by the following sentences. It seems that CST as a soft tissue manipulation leading to increased parasympathetic activity, which provides comfort and facilitation and cognitive processes.20 CST, on the other hand, can reduce cortisol levels. It also increases the level of serotonin in people by improving the efficacy of fascial visceral and eliminating visceral constraint.35 Regarding the high levels of cortisol in individuals with depression and their lower serotonin levels,43,44 CST can be effective in reducing depression.
CST, by removal of pressure on the membrane and cranium, result in natural movement of each bone and suture junction between these bones. CST removes pressure patterns which regulating the cycle of the brain, rhythm of the craniosacral, and accelerating the circulation of the CSF,21 thereby affecting the entire body. CST also reduces the muscle tone and causes relaxation and mood improvement in individuals.22 By removing the fascial restriction, it can lead to improve sleep.35 Regarding the mentioned cases, and controlling the pain and disability and depression CST can improves people's quality of life. Continuous efficacy of CST is explained by its effect on normalizing the environment around the brain, which can strengthen the body's self-healing system.45
Conclusion
According to the results of the study craniosacral therapy, and sensorimotor training, were all effective in improvement of pain, depression, functional disability, and muscle energy technique quality of life of patients with NSLBP. Craniosacral therapy is more effective than sensorimotor training and muscle energy technique in post-treatment and follow up. In addition, the effect of craniosacral therapy was continuous after two months follow up but it was not similar for sensorimotor training and muscle energy technique.
Limitation
The limitation of the study is comparatively a small sample size and enrollment of only few clinics. We recommend larger, multi-center studies to further validate our results.
Conflicts of interest
There is no conflict of interest for the present study.
Authors’ contribution
CG: Study design and concept
AA: Study design, Conducted the study
JS: Conducted the study, data collection
MD: Statistical analysis
NM: Literature review and writing the draft
References
1- PhD (Physiotherapy), Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
2- Assistant Professor, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
3- Associate Professor, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran.
*Correspondence: Ali Amiri, Assistant Professor, Rehabilitation Research Center, Department of Physiotherapy, School of Rehabilitation Sciences, Iran University of Medical Sciences, Tehran, Iran; E-mail: aliamiri12@protonmail.com; Phone: +989123658547
Abstract
Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
Keywords: Low Back Pain; Craniosacral Therapy; Muscle Energy Technique; Sensorimotor Training
Abbreviations: CST - Craniosacral therapy; MET - Muscle energy technique; SMT - Sensorimotor training; NCLBP - Non-specific chronic low back pain; ODQ - Oswestry functional disability questionnaire; 36-SF - 36-item short form health survey; BDI - Beck depression inventory; ROM - Range of motion
Citation: Ghasemi C, Amiri A, Sarrafzadeh J, Dadgoo M, Maroufi N. Comparison of the effects of craniosacral therapy, muscle energy technique, and sensorimotor training on non-specific chronic low back pain. Anaesth. pain intensive care 2020;24(5):532-543
Received: 21 July 2020, Reviewed: 14 August 2020, Revised: 15 August 2020, Accepted: 15 August 2020
DOI: https://doi.org/10.35975/apic.v24i5.1362
Introduction
Non-specific chronic low back pain (NCLBP) is a low back pain which is not attributable to a distinguishable, recognized certain pathology.1 Low back pain is estimated to be one of the important reasons of disability adjusted life years (DALYs).2 Non-specific Chronic low back pain (NCLBP) is a common problem.1 The lifetime occurrence of low back pain is informed to be 84%, and the frequency of chronic low back pain is around 23%, and about 11-12% of the people being disabled by low back pain.1 NCLBP is the most prevalent form of low back pain. NCLBP is mostly common at the age of 35 to 55 y.3 Hence, low back pain has a severe influence on the workforce and lead to a significant socioeconomic effects.3
Muscle Energy Technique (MET) is a multipurpose method conventionally used to address muscular tension, pain, and joint dysfunction and to develop range of motion (ROM).4 MET is a method in that the patient supplies the curative force, rather than the care giver.5 It was shown that MET is effective in decreasing lumbopelvic pain,6 decreasing disability in acute LBP,7 and Improving lumbar and cervical ROM in asymptomatic people.8 Recently, it is shown that MET is effective in the treatment of LBP, nevertheless it requires to be compared with other manual therapy methods.9
Craniosacral therapy (CST) is an alternative and complementary therapy which claimed to release the tension of the muscles, ligaments, and fascia in the sacral area.10 CST seems activate central pain inhibitory centers.11 CST is suggested for all musculoskeletal conditions particularly back pain 10, 11. It was shown that CST has effect on non-specific chronic low back pain,12 pelvic pain,13 chronic neck pain,14 and acute lower back pain.15
Recent research has indicated that proprioceptive sense is related to back pain and these individuals have weaker proprioceptive sense.16 It is demonstrated that Sensorimotor Training (SMT) can improve the proprioceptive sense. Studies have shown the effect of SMT on chronic low back pain control.17-19
NCLBP has become of the main public health issues throughout the world.1 The prevalence of chronic NCLBP is considerable and a percentage of the population being disabled by it 1. Also, it has a severe effect on the workforce and cause a significant socioeconomic effects3 Therefore, finding an effective method for treatment is important. Craniosacral therapy as a soft tissue manipulation leading to increased parasympathetic activity, which provides comfort and facilitation and cognitive processes.20 It removes pressure patterns which regulating the cycle of the brain, rhythm of the craniosacral, and accelerating the circulation of the CSF,21 thereby affecting the entire body. CST decreases the muscle tone and causes relaxation and mood improvement in individuals.22 Therefore, the hypothesis of this study is that whether CST has more effect on NCLBP rather than met and Smt. although there are studies that evaluated the effect of MET, SMT, or CST methods on NCLBP patients, no study compared the effect of these three methods on NCLBP. The aim of the present study is to assess the effectiveness of MET, CST, and CST on pain control, disability, depression, and quality of life of patients with NCLBP.
Methodology
In this randomized clinical trial (IRCT20170117032020N3) study 45 patients with NCLBP who referred to physiotherapy clinic of School of Rehabilitation of Iran University of Medical Sciences from September 2016 until November 2017 were participated. The sampling method was non-random. The number of samples was calculated through G-Power software and based on the studies of Volpe et al.23 and Salavati et al.24 and the following sample size was obtained:
In this study, α (probability of error of the first type) is equal to 0.05 and β (probability of error of the second type) is equal to 80%, based on which the effect size = 1. Therefore, currently the number of people studied in each of the 3 groups of 15 people is considered.
The NCLBP were defined as a localized pain in the lumbar region (from the twelfth rib to the gluteal fold) for 3 months continuously or repeatedly for more than six months and with an intensity of less than 6 to at least 3 based on the visual scale of the pain and it is defined by a specialist. The inclusion criteria were having low back pain below the costal margin and above inferior gluteal folds and suffering from low back pain (LBP) for more than 6 months; having the age range of 20 to 40 y old, and the disability level of more than 14% and less than 50% according to Oswestry questionnaire; and the exclusion criteria were pregnancy, history of neurologic disorder, infection, seizure, inflammatory diseases, tumor, lumbar fracture, and lumbar surgery. The eligible subjects were randomly divided in three groups including CST (n =15), SMT (n = 15), and MET (n = 15). Patients were matched for age, sex and body mass index in all groups. The study was approved by ethical committee of Iran University of Medical Sciences (IR.IUMS.REC139509211342216). Written consent was obtained from all participants. The interventions were performed as follow in 3 groups:
An experienced craniosacral therapist carried out the CST. Modified therapeutic protocol by Upledger and Vredevoogd was used for CST.25 Patients received 10 session of CST in 5 weeks (2 sessions per week) and each session lasts 45 minutes. A session contains 4 phases including in prone position, in side-lying position behind the therapist, in side-lying in front of the therapist, and in supine position (Figure 1); Patients were in each position for 10 minutes. To feel and follow craniosacral movements, craniosacral therapist put her both hands on two regions or bones.25
In MET group 10 sessions of muscle energy technique in 5 weeks (2 sessions per week) 26 were performed for treatment of posterior rotation of the right or left innominate (to restore anterior rotation) and anterior rotation of the right or left innominate (to restore posterior rotation) dysfunctions (with regard to the side of the dysfunction) which were done 3-5 times per session with 5-10 sec time of hold for each position, and correction of a sacroiliac joint up slip which was done 12 times each session27 (Figure 2). Dysfunctions were determined using the following tests: Standing flexion test, Gillet test or Stork test (sacral fixation test), supine to sit test, and sitting flexion test.
In SMT group, patients received 10 sessions of balance training in 5 weeks (2 sessions per week) based on global approach by Page (2006). According to this approach, patients’ progress evaluated through three stages of static, dynamic, and functional during 10 sessions.28 In each stage, patients experience different postures and base of support and their center of gravity is being challenged (Figure 3). To determine the pain intensity a 10 cm visual analogue scale (VAS) was used. VAS contains 0 to 10 degree which 0 represents “no pain” and 10 represent “worst imaginable pain”. This scale is a reliable and valid measurement tool for pain assessment in NCLBP.29 Participants were asked to score their pain at the test time.
The Persian version of Oswestry functional disability questionnaire (ODQ) was used to assess the functional disability of patients (16). ODQ includes 10 items, each scored from 0 to 5 and the highest score is 50 which should be doubled to show the percentage. The higher Oswestry disability index (ODI) scores shows the higher level of disability. According to the Baradaran et al. study, Infraclass correlation coefficient (ICC) for each item ranged from 0.43 to 0.80 that shows a good reliability and reproducibility of each item. Cronbach's α coefficient was 0.69 that shows a good internal consistency for Persian version of ODQ.30
To evaluate the depression in patients the Beck depression inventory-II (BDI-II) was used. BDI-II contains 21 questions. Each question has 4 sentences describing the patient’s situation. BDI-II score ranges from 0 to 63 and the higher scores designates the higher level of depression.31 Ghassemzadeh et al. showed that the BDI-II Persian version had high internal consistency (Cronbach’s α = 0.87) and acceptable test-retest reliability (r = 0.74).32
The Persian version of 36-item short form health survey (SF-36) was used to measure the quality of life of patients.33 This questionnaire has 8 domains including physical function, body pain, social functioning, general health, role physical, vitality, role emotional and mental health. Each domain is scored from 0 to 100 scale that the higher scores specify the better health condition. Montazeri et al. revealed that the internal consistency for all eight SF-36 scales met the minimum reliability standard, the Cronbach's alpha coefficients was ranged from 0.77 to 0.90 except for the vitality scale that was 0.65.33
Patients were asked to report the VAS score and fill the ODQ, BDI-II, and SF-36 questioners before the treatment, after the last session of treatment, and after 2 months follow up.
SPSS version 16 was used to analyze the data. ANOVA and Tukey post hoc tests used to compare the data. Repeated measures of analysis of variance (ANOVA, Wilks' Lambda test) was used to assess the effects of group, time and their interaction for VAS,
In MET group 10 sessions of muscle energy technique in 5 weeks (2 sessions per week)26 were performed for treatment of posterior rotation of the right or left innominate (to restore anterior rotation) and anterior rotation of the right or left innominate (to restore posterior rotation) dysfunctions (with regard to the side of the dysfunction) which were done 3-5 times per


ODI, BDI-II and SF-36. Values were significant at p < 0.001. Flowchart of study is shown in Figure 4.
Results
The results of repeated measure of ANOVA test showed that VAS changes were significant at all 3 times in each of the SMT, CST and MET groups (p < 0.001, p < 0.001, and p < 0.001). The result of the ANOVA test showed that the VAS variable in the baseline time was not significantly different between the groups, but in after treatment and post-follow up, there was a significant difference (p = 0.137, p < 0.001, p < 0.001). The result of the Tukey's post hoc test showed that VAS changes in post-treatment and follow-up time in the CST group were significantly different in

Table 1: Comparing VAS scores at Base time, Post-treatment and in follow-up time with the results of repeated measures of ANOVA (Mean ± SD)
| Intervention Groups | Time | p value | |||||
| Base time | Post-treatment | Follow up | P01 | P02 | P12 | P | |
| SMT | 6.52 ± 1.01 | 3.05 ± 0.80 | 4.17 ± 0.86 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| CST | 6.92 ± 1.00 | 1.36 ± 0.62* | 0.33 ± 0.51* | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| EMT | 6.20 ± 1.14 | 2.20 ± 0.77# | 4.06 ± 0.88# | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| P | 0.137 | < 0.001 | < 0.001 | ||||
| Results of repeated measure of ANOVA | Time effect | p < 0.001 | F = 851.561 | Effect size = 0.952 | |||
| Group effect | p < 0.001 | F = 22.090 | Effect size = 0.507 | ||||
| Interaction Effect | p < 0.001 | F = 87.080 | Effect size = 0.802 | ||||




that ODI changes in post-treatment and follow-up time in the CST group were significantly different in comparison to SMT group, and the changes in ODI at after treatment and follow-up times in the CST group compared with the MET group had a significant difference (Table 2; Figure 2). The results of repeated measure of ANOVA test showed that BDI changes were significant at 3 readings in each of the SMT, CST and MET groups (p < 0.001, p < 0.001, p < 0.001). The result of the ANOVA test showed that the BDI variable in the baseline time was not significantly different between 3 groups, but in after treatment and post-follow up, there was a significant difference (p = 0.579, p <0.001, p <0.001). The result of the Tukey's post hoc test showed that BDI changes in post-treatment and follow-up time in the CST group were significantly different in comparison to SMT group, and the changes in BDI at after treatment and follow-up times in the CST group compared with the MET group had a significant difference (Table 3; Figure 3). The results of repeated measure of ANOVA test showed that SF-36 changes were significant at 3 readings in each of the SMT, CST and MET groups (p < 0.001, p < 0.001, p < 0.001). The result of the ANOVA test showed that the SF-36 variable in the baseline time was not significantly different between 3 groups, but after treatment and post-follow up, there was a significant difference (p = 0.707, p < 0.001, p < 0.001). The result of the Tukey's post hoc test showed that BDI changes in post-treatment and follow-up time in the CST group were significantly different in comparison to SMT group, and the changes in SF-36 at after treatment and follow-up times in the CST group compared with the group MET had a significant difference (Table 4; Figure 4).
| Table 2: Comparing ODI scores at base time, post-treatment and in follow-up time with the results of repeated measures of ANOVA | |||||||
| Intervention Groups | Time | p value | |||||
| Base time | Post-treatment | Follow up | P01 | P02 | P12 | P | |
| SMT | 32.40 ± 10.98 | 17.07 ± 7.28 | 22.13 ± 6.90 | < 0.001 | 0.002 | 0.018 | < 0.001 |
| CST | 34.50 ± 8.50 | 5.38 ± 3.07* | 0.75 ± 1.43* | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| EMT | 30.47 ± 8.07 | 18.87 ± 6.59# | 19.07 ± 5.18# | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| P | 0.485 | < 0.001 | < 0.001 | ||||
| Results of repeated measure of ANOVA | Time effect | p < 0.001 | F = 199.090 | Effect size = 0.822 | |||
| Group effect | p < 0.001 | F = 16.389 | Effect size = 0.433 | ||||
| Interaction Effect | p < 0.001 | F = 27.858 | Effect size = 0.564 | ||||
| * Significant differences compared to SMT group, # significant differences compared to CST group, P01: Comparison of Post-treatment with base time, P02: Comparison of follow up with base time, P12: Comparison of Follow up by Post-treatment | |||||||
| Table 3: Comparing BDI scores at base time, post-treatment and in follow-up time with the results of repeated measures of ANOVA | |||||||
| Intervention Groups | Time (Mean ± SD) | p value | |||||
| Base time | Post-treatment | Follow up | P01 | P02 | P12 | P | |
| SMT | 25.67 ± 6.77 | 15.60 ± 5.52 | 20.53 ± 5.89 | < 0.001 | 0.001 | 0.009 | < 0.001 |
| CST | 27.38 ± 8.61 | 5.88 ± 4.14* | 2.13 ± 2.41* | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| EMT | 28.60 ± 7.41 | 20.53 ± 9.97# | 22.00 ± 7.43# | < 0.001 | 0.010 | 1.000 | < 0.001 |
| P | 0.579 | < 0.001 | < 0.001 | ||||
| Results of repeated measure of ANOVA | Time effect | p < 0.001 | F = 118.547 | Effect size = 0.734 | |||
| Group effect | p < 0.001 | F = 18.617 | Effect size = 0.464 | ||||
| Interaction Effect | p < 0.001 | F = 24.329 | Effect size = 0.531 | ||||
Table 4: Comparing SF-36 scores at base time, post-treatment and in follow-up time with the results of repeated measures of ANOVA
| Groups | Time (Mean ± SD) | P value | |||||
| Base time | Post-treatment | Follow up | P01 | P02 | P12 | P | |
| SMT | 45.80 ± 18.21 | 68.47 ± 14.97 | 58.87 ± 15.17 | < 0.001 | 0.001 | 0.010 | < 0.001 |
| CST | 35.31 ± 13.43 | 89.81 ± 5.23* | 96.56 ± 5.87* | < 0.001 | < 0.001 | 0.021 | < 0.001 |
| EMT | 46.60 ± 14.79 | 71.20 ± 15.23# | 59.40 ± 16.36# | < 0.001 | 0.012 | < 0.001 | < 0.001 |
| P | 0.089 | < 0.001 | < 0.001 | ||||
| Results of repeated measure of ANOVA | Time effect | p < 0.001 | F = 223.665 | Effect size = 0.839 | |||
| Group effect | p = 0.001 | F = 8.672 | Effect size = 0.287 | ||||
| Interaction Effect | p < 0.001 | F = 45.276 | Effect size = 0.678 | ||||
|
*Significant differences compared to SMT group, # significant differences compared to CST group, P01: Comparison of Post-treatment with base time, P02: Comparison of follow up with base time, P12: Comparison of Follow up by Post-treatment |
|||||||
Table 5: Comparing the scores of SF-36 questionnaire domains at base time, post-treatment and in follow-up time with the results of repeated measures of ANOVA
| Variables | Groups | Time (Mean ± SD) | p value | |||||
| Base time | Post-treatment | Follow up | P01 | P02 | P12 | P | ||
| Physical function | SMT | 40.00 ± 16.03 | 62.33 ± 20.86 | 59.33 ± 18.69 | < 0.001 | 0.001 | 1.000 | < 0.001 |
| CST | 30.63 ± 18.24 | 93.44 ± 3.96* | 100.00 ± 0.00* | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| EMT | 44.33 ± 15.90 | 70.33 ± 17.36# | 55.33 ± 21.33# | < 0.001 | 0.012 | < 0.001 | < 0.001 | |
| P | 0.078 | < 0.001 | < 0.001 | |||||
| Role Physical | SMT | 28.33 ± 31.14 | 65.00 ± 24.64 | 53.33 ± 32.55 | < 0.001 | 0.008 | 0.392 | < 0.001 |
| CST | 20.31 ± 26.17 | 95.31 ± 10.07* | 100.00 ± 0.00* | < 0.001 | < 0.001 | 0.248 | < 0.001 | |
| EMT | 26.67 ± 27.49 | 63.33 ± 26.50# | 41.67 ± 29.37# | < 0.001 | 0.209 | 0.021 | < 0.001 | |
| P | 0.707 | < 0.001 | < 0.001 | |||||
| Body pain | SMT | 44.40 ± 15.22 | 72.47 ± 13.52 | 59.60 ± 13.29 | < 0.001 | < 0.001 | 0.001 | < 0.001 |
| CST | 40.94 ± 20.94 | 87.75 ± 12.51* | 100.00 ± 0.00* | < 0.001 | < 0.001 | 0.004 | < 0.001 | |
| EMT | 44.73 ± 17.37 | 76.93 ± 12.53# | 65.53 ± 14.28# | < 0.001 | 0.019 | 0.004 | < 0.001 | |
| P | 0.810 | 0.025 | < 0.001 | |||||
| General health | SMT | 47.60 ± 25.60 | 64.93 ± 17.16 | 51.93 ± 18.18 | 0.001 | 1.000 | 0.008 | 0.001 |
| CST | 34.69 ± 13.22 | 78.00 ± 6.54* | 98.25 ± 2.76* | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| EMT | 45.60 ± 23.69 | 66.93 ± 20.41# | 57.73 ± 17.16# | 0.002 | 0.188 | 0.037 | 0.001 | |
| P | 0.204 | < 0.001 | < 0.001 | |||||
| Vitality | SMT | 50.00 ± 13.88 | 64.33 ± 12.79 | 55.67 ± 10.83 | < 0.001 | 0.219 | < 0.001 | < 0.001 |
| CST | 40.00 ± 17.12 | 85.31 ± 7.84* | 93.44 ± 4.73* | < 0.001 | < 0.001 | 0.018 | < 0.001 | |
| EMT | 53.67 ± 11.25 | 67.33 ± 9.79# | 59.67 ± 13.55# | 0.004 | 0.459 | 0.064 | 0.002 | |
| P | 0.031 | < 0.001 | < 0.001 | |||||
| Social Functioning | SMT | 58.60 ± 16.62 | 85.13 ± 14.35 | 71.80 ± 12.88 | < 0.001 | 0.002 | < 0.001 | < 0.001 |
| CST | 48.69 ± 19.32 | 92.31 ± 10.01* | 100.00 ± 0.00* | < 0.001 | < 0.001 | 0.023 | < 0.001 | |
| EMT | 60.27 ± 15.74 | 81.87 ± 18.18# | 74.40 ± 15.87# | < 0.001 | 0.005 | 0.045 | < 0.001 | |
| P | 0.143 | < 0.001 | < 0.001 | |||||
| Role emotional | SMT | 37.80 ± 33.13 | 64.40 ± 29.61 | 55.47 ± 32.66 | < 0.001 | 0.047 | 0.660 | 0.001 |
| CST | 20.81 ± 36.27 | 95.88 ± 11.27* | 100.00 ± 0.00* | < 0.001 | < 0.001 | 0.492 | < 0.001 | |
| EMT | 37.73 ± 30.62 | 73.33 ± 33.87# | 57.87 ± 36.72# | 0.001 | 0.098 | 0.341 | 0.001 | |
| P | 0.273 | < 0.001 | < 0.001 | |||||
| Total physical health | SMT | 60.27 ± 13.97 | 69.33 ± 11.96 | 63.47 ± 9.89 | 0.001 | 0.374 | 0.008 | < 0.001 |
| CST | 52.56 ± 14.84 | 90.81 ± 4.86* | 94.88 ± 4.50* | < 0.001 | < 0.001 | 0.041 | < 0.001 | |
| EMT | 59.73 ± 14.45 | 69.33 ± 13.32# | 64.00 ± 11.31# | - | - | - | 0.077 | |
| P | 0.260 | < 0.001 | < 0.001 | |||||
| Total mental health | SMT | 42.00 ± 18.68 | 65.73 ± 14.91 | 56.00 ± 15.22 | < 0.001 | 0.002 | 0.024 | < 0.001 |
| CST | 33.06 ± 10.71 | 87.75 ± 5.81* | 98.31 ± 1.40* | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| EMT | 43.00 ± 14.98 | 68.93 ± 14.41# | 56.00 ± 16.44# | < 0.001 | 0.022 | 0.002 | < 0.001 | |
| P | 0.139 | < 0.001 | < 0.001 | |||||
| Mental Health | SMT | 50.80 ± 18.22 | 69.73 ± 14.76 | 59.73 ± 13.83 | < 0.001 | 0.016 | 0.003 | < 0.001 |
| CST | 43.38 ± 15.47 | 90.00 ± 6.63* | 94.81 ± 9.73* | < 0.001 | < 0.001 | 0.361 | < 0.001 | |
| EMT | 51.33 ± 14.89 | 71.80 ± 15.54# | 62.60 ± 15.70# | < 0.001 | 0.024 | 0.003 | < 0.001 | |
| P | 0.319 | < 0.001 | < 0.001 | |||||
In Table 5 the scores of SF-36 questionnaire domains was compared in three methods at Base time, Post-treatment and in follow-up time with the results of repeated measures of ANOVA. The results of Table 5 demonstrated that all three methods of CST, SMT, and MET was effective in all domains of SF-36 questionnaire including physical function, role physical, body pain, general health, vitality, social functioning, role emotional, total physical health, and total mental health except mental health that MET was not effective on it. CST was more effective than MET and SMT in control of variables of quality of life post-treatment and in follow up. In addition, in CST group this result continued during follow-up period.
Discussion
Based on the results of the present study, all three methods were significantly effective in post-treatment pain control, post-treatment disability, and improving depression after treatment, but CST was significantly more effective than SMT and MET. Also, the pain control process and the depression improvement were continued in the CST group after follow-up, but not in the other groups. Based on the results of the SF-36 questionnaire, all three methods have been effective in improving the quality of life after treatment. CST was more effective in controlling the quality of life post-treatment and in follow up than other methods. In addition, all 3 methods were effective to improve all domains in the quality of life questionnaire (SF-36) including physical activity, physical role, body pain, general health, vitality, social function, emotional role, total physical health and total health mental health after the treatment, except for mental health that MET was not effective. CST was more effective in controlling the domains of quality of life after treatment and in follow up than 2 other methods. Also, the improvement in quality of life domains in the CST group continued after follow-up.
In the Castro-Sánchez study on NCLBP patients, 10 sessions of CST led to a significant reduction in pain intensity.12 In the study of Elden et al., the effect of CST on pelvic pain was investigated in pregnant women. The results showed a significant decrease in morning pain in these subjects.13 In a study by Białoszewski et al., patients with NCLBP were treated with CST and trigger point therapy. In both methods the severity and frequency of pain were reduced in both ways.34 In Haller's study, 8-week CST was performed for people with chronic neck pain. In comparison with the sham treated group in the craniosacral group, the severity of pain significantly improved after treatment and follow-up. In that study, CST was indicated to improve the quality of life of patients with chronic neck pain.14 Few studies have shown CST is effective in improving functional disability and acute lower back pain.13,14,15 Studies showed that the level of depression decreased after CST, although this difference was not significant.14,35 An improvement in quality of life after CST was demonstrated in patients with fibromyalgia35 and multiple sclerosis.36 Morone, Paolucci, and Nazarzadeh also referred to the effect of SMT on pain relief in their studies, which was consistent with the results of this study.17-19 Additionally, some studies showed that MET was effective in reducing pain in patients.6,7,37-39 The incapacity rate was improved by MET.7,37-40
The mechanism of action of CST can be explained as follow; it is a method for the removal of facial constraints between cranium and sacrum.11 The craniosacral system involves the structures of the central nervous system, including skull, cranial sutures, CSF, as well as brain and spinal cord membranes. It is affected by the musculoskeletal system,41 and is also thought to be related to the vascular system, endocrine, and the sympathetic and parasympathetic nervous systems.42 In the craniosacral theory, fascial constraints in the craniosacral system lead to abnormal arrhythmic movement CSF. There is an evidence that fascia is involved in reducing pain. In case of increase in the activity of fascial nociceptors in restricted connective tissue, tissue stiffness, muscle tension and pain increase, and CST decreases the pain by reduction of fascial restrictions.10,42
The effect of CST on reducing depression can be explained by the following sentences. It seems that CST as a soft tissue manipulation leading to increased parasympathetic activity, which provides comfort and facilitation and cognitive processes.20 CST, on the other hand, can reduce cortisol levels. It also increases the level of serotonin in people by improving the efficacy of fascial visceral and eliminating visceral constraint.35 Regarding the high levels of cortisol in individuals with depression and their lower serotonin levels,43,44 CST can be effective in reducing depression.
CST, by removal of pressure on the membrane and cranium, result in natural movement of each bone and suture junction between these bones. CST removes pressure patterns which regulating the cycle of the brain, rhythm of the craniosacral, and accelerating the circulation of the CSF,21 thereby affecting the entire body. CST also reduces the muscle tone and causes relaxation and mood improvement in individuals.22 By removing the fascial restriction, it can lead to improve sleep.35 Regarding the mentioned cases, and controlling the pain and disability and depression CST can improves people's quality of life. Continuous efficacy of CST is explained by its effect on normalizing the environment around the brain, which can strengthen the body's self-healing system.45
Conclusion
According to the results of the study craniosacral therapy, and sensorimotor training, were all effective in improvement of pain, depression, functional disability, and muscle energy technique quality of life of patients with NSLBP. Craniosacral therapy is more effective than sensorimotor training and muscle energy technique in post-treatment and follow up. In addition, the effect of craniosacral therapy was continuous after two months follow up but it was not similar for sensorimotor training and muscle energy technique.
Limitation
The limitation of the study is comparatively a small sample size and enrollment of only few clinics. We recommend larger, multi-center studies to further validate our results.
Conflicts of interest
There is no conflict of interest for the present study.
Authors’ contribution
CG: Study design and concept
AA: Study design, Conducted the study
JS: Conducted the study, data collection
MD: Statistical analysis
NM: Literature review and writing the draft
References
- Balague F, Mannion AF, Pellise F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482-491. [PubMed] DOI: 1016/S0140-6736(11)60610-7
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017 Sep 16;390(10100):1260-1344. [PubMed] DOI: 1016/S0140-6736(17)32130-X
- Low back pain. 2013. Available from: https://www.who.int/medicines/areas/priority_medicines/BP6_24LBP.pdf
- Varghese S. A study on the effectiveness of muscle energy techniques compared to manipulation therapy in chronic low back pain. Int J Latest Res Sci Technol. 2012;1(2):D214-217. DOI: 1142%2FS1013702518500051
- DeRosa CP, Porterfield JA. A physical therapy model for the treatment of low back pain. Phys Ther. 1992;72(4):261-219. [PubMed] DOI: 1093/ptj/72.4.261
- Selkow NM, Grindstaff TL, Cross KM, Pugh K, Hertel J, Saliba S. Short-term effect of muscle energy technique on pain in individuals with non-specific lumbopelvic pain: a pilot study. J Man Manip Ther. 2009;17(1):E14-18. [PubMed] DOI: 1179/jmt.2009.17.1.14E
- Wilson E, Payton O, Donegan-Shoaf L, Dec K. Muscle energy technique in patients with acute low back pain: a pilot clinical trial. J Orthop Sports Phys Ther. 2003;33(9):502-512. [PubMed] DOI: 2519/jospt.2003.33.9.502
- Schenk R, Adelman K, Rousselle J. The effects of muscle energy technique on cervical range of motion. J Manual Manipulative Ther. 1994;2(4):149-155. DOI: 1179/jmt.1994.2.4.149
- Day JM, Nitz AJ. The effect of muscle energy techniques on disability and pain scores in individuals with low back pain. J Sport Rehabil. 2012;21(2):194-198. [PubMed] DOI: 1123/jsr.21.2.194
- Green C, Martin CW, Bassett K, Kazanjian A. A systematic review and critical appraisal of the scientific evidence on craniosacral therapy. Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]: Centre for Reviews and Dissemination (UK); 1999. Available from: https://www.ncbi.nlm.nih.gov/books/NBK67710/
- Upledger JE, Vredevoogd JD. Craniosacral therapy: Citeseer; 1983.
- Castro-Sanchez AM, Lara-Palomo IC, Mataran-Penarrocha GA, Saavedra-Hernandez M, Perez-Marmol JM, Aguilar-Ferrandiz ME. Benefits of Craniosacral Therapy in patients with chronic low back pain: a randomized controlled trial. J Altern Complement Med. 2016;22(8):650-657. [PubMed] DOI: 1089/acm.2016.0068
- Elden H, Ostgaard HC, Glantz A, Marciniak P, Linner AC, Olsen MF. Effects of craniosacral therapy as adjunct to standard treatment for pelvic girdle pain in pregnant women: a multicenter, single blind, randomized controlled trial. Acta Obstet Gynecol Scand. 2013;92(7):775-782. [PubMed] DOI: 1111/aogs.12096
- Haller H, Lauche R, Cramer H, Rampp T, Saha FJ, Ostermann T, et al. Craniosacral therapy for the treatment of chronic neck pain: a randomized sham-controlled trial. Clin J Pain. 2016;32(5):441-449. [PubMed] DOI: 1097/AJP.0000000000000290
- Powell W 2nd, Knaap SF. Cranial treatment and spinal manipulation for a patient with low back pain: a case study. J Chiropr Med. 2015;14(1):57-61. [PubMed] DOI: 1016/j.jcm.2014.12.001
- Brumagne S, Cordo P, Verschueren S. Proprioceptive weighting changes in persons with low back pain and elderly persons during upright standing. Neurosci Lett. 2004;366(1):63-66. [PubMed] DOI: 1016/j.neulet.2004.05.013
- Paolucci T, Fusco A, Iosa M, Grasso MR, Spadini E, Paolucci S, et al. The efficacy of a perceptive rehabilitation on postural control in patients with chronic nonspecific low back pain. Int J Rehabil Res. 2012;35(4):360-6. DOI: 1097/MRR.0b013e328356427c www.ncbi.nlm.nih.gov/pubmed/22842780
- Nazarzadeh M, Letafatkar A, Saboonchi R. Effect of sensory-motor exercises on proprioceptive sense and neuromuscular coordination in patients with chronic non-specific low back pain. Sport Medicine Studies. 2014;15:71-88.
- Morone G, Iosa M, Paolucci T, Fusco A, Alcuri R, Spadini E, et al. Efficacy of perceptive rehabilitation in the treatment of chronic nonspecific low back pain through a new tool: a randomized clinical study. Clin Rehabil. 2012;26(4):339-350. [PubMed] DOI: 1177/0269215511414443
- Field T, Morrow C, Valdeon C, Larson S, Kuhn C, Schanberg S. Massage reduces anxiety in child and adolescent psychiatric patients. J Am Acad Child Adolesc Psychiatry. 1992;31(1):125-131. [PubMed] DOI: 1097/00004583-199201000-00019
- Upledger J, Wanveer T. Helping the Brain Drain: How CranioSacral Therapy Aids ADD/ADHD. Massage Today. 2007. Available from: https://www.massagetoday.com/articles/13578/Helping-the-Brain-Drain-How-CranioSacral-Therapy-Aids-ADDADHD
- Pishyareh E, Ebrahimi E, Hosseini SA, Kazem-Nejad A, Ramin M. The impact of cranios acral therapy on inhibition of hypertonicity of the lower limb in children with dipelgia spastic cerebral palsy of 3-8 years old. Arc Rehab. 2001;1(3):7-11. [Free Full Text]
- della Volpe R, Popa T, Ginanneschi F, Spidalieri R, Mazzocchio R, Rossi A. Changes in coordination of postural control during dynamic stance in chronic low back pain patients. Gait Posture. 2006;24(3):349-355. [PubMed] DOI: 1016/j.gaitpost.2005.10.009
- Salavati M, Mazaheri M, Negahban H, Ebrahimi I, Jafari AH, Kazemnejad A, et al. Effect of dual-tasking on postural control in subjects with nonspecific low back pain. Spine (Phila Pa 1976). 2009;34(13):1415-1421. [PubMed] DOI: 1097/BRS.0b013e3181a3a917
- Upledger J, Vredevoogd J. The spinal dura matter and sacrococcygeal complex. Craniosacral Therapy: Eastland Press, Seattle, WA; 1996. p. 131-51.
- Donatelli RA, Wooden MJ. Orthopaedic Physical Therapy-E-Book: Elsevier health sciences; 2009.
- Schamberger W. The Malalignment Syndrome: diagnosis and treatment of common pelvic and back pain: Elsevier Health Sciences; 2012.
- Page P. Sensorimotor training: A “global” approach for balance training. J Bodywork Movement Ther. 2006;10(1):77-84.
- Ogon M, Krismer M, Sollner W, Kantner-Rumplmair W, Lampe A. Chronic low back pain measurement with visual analogue scales in different settings. Pain. 1996;64(3):425-428. [PubMed] DOI: 1016/0304-3959(95)00208-1
- Baradaran A, Ebrahimzadeh MH, Birjandinejad A, Kachooei AR. Cross-Cultural Adaptation, Validation, and Reliability Testing of the Modified Oswestry Disability Questionnaire in Persian Population with Low Back Pain. Asian Spine J. 2016;10(2):215-219. [PubMed] DOI: 4184/asj.2016.10.2.215
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of general psychiatry. 1961;4(6):561-571. [PubMed] DOI: 1001/archpsyc.1961.01710120031004
- Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory--Second edition: BDI-II-PERSIAN. Depress Anxiety. 2005;21(4):185-192. [PubMed] DOI: 1002/da.20070
- Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14(3):875-882. [PubMed] DOI: 1007/s11136-004-1014-5
- Bialoszewski D, Bebelski M, Lewandowska M, Slupik A. Utility of craniosacral therapy in treatment of patients with non-specific low back pain. Preliminary report. Ortop Traumatol Rehabil. 2014;16(6):605-615. [PubMed] DOI: 5604/15093492.1135120
- Mataran-Penarrocha GA, Castro-Sanchez AM, Garcia GC, Moreno-Lorenzo C, Carreno TP, Zafra MD. Influence of craniosacral therapy on anxiety, depression and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. 2011;2011:178769. [PubMed] DOI: 1093/ecam/nep125
- Raviv G, Shefi S, Nizani D, Achiron A. Effect of craniosacral therapy on lower urinary tract signs and symptoms in multiple sclerosis. Complement Ther Clin Pract. 2009;15(2):72-75. [PubMed] DOI: 1016/j.ctcp.2008.12.006
- Ellythy MA. Efficacy of muscle energy technique versus strain counter strain on low back dysfunction. Bulletin of Faculty of Physical Therapy. 2012;17(2). [Free Full Text]
- Patel VD, Eapen C, Ceepee Z, Kamath R. Effect of muscle energy technique with and without strain–counterstrain technique in acute low back pain—A randomized clinical trial. Hong Kong Physiother J. 2018;38(01):41-51. [PubMed] DOI: 10.1142/s1013702518500051
- Phadke A, Bedekar N, Shyam A, Sancheti P. Effect of muscle energy technique and static stretching on pain and functional disability in patients with mechanical neck pain: A randomized controlled trial. Hong Kong Physiother J. 2016;35:5-11. [PubMed] DOI: 1016/j.hkpj.2015.12.002
- Patil PN, Chandu B, Metgud S, Khatri S. Effectiveness of muscle energy technique on quadratus lumborum in acute low back pain-randomized controlled trial. Ind J Physiother Occupational Ther. 2010;4(1):54-58.
- Kahkeshani K, Ward PJ. Connection between the spinal dura mater and suboccipital musculature: evidence for the myodural bridge and a route for its dissection--a review. Clin Anat. 2012;25(4):415-422. [PubMed] DOI: 1002/ca.21261
- Ferguson A. A review of the physiology of cranial osteopathy. J Osteopathic Med. 2003;6(2):74-84.
- Cowen PJ, Browning M. What has serotonin to do with depression? World Psychiatry. 2015;14(2):158-160. [PubMed] DOI: 1002/wps.20229
- Field T, Hernandez-Reif M, Diego M, Schanberg S, Kuhn C. Cortisol decreases and serotonin and dopamine increase following massage therapy. International Journal of Neuroscience. 2005;115(10):1397-1413. [PubMed] DOI: 1080/00207450590956459
- Upledger JE. Craniosacral therapy: Touchstone for natural healing: North Atlantic Books; 2001.