Amrita Gupta, MD1, Yogita Dwivedi, MD2, Sumi Saxena, MD3, Uma Srivastava, MD, DA4, Sandeep Mangla5, Sukhdev Mishra6
1Lecturer; 2Assistant professor; 4Professor; 5PG student
Department of Anesthesiology, Sarojini Naidu Medical College (SNMC), Moti Katra, Agra, Uttar Pradesh 282002, (India)
3Senior resident, Department of Anesthesiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), Rae Bareli Road, Lucknow, Uttar Pradesh 226014, (India)
6Scientist, Division of Biostatistics, National Institute of Occupational Health/ Indian Council of Medical Research; Department of Health Research, Ministry of Health & Family Welfare, Government of India, Meghani Nagar, Ahmedabad (India)
Correspondence: Dr Amrita Gupta, MD, Department of Anesthesiology, Sarojini Naidu Medical College (SNMC), Moti Katra, Agra, Uttar Pradesh 282002, (India)
ABSTRACT
Introduction: Dexmedetomidine provides stable perioperative hemodynamic profile with decreased requirement of opioids. It has neuroprotective effect and may be suitable anesthetic adjuvant when compared to fentanyl.
The main aim of our study was to compare dexmedetomidine and fentanyl in relation to blunting of sympathetic response to intubation and induction while secondary variables were to study their effect on perioperative hemodynamic changes, operative conditions, recovery profile and side effects.
Methodology: In this double blind randomized control trial 50 patients of ASA I and II grade scheduled for elective neurosurgery were selected over a period of 1 year, after obtaining written informed consent. Patients were randomly divided into two groups; in Group-D patient received 1 µg/kg of dexmedetomidine as loading dose within 10 min before induction and 2 µg/kg of fentanyl at induction and 0.04-0.05 µg/kg/min of dexmedetomidine as maintenance during surgery. In Group-F patient received induction with 3 µg/kg of fentanyl and maintained with 0.02-0.03 µg/kg/min of fentanyl.
Hemodynamic changes, cerebral relaxation store, recovery time and intraoperative and postoperative side effects were noted
Results: Baseline heart rate and BP was similar in both the groups. In Group-D and F, Heart rate and BP were increased from baseline during intubation, skull clamping and extubation but were within physiological limits. The rise in heart rate and BP was comparatively lower in Group-D as compared to Group-F. all the values were statistically significant (p < 0.05)
Cerebral relaxation score was lower in Group-D as compared to Group-F, along with faster recovery. During postoperative period there was no shivering nausea and vomiting in Group-D but in Group-F, 1 patient experienced shivering while 2 patients complained of nausea and vomiting.
Conclusion: In our study we found that dexmedetomidine provided better hemodynamic profile as compared to fentanyl with better cerebral relaxation score and recovery time. Hence we conclude that dimetindene is safer and effective alternate to fentanyl as an anesthetic adjuvant in neurosurgery.
Key words: Supratentorial craniotomies; Dexmedetomidine; Fentanyl; Anesthesia, General; Cerebral relaxation score
Citation: Gupta A, MD, Dwivedi Y, Saxena S, Srivastava U, Mangla S, Mishra S. A randomized control study of dexmedetomidine versus fentanyl as an anesthetic adjuvant in supratentorial craniotomies. Anaesth Pain & Intensive Care 2017;21(3): 306-311
Received - 19 Dec 2016; Reviewed – 23 Jan, 8 Mar 2017; Corrected – 26 Jun, 7 Aug 2017; Accepted – 25 Aug 2017
INTRODUCTION
The aim of neuroanesthesia is to protect the brain as much as possible with the means available to the anesthetist. The goals of intraoperative managements are to provide optimal operating conditions, maintain hemodynamic stability, adequate cerebral perfusion pressure, low ICP and to provide cerebral protection and rapid recovery.1 The intense surgical stimulus causes increase in sympathetic activity and marked changes in systemic blood pressure, cerebral blood flow and intracranial pressure. Perioperative hypertension is associated with intracranial bleed while low central blood pressure predisposes the patient to cerebral ischemia. During the intraoperative management these responses should be prevented, attenuated and managed for a favorable outcome.
Various drugs have been used to attenuate these responses especially at the time of intubation and rest of the surgery duration. Fentanyl is one of the most popular and most common drug used for the said purpose. It’s a short acting potent opioid which blunt these sympathetic responses however it is associated with side effects like respiratory depression. Dexmedetomidine is an α2 adrenoceptor agonist, which has sympatholytic, sedative, analgesic, opioid sparing and hemodynamic stabilizing properties without causing significant respiratory depression.2 These properties of dexmedetomidine would be consistent with the important goals of maintaining hemodynamic stability during neurosurgical procedures.
The main aim of our study was to compare dexmedetomidine and fentanyl in relation to blunting of sympathetic response to intubation and induction while secondary variables are to study their effect on perioperative hemodynamic changes, operative conditions, recovery profile and side effects.
METHODOLOGY
After obtaining informed written consent and approval of institutional ethical committee, this randomized double blind study was performed. Inclusion criteria was- ASA I and II patients, age 18 to 65 years, GCS > 12 undergoing supratentorial craniotomy under general anesthesia. The exclusion criteria were; patients with significant systemic disease like uncontrolled hypertension (blood pressure > 140/90), severe respiratory disease such as asthma or ischemic heart disease, alcoholics, drug addicts, psychiatric patients, patients who had taken opioids or benzodiazepines 48 hours prior to surgery, patient with active infection, and patients with BMI > 30 kg/m2.
Our study was double blind in which the resident who was giving the drug was not aware about the drug and in postoperative care unit the sister on duty did the monitoring and recorded the results.
Patients were randomized into two groups (each having 25 patients) – Group-D (loading and maintenance of dexmedetomidine infusion) and Group-F (loading and maintenance by fentanyl infusion) on the basis of computer generated random table.
On arrival to operating room IV line was secured and vital parameters were recorded as baseline values which included monitoring of electrocardiography, heart rate, oxygen saturation, end tidal CO2, non-invasive blood pressure. Same parameters were recorded at 1 and 5 min after intubation, before and 1 min after skull clamping, immediately before skin incision and 1 min after skin incision. All patients received standard premedication i.e. inj glycopyrrolate 0.2 mg and inj dexamethasone 8 mg. Mannitol infusion was given in a dose of 0.5-1 gm/kg over 1 h.
Patients in Group-D were given 1 µg/kg of dexmedetomidine as loading dose within 10 min before induction and at the time of induction fentanyl 2 µg/kg was given. For maintenance dexmedetomidine infusion was continued at the rate of 0.04-0.05 µg/kg/min.
Patients in Group-F received 3 µg/kg of fentanyl during induction and for maintenance fentanyl infusion was given at 0.02-0.03 µg/kg/min. In both the groups patients were induced with 5 mg/kg of thiopentone plus 0.1 mg/kg of vecuronium, and maintained with 0.7% isoflurane in a mixture of 60% nitrous oxide and 40% oxygen. Mechanical ventilation was done in both groups with tidal volume of 8-10 ml/kg to keep EtCO2 in the range of 28-32 mmHg. Before skull clamping both groups received fentanyl 1µg/kg and local anesthesia was administered on the skin site to be nailed with 3-5 ml of 2% lignocaine.
Dexmedetomidine and fentanyl infusions were continued until initiation of skin sutures. Inj ketorolac 30 mg IV was given for postoperative analgesia and inj ondansetron 4mg IV for PONV prophylaxis. After completion of sutures anesthetic gas inhalation was stopped. Neuromuscular blockade was reversed with inj glycopyrrolate 0.01mg/kg and inj neostigmine 0.05 mg/kg and all patients were evaluated with Alderete post anesthesia recovery score.
Intraoperatively, the infusion of dexmedetomidine or fentanyl was titrated to keep systemic blood pressure within -20% to +10% from baseline value. Cerebral relaxation score was evaluated by surgeon (1-perfect with no swelling; 2- minimal swelling, 3- substantial swelling but does not require medication; 4- severe swelling, needs medication). The doses of fentanyl and dexmedetomidine as well as use of additional drugs were recorded.
Postoperative monitoring was done in PACU for 24 h with continuous SpO2 and NIBP monitoring, patients were monitored for any postoperative side effects like nausea, vomiting, pain, anxiety or any change in neurological status etc.
STATISTICAL ANALYSIS
After power analysis, performed according to mean arterial pressure, sample size was determined as 25 in the groups assigned for power=0.80, β=0.20 and α=0.05. Continuous data were presented as mean ± SD and analyzed with the help of unpaired Student t-test and the Mann–Whitney U-test. Repeated measures (ABP, HR, etc.) were analyzed by two-way analysis of variance. Categorical data (incidence of complications, VAS, etc.) were presented as the number (frequency) and were analyzed using the χ2 or the Fisher exact test. Data were considered significant if the p-value was less than 0.05. Data were analyzed using the SPSS statistical program (version 20, IBM, USA).
RESULTS
Our study showed both groups were statistically similar in terms of demographic data (age, weight, gender). Preoperative baseline BP, HR, SpO2 values were comparable between the two groups (Table 1).
Table 1: Demographic data
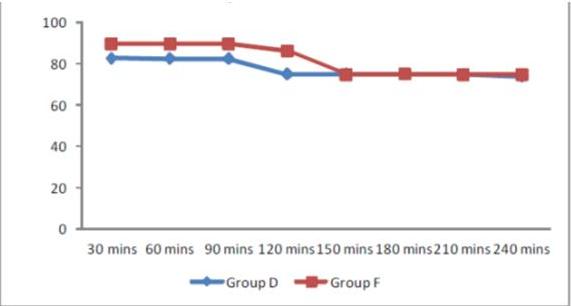
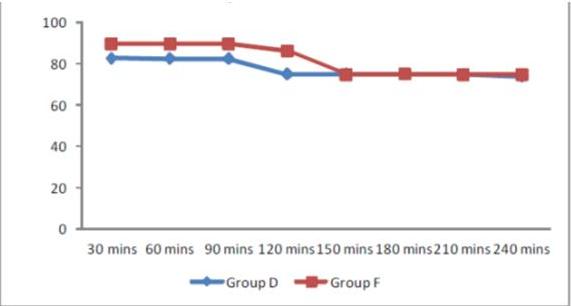
In Group-D and Group-F HR values were increased from baseline at induction and at all observation times especially at time of skull clamping but the values were within physiological limit. Heart rate remained elevated postoperatively and came to baseline after 2 h in Group-F. The rise in HR was significantly less in Group-D as compared to Group-F during all intraoperative observation period, extubation and postoperative till 2 h. SpO2values before and after induction, during perioperative period were similar in two groups (Graph 1).
Graph 1: Intraoperative heart rate
Mean arterial pressure values in Group-D and F were higher than baseline one minute after induction (∆MAP 4.52 in Group-D vs 16.36 in Group-F), laryngoscopy and intubation ((∆MAP 7.92 in Group-D vs 30.08 in Group-F), at skull clamping, skin incision and at various times during intra and postoperative period, and returned to the baseline two hours postoperatively; however, these values were within physiological limits. There was increase in mean arterial pressure at all observations in both the groups; however, the increase was significantly higher in Group-F as compared to Group-D (Table 2).
Table 2: Comparative mean arterial pressure at various stages
Cerebral relaxation score as assessed by the operating surgeon was significantly lower in dexmedetomidine group as compared to fentanyl group (Table 3).
Table 3: Cerebral relaxation score
Our study showed that in Group-D recovery was faster from anesthesia without causing respiratory depression as compared to Group-F; 5.32 min vs. 6.56 min respectively (Table 4).
Table 4: Time for gaining consciousness postoperatively
Dexmedetomidine decreased the total dose of opioid required during intraoperative period; 100 µg in Group-D as compared to 250 µg in Group-F.
In Group-D there were no postoperative complications or side effects like shivering and postoperative nausea or vomiting while In Group-F, 1 patient complained of shivering and 2 patients complained of postoperative nausea and vomiting.
DISCUSSION
Hemodynamic stability is of utmost importance perioperatively in neuroanesthesia. Hypertension may cause increased bleeding or edema. Hypotension on the other hand predispose the patient to cerebral ischemia, because auto regulation of cerebral blood flow is often deranged near tumor or traumatized areas. However, during supratentorial tumor surgery such responses are infrequent.3
Dexmedetomidine has analgesic and opioid sparing effect. It provides hemodynamic stability without respiratory depression.4
In our study two groups were similar in terms of demographic profile and operation time. Baseline preoperative blood pressure, heart rate and SpO2 values were recorded and found to be similar in both groups.
Many previous studies like soliman et al5 and tanskenen et al4 have shown that dexmedetomidine can attenuate sympathetic response of intubation and extubation as also evidenced in our study
Dexmedetomidine attenuates sympathoadrenal stimulation during tracheal intubation but does not completely abolish cardiovascular response.6 In our study also heart rate values increased in both the group from baseline but always within 20% of baseline and physiological limits but dexmedetomidine cause bradycardia and hypotension. In our study 2 patients had bradycardia and one patient had hypotension in dexmedetomidine group but none in fentanyl group. The hemodynamic parameters increased from the baseline in both groups, this may have occurred due to immense surgical stress and various intense stimulations in the intraoperative period. Also in both groups the values returned to the baseline two hours postoperatively may be because the surgical stress was reduced and patients returned to their normal physiological state after one to two hours.
Central sympatholytic effect of dexmedetomidine continued up to the postoperative period. Therefore the extubation was smooth with stable hemodynamics.
We found that the cerebral relaxation scores were significantly lower in Group-D as compared to Group-F indicating superior cerebral relaxation provided by dexmedetomidine due to minimal cerebral swelling caused by decrease in cerebral blood flow. Also decrease in intracranial pressure occurred by inhibiting hypercapneic cerebral vasodilatation and potent cerebral vasoconstriction by dexmedetomidine.7-8 Prielipp et al9 (2002) using PET showed that dexmedetomidine decreased global cerebral blood flow in human; theoretically this reduction in cerebral blood flow may predispose to cerebral ischemia, but animal studies have shown that vasodilatory response to hypoxia is preserved, therefore counteracting the ischemic effect (Takenaka et al7 2000).
Many studies like ours, have reported shorter recovery time from anesthesia with use of dexmedetomidine than fentanyl. Hence the extubation was early in Group-D as compared to Group-F. Dexmedetomidine has minimal adverse effects on respiration10-12 and hence it is being used successfully during weaning and extubation (Shehabi et al11 2004); it also reduces postoperative shivering (Aryan et al13) and patients receiving dexmedetomidine require less antiemetic as in our study. Most common side effect of fentanyl is nausea and vomiting which was found in 2 patients in our group. Only 1 patient in Group-D required atropine 0.5 mg and 2 patients required ephedrine for bradycardia and hypotension respectively.
Limitations of study:
Limited number of patients and use of subjective measure to measure cerebral relaxation instead of real time ICP monitoring.
Future scope of research:
Use of Dexmedetomidine can be evaluated for other neurosurgical procedures like spinal surgeries as alfa 2 receptors are present in dorsal horn of spinal cord. Use of dexmedetomidine can be explored in pediatric neurosurgical procedures.
CONCLUSION
In the present study we have demonstrated that both drugs can be used for neurosurgery, but dexmedetomidine has more stable hemodynamic parameters as compared to fentanyl, during and after anesthesia. Cerebral relaxation scores and emergence from anesthesia are better with dexmedetomidine. Dexmedetomidine provides better operative conditions with minimal cerebral swelling by reducing cerebral blood flow.
Conflict of interest: None declared by the authors
Author contribution:
AG + YD + US – Co-guides
SS – Conducted the study
SM – Helped in study
SMi – Statistical analysis
REFERENCES
1Lecturer; 2Assistant professor; 4Professor; 5PG student
Department of Anesthesiology, Sarojini Naidu Medical College (SNMC), Moti Katra, Agra, Uttar Pradesh 282002, (India)
3Senior resident, Department of Anesthesiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences (SGPGIMS), Rae Bareli Road, Lucknow, Uttar Pradesh 226014, (India)
6Scientist, Division of Biostatistics, National Institute of Occupational Health/ Indian Council of Medical Research; Department of Health Research, Ministry of Health & Family Welfare, Government of India, Meghani Nagar, Ahmedabad (India)
Correspondence: Dr Amrita Gupta, MD, Department of Anesthesiology, Sarojini Naidu Medical College (SNMC), Moti Katra, Agra, Uttar Pradesh 282002, (India)
ABSTRACT
Introduction: Dexmedetomidine provides stable perioperative hemodynamic profile with decreased requirement of opioids. It has neuroprotective effect and may be suitable anesthetic adjuvant when compared to fentanyl.
The main aim of our study was to compare dexmedetomidine and fentanyl in relation to blunting of sympathetic response to intubation and induction while secondary variables were to study their effect on perioperative hemodynamic changes, operative conditions, recovery profile and side effects.
Methodology: In this double blind randomized control trial 50 patients of ASA I and II grade scheduled for elective neurosurgery were selected over a period of 1 year, after obtaining written informed consent. Patients were randomly divided into two groups; in Group-D patient received 1 µg/kg of dexmedetomidine as loading dose within 10 min before induction and 2 µg/kg of fentanyl at induction and 0.04-0.05 µg/kg/min of dexmedetomidine as maintenance during surgery. In Group-F patient received induction with 3 µg/kg of fentanyl and maintained with 0.02-0.03 µg/kg/min of fentanyl.
Hemodynamic changes, cerebral relaxation store, recovery time and intraoperative and postoperative side effects were noted
Results: Baseline heart rate and BP was similar in both the groups. In Group-D and F, Heart rate and BP were increased from baseline during intubation, skull clamping and extubation but were within physiological limits. The rise in heart rate and BP was comparatively lower in Group-D as compared to Group-F. all the values were statistically significant (p < 0.05)
Cerebral relaxation score was lower in Group-D as compared to Group-F, along with faster recovery. During postoperative period there was no shivering nausea and vomiting in Group-D but in Group-F, 1 patient experienced shivering while 2 patients complained of nausea and vomiting.
Conclusion: In our study we found that dexmedetomidine provided better hemodynamic profile as compared to fentanyl with better cerebral relaxation score and recovery time. Hence we conclude that dimetindene is safer and effective alternate to fentanyl as an anesthetic adjuvant in neurosurgery.
Key words: Supratentorial craniotomies; Dexmedetomidine; Fentanyl; Anesthesia, General; Cerebral relaxation score
Citation: Gupta A, MD, Dwivedi Y, Saxena S, Srivastava U, Mangla S, Mishra S. A randomized control study of dexmedetomidine versus fentanyl as an anesthetic adjuvant in supratentorial craniotomies. Anaesth Pain & Intensive Care 2017;21(3): 306-311
Received - 19 Dec 2016; Reviewed – 23 Jan, 8 Mar 2017; Corrected – 26 Jun, 7 Aug 2017; Accepted – 25 Aug 2017
INTRODUCTION
The aim of neuroanesthesia is to protect the brain as much as possible with the means available to the anesthetist. The goals of intraoperative managements are to provide optimal operating conditions, maintain hemodynamic stability, adequate cerebral perfusion pressure, low ICP and to provide cerebral protection and rapid recovery.1 The intense surgical stimulus causes increase in sympathetic activity and marked changes in systemic blood pressure, cerebral blood flow and intracranial pressure. Perioperative hypertension is associated with intracranial bleed while low central blood pressure predisposes the patient to cerebral ischemia. During the intraoperative management these responses should be prevented, attenuated and managed for a favorable outcome.
Various drugs have been used to attenuate these responses especially at the time of intubation and rest of the surgery duration. Fentanyl is one of the most popular and most common drug used for the said purpose. It’s a short acting potent opioid which blunt these sympathetic responses however it is associated with side effects like respiratory depression. Dexmedetomidine is an α2 adrenoceptor agonist, which has sympatholytic, sedative, analgesic, opioid sparing and hemodynamic stabilizing properties without causing significant respiratory depression.2 These properties of dexmedetomidine would be consistent with the important goals of maintaining hemodynamic stability during neurosurgical procedures.
The main aim of our study was to compare dexmedetomidine and fentanyl in relation to blunting of sympathetic response to intubation and induction while secondary variables are to study their effect on perioperative hemodynamic changes, operative conditions, recovery profile and side effects.
METHODOLOGY
After obtaining informed written consent and approval of institutional ethical committee, this randomized double blind study was performed. Inclusion criteria was- ASA I and II patients, age 18 to 65 years, GCS > 12 undergoing supratentorial craniotomy under general anesthesia. The exclusion criteria were; patients with significant systemic disease like uncontrolled hypertension (blood pressure > 140/90), severe respiratory disease such as asthma or ischemic heart disease, alcoholics, drug addicts, psychiatric patients, patients who had taken opioids or benzodiazepines 48 hours prior to surgery, patient with active infection, and patients with BMI > 30 kg/m2.
Our study was double blind in which the resident who was giving the drug was not aware about the drug and in postoperative care unit the sister on duty did the monitoring and recorded the results.
Patients were randomized into two groups (each having 25 patients) – Group-D (loading and maintenance of dexmedetomidine infusion) and Group-F (loading and maintenance by fentanyl infusion) on the basis of computer generated random table.
On arrival to operating room IV line was secured and vital parameters were recorded as baseline values which included monitoring of electrocardiography, heart rate, oxygen saturation, end tidal CO2, non-invasive blood pressure. Same parameters were recorded at 1 and 5 min after intubation, before and 1 min after skull clamping, immediately before skin incision and 1 min after skin incision. All patients received standard premedication i.e. inj glycopyrrolate 0.2 mg and inj dexamethasone 8 mg. Mannitol infusion was given in a dose of 0.5-1 gm/kg over 1 h.
Patients in Group-D were given 1 µg/kg of dexmedetomidine as loading dose within 10 min before induction and at the time of induction fentanyl 2 µg/kg was given. For maintenance dexmedetomidine infusion was continued at the rate of 0.04-0.05 µg/kg/min.
Patients in Group-F received 3 µg/kg of fentanyl during induction and for maintenance fentanyl infusion was given at 0.02-0.03 µg/kg/min. In both the groups patients were induced with 5 mg/kg of thiopentone plus 0.1 mg/kg of vecuronium, and maintained with 0.7% isoflurane in a mixture of 60% nitrous oxide and 40% oxygen. Mechanical ventilation was done in both groups with tidal volume of 8-10 ml/kg to keep EtCO2 in the range of 28-32 mmHg. Before skull clamping both groups received fentanyl 1µg/kg and local anesthesia was administered on the skin site to be nailed with 3-5 ml of 2% lignocaine.
Dexmedetomidine and fentanyl infusions were continued until initiation of skin sutures. Inj ketorolac 30 mg IV was given for postoperative analgesia and inj ondansetron 4mg IV for PONV prophylaxis. After completion of sutures anesthetic gas inhalation was stopped. Neuromuscular blockade was reversed with inj glycopyrrolate 0.01mg/kg and inj neostigmine 0.05 mg/kg and all patients were evaluated with Alderete post anesthesia recovery score.
Intraoperatively, the infusion of dexmedetomidine or fentanyl was titrated to keep systemic blood pressure within -20% to +10% from baseline value. Cerebral relaxation score was evaluated by surgeon (1-perfect with no swelling; 2- minimal swelling, 3- substantial swelling but does not require medication; 4- severe swelling, needs medication). The doses of fentanyl and dexmedetomidine as well as use of additional drugs were recorded.
Postoperative monitoring was done in PACU for 24 h with continuous SpO2 and NIBP monitoring, patients were monitored for any postoperative side effects like nausea, vomiting, pain, anxiety or any change in neurological status etc.
STATISTICAL ANALYSIS
After power analysis, performed according to mean arterial pressure, sample size was determined as 25 in the groups assigned for power=0.80, β=0.20 and α=0.05. Continuous data were presented as mean ± SD and analyzed with the help of unpaired Student t-test and the Mann–Whitney U-test. Repeated measures (ABP, HR, etc.) were analyzed by two-way analysis of variance. Categorical data (incidence of complications, VAS, etc.) were presented as the number (frequency) and were analyzed using the χ2 or the Fisher exact test. Data were considered significant if the p-value was less than 0.05. Data were analyzed using the SPSS statistical program (version 20, IBM, USA).
RESULTS
Our study showed both groups were statistically similar in terms of demographic data (age, weight, gender). Preoperative baseline BP, HR, SpO2 values were comparable between the two groups (Table 1).
Table 1: Demographic data
| Variable | Group-D | Group-F | p-value |
| Age (y) | 42.84 ± 13.825 | 39.72 ± 14.516 | 0.440 |
| Weight (Kg) | 53.20 ± 5.515 | 54.16 ± 6.094 | 0.562 |
| Duration (min) | 105.96 ± 9.533 | 103.52 ± 9.514 | 0.370 |
| Sex M:F | 14:11 | 11:14 | 0.396 |
In Group-D and Group-F HR values were increased from baseline at induction and at all observation times especially at time of skull clamping but the values were within physiological limit. Heart rate remained elevated postoperatively and came to baseline after 2 h in Group-F. The rise in HR was significantly less in Group-D as compared to Group-F during all intraoperative observation period, extubation and postoperative till 2 h. SpO2values before and after induction, during perioperative period were similar in two groups (Graph 1).
Graph 1: Intraoperative heart rate
Mean arterial pressure values in Group-D and F were higher than baseline one minute after induction (∆MAP 4.52 in Group-D vs 16.36 in Group-F), laryngoscopy and intubation ((∆MAP 7.92 in Group-D vs 30.08 in Group-F), at skull clamping, skin incision and at various times during intra and postoperative period, and returned to the baseline two hours postoperatively; however, these values were within physiological limits. There was increase in mean arterial pressure at all observations in both the groups; however, the increase was significantly higher in Group-F as compared to Group-D (Table 2).
Table 2: Comparative mean arterial pressure at various stages
| Time period | Group-D | Group-F | p- value | ||
| Mean ± SD | SE | mean ± SD | SE | ||
| baseline | 88.00 ± 1.683 | 0.337 | 87.76 ±1.715 | 0.343 | 0.858 |
| At induction | 92.52 ± 1.558 | 0.312 | 104.12 ± 2.977 | 0.595 | 0.002 |
| At laryngoscopy and intubation | 95.92 ± 0.997 | 0.199 | 117.84 ± 1.818 | 0.364 | 0.002 |
| At skull clamp | 102.28 ± 1.745 | 0.349 | 119.56 ± 3.330 | 0.666 | 0.002 |
| At skin incision | 97.48 ± 1.873 | 0.375 | 115.96 ± 3.348 | 0.670 | 0.001 |
| At 60 min | 92.60 ± 1.581 | 0.316 | 103.92 ± 3.463 | 0.693 | 0.001 |
| At 120 min | 91.16 ± 1.179 | 0.236 | 106.92 ± 2.842 | 0.568 | 0.001 |
| At extubation | 97.28 ± 1.768 | 0.354 | 115.08 ± 3.068 | 0.614 | 0.002 |
Cerebral relaxation score as assessed by the operating surgeon was significantly lower in dexmedetomidine group as compared to fentanyl group (Table 3).
Table 3: Cerebral relaxation score
| Groups | Frequency | Mean rank | Sum of ranks | Mann-Whitney U test | p-value | |
| Cerebral relaxation score | Group-D | 25 | 14.44 | 361.00 | 36.00 | 0.00 |
| Group-F | 25 | 36.56 | 914.00 | |||
| Total | 50 |
Our study showed that in Group-D recovery was faster from anesthesia without causing respiratory depression as compared to Group-F; 5.32 min vs. 6.56 min respectively (Table 4).
Table 4: Time for gaining consciousness postoperatively
| Time (min) | Group-D | Group-F | p-value | ||
| Mean ± SD | SE | Mean ± SD | SE | ||
| For extubation | 5.32 ± 1.676 | 0.335 | 6.56 ± 1.003 | 0.201 | 0.003 |
| For eye opening | 7.72 ± 2.283 | 0.457 | 8.88 ± 1.453 | 0.291 | 0.037 |
| To respond to verbal command | 8.64 ± 2.234 | 0.447 | 10.24 ± 2.403 | 0.481 | 0.019 |
| To reach ADS 8 | 10.08 ± 1.681 | 0.336 | 11.84 ± 2.427 | 0.485 | 0.005 |
In Group-D there were no postoperative complications or side effects like shivering and postoperative nausea or vomiting while In Group-F, 1 patient complained of shivering and 2 patients complained of postoperative nausea and vomiting.
DISCUSSION
Hemodynamic stability is of utmost importance perioperatively in neuroanesthesia. Hypertension may cause increased bleeding or edema. Hypotension on the other hand predispose the patient to cerebral ischemia, because auto regulation of cerebral blood flow is often deranged near tumor or traumatized areas. However, during supratentorial tumor surgery such responses are infrequent.3
Dexmedetomidine has analgesic and opioid sparing effect. It provides hemodynamic stability without respiratory depression.4
In our study two groups were similar in terms of demographic profile and operation time. Baseline preoperative blood pressure, heart rate and SpO2 values were recorded and found to be similar in both groups.
Many previous studies like soliman et al5 and tanskenen et al4 have shown that dexmedetomidine can attenuate sympathetic response of intubation and extubation as also evidenced in our study
Dexmedetomidine attenuates sympathoadrenal stimulation during tracheal intubation but does not completely abolish cardiovascular response.6 In our study also heart rate values increased in both the group from baseline but always within 20% of baseline and physiological limits but dexmedetomidine cause bradycardia and hypotension. In our study 2 patients had bradycardia and one patient had hypotension in dexmedetomidine group but none in fentanyl group. The hemodynamic parameters increased from the baseline in both groups, this may have occurred due to immense surgical stress and various intense stimulations in the intraoperative period. Also in both groups the values returned to the baseline two hours postoperatively may be because the surgical stress was reduced and patients returned to their normal physiological state after one to two hours.
Central sympatholytic effect of dexmedetomidine continued up to the postoperative period. Therefore the extubation was smooth with stable hemodynamics.
We found that the cerebral relaxation scores were significantly lower in Group-D as compared to Group-F indicating superior cerebral relaxation provided by dexmedetomidine due to minimal cerebral swelling caused by decrease in cerebral blood flow. Also decrease in intracranial pressure occurred by inhibiting hypercapneic cerebral vasodilatation and potent cerebral vasoconstriction by dexmedetomidine.7-8 Prielipp et al9 (2002) using PET showed that dexmedetomidine decreased global cerebral blood flow in human; theoretically this reduction in cerebral blood flow may predispose to cerebral ischemia, but animal studies have shown that vasodilatory response to hypoxia is preserved, therefore counteracting the ischemic effect (Takenaka et al7 2000).
Many studies like ours, have reported shorter recovery time from anesthesia with use of dexmedetomidine than fentanyl. Hence the extubation was early in Group-D as compared to Group-F. Dexmedetomidine has minimal adverse effects on respiration10-12 and hence it is being used successfully during weaning and extubation (Shehabi et al11 2004); it also reduces postoperative shivering (Aryan et al13) and patients receiving dexmedetomidine require less antiemetic as in our study. Most common side effect of fentanyl is nausea and vomiting which was found in 2 patients in our group. Only 1 patient in Group-D required atropine 0.5 mg and 2 patients required ephedrine for bradycardia and hypotension respectively.
Limitations of study:
Limited number of patients and use of subjective measure to measure cerebral relaxation instead of real time ICP monitoring.
Future scope of research:
Use of Dexmedetomidine can be evaluated for other neurosurgical procedures like spinal surgeries as alfa 2 receptors are present in dorsal horn of spinal cord. Use of dexmedetomidine can be explored in pediatric neurosurgical procedures.
CONCLUSION
In the present study we have demonstrated that both drugs can be used for neurosurgery, but dexmedetomidine has more stable hemodynamic parameters as compared to fentanyl, during and after anesthesia. Cerebral relaxation scores and emergence from anesthesia are better with dexmedetomidine. Dexmedetomidine provides better operative conditions with minimal cerebral swelling by reducing cerebral blood flow.
Conflict of interest: None declared by the authors
Author contribution:
AG + YD + US – Co-guides
SS – Conducted the study
SM – Helped in study
SMi – Statistical analysis
REFERENCES
- Everette LL, van Rooyan IF, Warner MH, Shurtleff HA, Saneto RP, Oiemann JG. Relation between dexmedetomidine in awake craniotomy in adolescent: report of 2 cases. Paediatr Anaesth. 2016 Mar;16(3):338-42. [PubMed]
- Talke P, Li J, Jain U, Leung J, Drasner K, Hollenberg M, et al. Effects of perioperative dexmedetomidine infusion in patients undergoing vascular surgery. The study of Perioperative Ischemia Research Group. Anesthesiology. 1995 Mar;82(3):620–3. [PubMed] [Free full text]
- Fieschi C, Agnoli A, Battistini N, Bozzao L, Prencipe M. Derangement of regional cerebral blood flow and of its regulatory mechanisms in acute cerebrovascular lesions. Neurology. 1968;18:1166–79. [PubMed]
- P.E. Tanskanen, Kytta JV, Randell TT, Aantaa RE. dexmedetomidine as an anaesthetic adjuvant in patients undergoing intracranial tumor surgery: a double blind, randomized and placebo controlled study. Br J Anesth. 2006 Nov;97(5):658-65. [PubMed] [Free full text]
- Soliman RN, Hasan AR, Rashwan AM, Omer AM . Prospective randomized controlled study to assess the role of dexmedetomidine in patients with supratentorial tumors undergoing craniotomy under general anesthesia. Middle East J Anesthesiol. 2011 Feb;21(1):23-33. [PubMed]
- Scheinin B, Lindgren L, Randell T, Scheinin H, Scheinin M. Dexmedetomidine attenuates sympathoadrenal responses to tracheal intubation and reduces the need for thiopentone and peroperative fentanyl. Br J Anaesth. 1992 Feb;68(2):126–31. [PubMed]
- Takenaka M, Iida H, Iida M, Dohi S. Intrathecal dexmedetomidine attenuates hypercapnic but not hypoxic cerebral vasodilation in anesthetized rabbits. Anesthesiology. 2000 May;92(5):1376–84. [PubMed] [Free full text]
- Ard JL Jr., Bekker AY, Doyle WK. Dexmedetomidine in awake craniotomy: a technical note. Surg Neurol. 2005 Feb;63(2):114-6. [PubMed]
- Prielipp RC, Wall MH, Tobin JR, Groban L, Cannon MA, Fahey FH, et al. Dexmedetomidine induced sedation in volunteers decreases regional and global cerebral blood flow. Anesth Analg. 2002 Oct;95(4):1052–9. [PubMed] [Free full text]
- Ebert TJ, Hall JE, Barney JA, Uhrich TD, Colinco MD. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000 Aug;93(2):382–94. [PubMed] [Free full text]
- Shehabi Y, Ruettimann U, Adamson H, Innes R, Ickeringill M. Dexmedetomidine infusion for more than 24 hours in critically ill patients: sedative and cardiovascular effects. Intensive Care Med. 2004 Dec;30(12):2188–96.[PubMed] .
- Hall JE, Uhrich TD, Barney JA, Shahbaz RA, Ebert TJ. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000 Mar;90(3):699–705. [PubMed]
- Aryan HE, Box KW Ibrahim D, Desiraiu U, Ames CP. Safety and efficacy of dexmedetomidine in neurosurgical patients. Brain Inj. 2006 Jul;20(8):791-8. [PubMed]