Kjetil Larsen
Corrective Exercise Specialist, Training & Rehabilitation, Eikenga 4, 0579 OSLO (Norway)
Correspondence: Kjetil Larsen, Sandakerveien 22E, 0473 OSLO, Norway; Phone: +47 975 45 192; E-mail: Kjetil@treningogrehab.no
ABSTRACT
The pathophysiology of low back pain (LBP) is considered to be unknown. However, a strong pattern of biomechanical factors points us to the most likely cause of LBP. It is well known that the utmost majority of disc herniations, protrude posteriorly or posterolaterally, and it is widely accepted that this is caused by spinal flexion. It is also known that so-called neutrally lordotic spinal segments, i.e. the cervical and lumbosacral segments, are much more susceptible to these injuries, as up to 95% of disc pathology occur in the low cervical and lumbar levels. The literature also shows that reduced lumbosacral angles are a significant tendency in these patients. Further, many studies show atrophy of the extensor musculature in LBP sufferers. The intervertebral discs are richly innervated and may, like most other structures, yield warning signs which lead to pain generation when exposed to noxious stimulus such as anterior compressive forces, compatible with the above-mentioned factors. Based on the biomechanical evidence and the statistics, a postural cause of LBP, namely habitual lumbopelvic flexion (LPF), is very likely. Postural LPF is treatable, and a suggested approach for identification and intervention has been included in this paper.
Citation: Larsen K. Common low back pain, is it really a mystery? Anaesth Pain & Intensive Care 2018;22(1):125-130
Keywords: Low back pain; Discogenic pain; Biomechanics; Pathophysiology; Spinal morphology
Received; 6 March 2018; Reviewed 6 March 2018; Corrected 10 March 2018; Accepted 26 March 2018
INTRODUCTION
Lower back pain has become a plague of the modern society.1 It is estimated that it is one of the most common causes of sick-leave and is thus causing a great financial burden upon society.2 Not making things easier, research is quite conflicted, and etiological consensus has not even remotely been reached; in fact, the World Health Organization states that a staggering 85% of all LBP is considered idiopathic.3 It is troubling and perhaps a paradox that modern medicine can perform brain surgery but is not able to resolve a seemingly simple issue such as low back pain, especially considered the massive amount of research that has been done in this regard.
Despite the above, a lot of evidence does point us to the most likely cause of LBP, if one is willing to follow the red thread. It is my experience that LBP has an obvious common denominator, and also often a relatively simple solution.
Granted, this paper presumes that one accepts the notion that excessive disc compression may lead to pain. The spinal discs are richly innervated, mainly by the sympathetic nervous system4-6 (Figure 1), and may of course generate warning signals if irritated. Just like a paper cut is highly likely to cause a certain degree of pain, surely irritation the spinal discs may as well. This may explain why many experience pain even when no specific pathology is proven upon imaging; warning signals are generated to prevent injury.
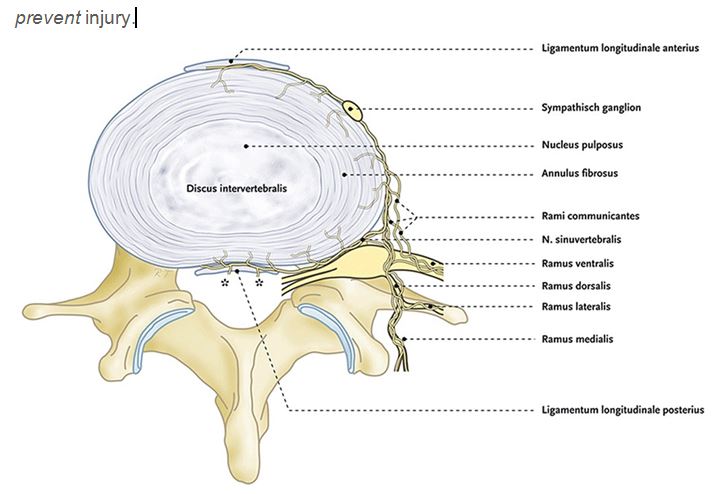
Figure 1: Nerve supply to the vertebrae (Source: Kallewaard et al., 2010)
It has, however, been shown quite clearly that pain is complex and not well understood (e.g. in numerous papers by Moseley and others), and that we may respond differently to noxious input, and I am not disputing this. It is very well known that many imaging findings are asymptomatic, for example. However, it is important to keep in mind that we still need to be able to provide treatment for those who do translate the noxious input into pain. And, although pain education is important in calming the patient down and may somewhat improve their quality of life, it is now being increasingly known that it may not resolve the patient's actual pain perception. In fact, a recent meta-analysis states, and I quote their conclusion: "Evidence suggests that education programs are not recommended in preventing or treating neck pain as well as treating low back pain".7
This should, in my opinion, motivate us to keep looking for a cause for LBP, rather than blaming its majority on psychogenicity. That said, it is interesting to note that flexed postures and introverted personalities have been associated,8 possibly aiding in connecting of certain elements within the bio-psycho-social modalities. What came first, the chicken or the egg?
ETIOLOGY
Several factors have been quite consistently been identified in patients with low back pain. Firstly, let us consider perhaps the most convincing fact; virtually all disc herniations protrude posteriorly or posterolaterally.9 The common denominator is posterior herniation, which has been shown repeatedly to be caused by spinal flexion.10-17 In fact, it has been shown to be caused up to 30 times faster if there is 45° of spinal flexion.18 This mechanism is well known and largely accepted. Moderate to severe disc degeneration and herniations are a much more common finding in LBP than asymptomatic groups, especially those with the two pathologies combined.19
Approximately 95% of disc injuries are also known to occur in the neutrally lordotic regions; the cervical and lumbar spinal segments. Only between 0,5-4% of disc injuries occur at the thoracic spinal segment, which is neutrally kyphotic.10 This implies that neutrally lordotic segments are more sensitive to habitual flexion than neutrally kyphotic segments are.
Further, studies show that reduced lumbar and sacral angles, i.e. reduced extension, are associated with disc injuries and degeneration.19-23 Moreover, disc injuries generally occur in the proximity of the pelvis, at the L4-S1 levels,10 strongly indicating that the lumbopelvic flexion may be the main influencing factor, and not necessarily the lumbar spine in isolation.24-26
Disc pathology has also been associated with lighter but persistent loading patterns, whereas fractures have been associated with higher compressive forces (e.g. trauma).27 This may indicate that repetitive motion and/or continuous (i.e. postural / habitual) loading patterns are present. These, if remained unaltered, may explain why so many patients have recurrent episodes of LBP, as the underlying cause has not been addressed.
Compatible with all of the above, cross-sectional studies show that atrophy of the spinal extensors occur in chronic low back pain patients, namely the multifidi, erector spinae, quadratus lumborum and psoas major muscles.28-33
These factors imply that a lack of spinal extension is the most likely cause of common disc pathology. More specifically, as I perceive it, a lack of postural lumbopelvic extension.
CONTROVERSIES REGARDING POSTURE
Posture and the correction of such has become a very controversial topic the recent years. It has been claimed that the importance of postural correctives have been disproven, and even that it may be detrimental to the patient’s selfesteem.34 However, postural factors may most certainly influence and how the intervertebral discs are loaded, as well as how greatly the spinal extensors engage habitually. Therefore, if one accepts the notion of discogenic pain, considering the wealth of biomechanical evidence with regards to LBP, it would in my opinion be quite unreasonable to disregard posture as a potential cause.
Unfortunately, there are some very important nuances that may easily misguide practitioners when evaluating when treating posture with their patients. It is often claimed that “anterior pelvic tilt”, is a common cause of LBP, but based on the evidence this may almost immediately be disregarded. The reason for this is that extension of the spine would cause anterior herniation of the nucleus, which is very rarely seen. Further, we would probably not see atrophy of the extensor musculature if this was to be true, and especially not a decrease in lumbosacral angles. Anterior pelvic tilt, also known as hyperlordosis can impossibly be a common cause of LBP, the evidence considered. It is my opinion that changing a patient’s pelvic alignment in order to reduce lumbosacral lordosis should be considered iatrogenic, and because this has been done for many years, one may start to understand why so many practitioners have become opponents of postural correctives.
Certainly, corrective strategies must be based on evidence and common sense, not on popular fallacy.
Another common cause of confusion is that these patients tend to have increased pain when going into lumbosacral extension. This is in fact a paradox, and the reason why it occurs is because anterior shearing (caused by flexion), will lead to posterior occurrence of the wound (annular rupture, nuclear protrusion). When going into a more extended lumbopelvic posture, although this will fundamentally resolve the underlying cause of the posterior wound (i.e. the habitual flexion), it will cause compression of the wound and thus also initial exacerbation of pain. This is completely harmless, and it is important to teach the patient that, so that they are not afraid to maintain an extended pelvis. Interestingly, slight flexion will often be perceived by the patient as soothing, but it is my opinion and experience that although soothing, it may be the cause of their problem in the first place.
Moreover, the “neutral zone” has already been discussed many times; however, its specific measurements are not well defined. I believe that the reason for this is faulty pelvic landmark measurements. The posterior superior iliac spine to anterior superior iliac spine ratio (PSIS:ASIS) pelvic measurements (i.e. horizontal alignment of these landmarks) is thought to represent neutral pelvic alignment, but rather it will often flex the lumbosacral spine and thus predispose the patient to injury, as habitual/postural flexion will increase. It is my experience that the most reliable pelvic measurement is to align the pubic symphysis (PS) and anterior superior iliac spine (ASIS) vertically,35,36 being careful not to mistake extension at the thoracolumbar junction (where we rarely see injuries) as lumbosacral extension. It must, however, be mentioned that pelvic morphology may somewhat differ,37 that’s why the patients’ corrective measures should meet several criteria, and not merely the landmark measurements alone.
Further, with regards to so-called spinal neutrality, it has often been said that “If we cannot flex our spines then we will become immobilized”, and “the spine is designed for movement in all directions”, and this is used as an argument against the biomechanical approach to LBP. I think these are good, but somewhat unauthenticated statements. The problem is not to bend down to tie your shoes or pick up the kids, but rather to be situated in a constantly flexed posture. Moreover, if the spine was designed to do whatever we wanted to, so many people would not be struggling with recurrent LBP. Doubtlessly there is room for improvement.
Sensitization has also been offered as a potential explanation for chronic pain, however it is not reasonable to expect long lasting changes in pain levels if the proper intervention has not been implemented. May the wound on your finger heal if you keep cutting it? – Can the spine heal if it is continuously misloaded? Controversial, yes, but in my experience the reality.
PELVIC MEASUREMENTS IN PRACTICE
In the image below it is easy to see that the pubic symphysis is far anterior to the ASIS. This would then imply that the patient is in the notorious posterior pelvic tilt (PPT). PPT fits well as a common cause of back pain, because it is compatible with all of the biomechanical studies cited in the etiology section (Figure 2). PPT will cause continuous flexion of the lumbosacral spine, thus also a decreased lumbar and sacral angle, potentially excessive compression the anterior intervertebral disc, and disengagement of the lumbosacral extensors (as they are antagonistic of lumbosacral flexion – also offering an explanation of why they atrophy in these patients).
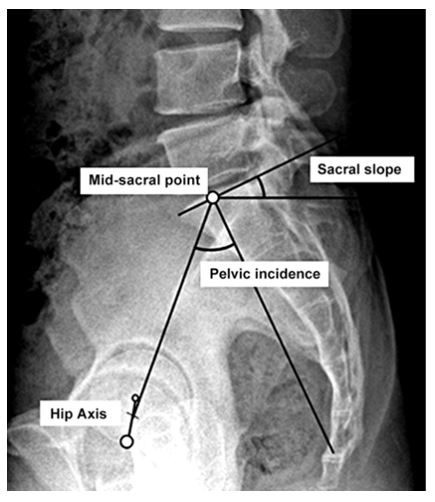
Figure 2: Pelvic axes in relation to midsacral point; Source: Lee et al., 201226
In practice, the patient will present with a completely flat lumbosacral spinal segment. They may or may not be extended through the thoracolumbar junction (i.e. swayback posture, which is usually misinterpreted as anterior pelvic tilt), but the LS will be flexed and will look flat, which is usually confirmable by kneeling by the side of the patient (patient will be standing during the assessment) and measuring the vertical alignment between the given landmarks (PS:ASIS vertically), where the PS will be most likely be found anterior to the ASIS. Upon palpation of the lumbosacral erector spinae, asymmetry will usually be seen from, and caudal to the L4 level. Commonly the LS erectors will be soft and disengaged in this area, and there may also be swelling and/or connective tissue densification.38
In the image below (Figure 3), a male subject with conspicuous flat-back posture and posterior pelvic tilt is seen. This is a quite common structural presentation. Pay notice of the angle of the pelvis (i.e. the gluteal apex), as it is pointing obliquely caudally. It should point gently upward when the PS and ASIS are aligned, thus being much more extended than generally believed to be neutral, when in proper position.
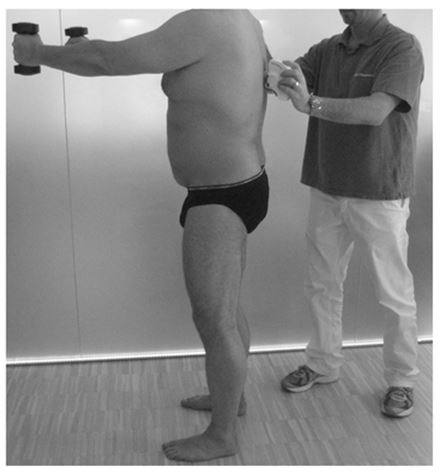
Figure 3: A typical flat-back posture and posterior pelvic tilt seen in a patient with LBP (Source: Hildebrandt et al., 2017)
This problem may be remedied by cueing the patient to relax their abdominals, and rather extend the pelvis until the PS and ASIS are vertical, the gluteal apex is angled gently up, and the lumbosacral erectors are palpably active in standing posture. The patient will feel that he or she is now required to use these muscles, often confirming that they were not used previously. This may be considered a permanent change, not an exercise.
To supplement this change, exercises may be prescribed for the erector spinae, multifidii, quadratus lumborum and psoas major muscles.
CONCLUSION
Based on the evidence, a strong biomechanical influence in the pathogenesis of LBP is indisputable, and it is my opinion that it must be recognized. Based on the evidence it cannot be claimed that a postural/biomechanical cause of LBP has been disproven, as the evidence is clearly compatible with these factors. It is, however, more or less disproven that excessive lordosis is a common cause of LBP; there is very little evidence to suggest this.
Whether or not discogenic pain is real may remain controversial for now. If one, however, accepts discogenic pain as factual, then certainly the evidence indicates flexion as the most probable cause of LBP. It is the author’s experience that LBP may be relieved by increasing postural / habitual lumbopelvic extension.
Conflict of interest: None declared by the author
REFERENCES
Corrective Exercise Specialist, Training & Rehabilitation, Eikenga 4, 0579 OSLO (Norway)
Correspondence: Kjetil Larsen, Sandakerveien 22E, 0473 OSLO, Norway; Phone: +47 975 45 192; E-mail: Kjetil@treningogrehab.no
ABSTRACT
The pathophysiology of low back pain (LBP) is considered to be unknown. However, a strong pattern of biomechanical factors points us to the most likely cause of LBP. It is well known that the utmost majority of disc herniations, protrude posteriorly or posterolaterally, and it is widely accepted that this is caused by spinal flexion. It is also known that so-called neutrally lordotic spinal segments, i.e. the cervical and lumbosacral segments, are much more susceptible to these injuries, as up to 95% of disc pathology occur in the low cervical and lumbar levels. The literature also shows that reduced lumbosacral angles are a significant tendency in these patients. Further, many studies show atrophy of the extensor musculature in LBP sufferers. The intervertebral discs are richly innervated and may, like most other structures, yield warning signs which lead to pain generation when exposed to noxious stimulus such as anterior compressive forces, compatible with the above-mentioned factors. Based on the biomechanical evidence and the statistics, a postural cause of LBP, namely habitual lumbopelvic flexion (LPF), is very likely. Postural LPF is treatable, and a suggested approach for identification and intervention has been included in this paper.
Citation: Larsen K. Common low back pain, is it really a mystery? Anaesth Pain & Intensive Care 2018;22(1):125-130
Keywords: Low back pain; Discogenic pain; Biomechanics; Pathophysiology; Spinal morphology
Received; 6 March 2018; Reviewed 6 March 2018; Corrected 10 March 2018; Accepted 26 March 2018
INTRODUCTION
Lower back pain has become a plague of the modern society.1 It is estimated that it is one of the most common causes of sick-leave and is thus causing a great financial burden upon society.2 Not making things easier, research is quite conflicted, and etiological consensus has not even remotely been reached; in fact, the World Health Organization states that a staggering 85% of all LBP is considered idiopathic.3 It is troubling and perhaps a paradox that modern medicine can perform brain surgery but is not able to resolve a seemingly simple issue such as low back pain, especially considered the massive amount of research that has been done in this regard.
Despite the above, a lot of evidence does point us to the most likely cause of LBP, if one is willing to follow the red thread. It is my experience that LBP has an obvious common denominator, and also often a relatively simple solution.
Granted, this paper presumes that one accepts the notion that excessive disc compression may lead to pain. The spinal discs are richly innervated, mainly by the sympathetic nervous system4-6 (Figure 1), and may of course generate warning signals if irritated. Just like a paper cut is highly likely to cause a certain degree of pain, surely irritation the spinal discs may as well. This may explain why many experience pain even when no specific pathology is proven upon imaging; warning signals are generated to prevent injury.
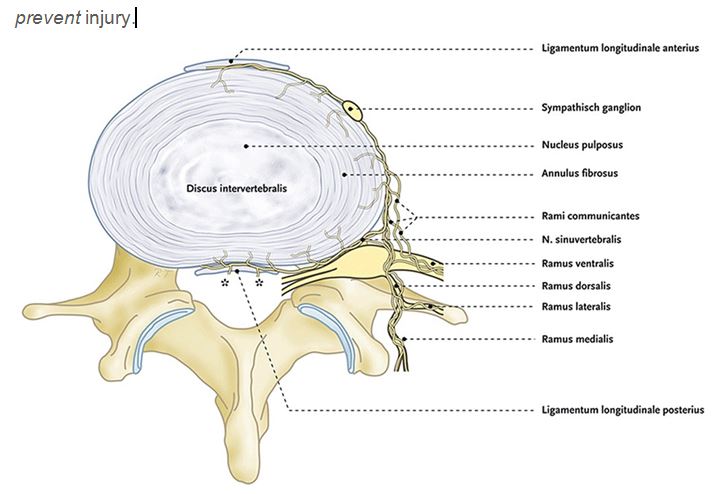
Figure 1: Nerve supply to the vertebrae (Source: Kallewaard et al., 2010)
It has, however, been shown quite clearly that pain is complex and not well understood (e.g. in numerous papers by Moseley and others), and that we may respond differently to noxious input, and I am not disputing this. It is very well known that many imaging findings are asymptomatic, for example. However, it is important to keep in mind that we still need to be able to provide treatment for those who do translate the noxious input into pain. And, although pain education is important in calming the patient down and may somewhat improve their quality of life, it is now being increasingly known that it may not resolve the patient's actual pain perception. In fact, a recent meta-analysis states, and I quote their conclusion: "Evidence suggests that education programs are not recommended in preventing or treating neck pain as well as treating low back pain".7
This should, in my opinion, motivate us to keep looking for a cause for LBP, rather than blaming its majority on psychogenicity. That said, it is interesting to note that flexed postures and introverted personalities have been associated,8 possibly aiding in connecting of certain elements within the bio-psycho-social modalities. What came first, the chicken or the egg?
ETIOLOGY
Several factors have been quite consistently been identified in patients with low back pain. Firstly, let us consider perhaps the most convincing fact; virtually all disc herniations protrude posteriorly or posterolaterally.9 The common denominator is posterior herniation, which has been shown repeatedly to be caused by spinal flexion.10-17 In fact, it has been shown to be caused up to 30 times faster if there is 45° of spinal flexion.18 This mechanism is well known and largely accepted. Moderate to severe disc degeneration and herniations are a much more common finding in LBP than asymptomatic groups, especially those with the two pathologies combined.19
Approximately 95% of disc injuries are also known to occur in the neutrally lordotic regions; the cervical and lumbar spinal segments. Only between 0,5-4% of disc injuries occur at the thoracic spinal segment, which is neutrally kyphotic.10 This implies that neutrally lordotic segments are more sensitive to habitual flexion than neutrally kyphotic segments are.
Further, studies show that reduced lumbar and sacral angles, i.e. reduced extension, are associated with disc injuries and degeneration.19-23 Moreover, disc injuries generally occur in the proximity of the pelvis, at the L4-S1 levels,10 strongly indicating that the lumbopelvic flexion may be the main influencing factor, and not necessarily the lumbar spine in isolation.24-26
Disc pathology has also been associated with lighter but persistent loading patterns, whereas fractures have been associated with higher compressive forces (e.g. trauma).27 This may indicate that repetitive motion and/or continuous (i.e. postural / habitual) loading patterns are present. These, if remained unaltered, may explain why so many patients have recurrent episodes of LBP, as the underlying cause has not been addressed.
Compatible with all of the above, cross-sectional studies show that atrophy of the spinal extensors occur in chronic low back pain patients, namely the multifidi, erector spinae, quadratus lumborum and psoas major muscles.28-33
These factors imply that a lack of spinal extension is the most likely cause of common disc pathology. More specifically, as I perceive it, a lack of postural lumbopelvic extension.
CONTROVERSIES REGARDING POSTURE
Posture and the correction of such has become a very controversial topic the recent years. It has been claimed that the importance of postural correctives have been disproven, and even that it may be detrimental to the patient’s selfesteem.34 However, postural factors may most certainly influence and how the intervertebral discs are loaded, as well as how greatly the spinal extensors engage habitually. Therefore, if one accepts the notion of discogenic pain, considering the wealth of biomechanical evidence with regards to LBP, it would in my opinion be quite unreasonable to disregard posture as a potential cause.
Unfortunately, there are some very important nuances that may easily misguide practitioners when evaluating when treating posture with their patients. It is often claimed that “anterior pelvic tilt”, is a common cause of LBP, but based on the evidence this may almost immediately be disregarded. The reason for this is that extension of the spine would cause anterior herniation of the nucleus, which is very rarely seen. Further, we would probably not see atrophy of the extensor musculature if this was to be true, and especially not a decrease in lumbosacral angles. Anterior pelvic tilt, also known as hyperlordosis can impossibly be a common cause of LBP, the evidence considered. It is my opinion that changing a patient’s pelvic alignment in order to reduce lumbosacral lordosis should be considered iatrogenic, and because this has been done for many years, one may start to understand why so many practitioners have become opponents of postural correctives.
Certainly, corrective strategies must be based on evidence and common sense, not on popular fallacy.
Another common cause of confusion is that these patients tend to have increased pain when going into lumbosacral extension. This is in fact a paradox, and the reason why it occurs is because anterior shearing (caused by flexion), will lead to posterior occurrence of the wound (annular rupture, nuclear protrusion). When going into a more extended lumbopelvic posture, although this will fundamentally resolve the underlying cause of the posterior wound (i.e. the habitual flexion), it will cause compression of the wound and thus also initial exacerbation of pain. This is completely harmless, and it is important to teach the patient that, so that they are not afraid to maintain an extended pelvis. Interestingly, slight flexion will often be perceived by the patient as soothing, but it is my opinion and experience that although soothing, it may be the cause of their problem in the first place.
Moreover, the “neutral zone” has already been discussed many times; however, its specific measurements are not well defined. I believe that the reason for this is faulty pelvic landmark measurements. The posterior superior iliac spine to anterior superior iliac spine ratio (PSIS:ASIS) pelvic measurements (i.e. horizontal alignment of these landmarks) is thought to represent neutral pelvic alignment, but rather it will often flex the lumbosacral spine and thus predispose the patient to injury, as habitual/postural flexion will increase. It is my experience that the most reliable pelvic measurement is to align the pubic symphysis (PS) and anterior superior iliac spine (ASIS) vertically,35,36 being careful not to mistake extension at the thoracolumbar junction (where we rarely see injuries) as lumbosacral extension. It must, however, be mentioned that pelvic morphology may somewhat differ,37 that’s why the patients’ corrective measures should meet several criteria, and not merely the landmark measurements alone.
Further, with regards to so-called spinal neutrality, it has often been said that “If we cannot flex our spines then we will become immobilized”, and “the spine is designed for movement in all directions”, and this is used as an argument against the biomechanical approach to LBP. I think these are good, but somewhat unauthenticated statements. The problem is not to bend down to tie your shoes or pick up the kids, but rather to be situated in a constantly flexed posture. Moreover, if the spine was designed to do whatever we wanted to, so many people would not be struggling with recurrent LBP. Doubtlessly there is room for improvement.
Sensitization has also been offered as a potential explanation for chronic pain, however it is not reasonable to expect long lasting changes in pain levels if the proper intervention has not been implemented. May the wound on your finger heal if you keep cutting it? – Can the spine heal if it is continuously misloaded? Controversial, yes, but in my experience the reality.
PELVIC MEASUREMENTS IN PRACTICE
In the image below it is easy to see that the pubic symphysis is far anterior to the ASIS. This would then imply that the patient is in the notorious posterior pelvic tilt (PPT). PPT fits well as a common cause of back pain, because it is compatible with all of the biomechanical studies cited in the etiology section (Figure 2). PPT will cause continuous flexion of the lumbosacral spine, thus also a decreased lumbar and sacral angle, potentially excessive compression the anterior intervertebral disc, and disengagement of the lumbosacral extensors (as they are antagonistic of lumbosacral flexion – also offering an explanation of why they atrophy in these patients).
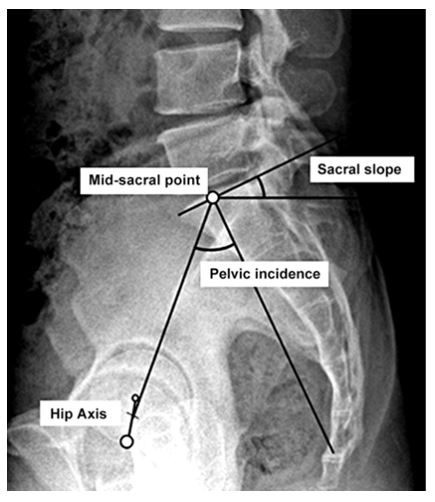
Figure 2: Pelvic axes in relation to midsacral point; Source: Lee et al., 201226
In practice, the patient will present with a completely flat lumbosacral spinal segment. They may or may not be extended through the thoracolumbar junction (i.e. swayback posture, which is usually misinterpreted as anterior pelvic tilt), but the LS will be flexed and will look flat, which is usually confirmable by kneeling by the side of the patient (patient will be standing during the assessment) and measuring the vertical alignment between the given landmarks (PS:ASIS vertically), where the PS will be most likely be found anterior to the ASIS. Upon palpation of the lumbosacral erector spinae, asymmetry will usually be seen from, and caudal to the L4 level. Commonly the LS erectors will be soft and disengaged in this area, and there may also be swelling and/or connective tissue densification.38
In the image below (Figure 3), a male subject with conspicuous flat-back posture and posterior pelvic tilt is seen. This is a quite common structural presentation. Pay notice of the angle of the pelvis (i.e. the gluteal apex), as it is pointing obliquely caudally. It should point gently upward when the PS and ASIS are aligned, thus being much more extended than generally believed to be neutral, when in proper position.
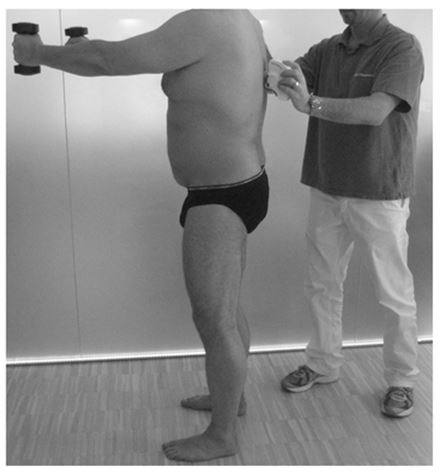
Figure 3: A typical flat-back posture and posterior pelvic tilt seen in a patient with LBP (Source: Hildebrandt et al., 2017)
This problem may be remedied by cueing the patient to relax their abdominals, and rather extend the pelvis until the PS and ASIS are vertical, the gluteal apex is angled gently up, and the lumbosacral erectors are palpably active in standing posture. The patient will feel that he or she is now required to use these muscles, often confirming that they were not used previously. This may be considered a permanent change, not an exercise.
To supplement this change, exercises may be prescribed for the erector spinae, multifidii, quadratus lumborum and psoas major muscles.
CONCLUSION
Based on the evidence, a strong biomechanical influence in the pathogenesis of LBP is indisputable, and it is my opinion that it must be recognized. Based on the evidence it cannot be claimed that a postural/biomechanical cause of LBP has been disproven, as the evidence is clearly compatible with these factors. It is, however, more or less disproven that excessive lordosis is a common cause of LBP; there is very little evidence to suggest this.
Whether or not discogenic pain is real may remain controversial for now. If one, however, accepts discogenic pain as factual, then certainly the evidence indicates flexion as the most probable cause of LBP. It is the author’s experience that LBP may be relieved by increasing postural / habitual lumbopelvic extension.
Conflict of interest: None declared by the author
REFERENCES
- Hoy D, Brooks P, Blyth F, Buchbinder R. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010 Dec;24(6):769-81.doi: 10.1016/j.berh.2010.10.002[PubMed]
- Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, Williams G, Smith E, Vos T, Barendregt J, Murray C, Burstein R, Buchbinder R.The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014 Jun;73(6):968-74. doi: 10.1136/annrheumdis-2013-204428. Epub 2014 Mar 24[PubMed][Free full text]
- Chronic diseases and health promotion: http://www.who.int/chp/topics/rheumatic/en/
- Bogduk N, Tynan W, Wilson AS. The nerve supply to the human lumbar intervertebral discs. J Anat. 1981 Jan;132(Pt 1):39-56.[PubMed][Free full text]
- Bogduk N.The innervation of the vertebral column. Aust J Physiother. 1985;31(3):89-94. doi: 10.1016/S0004-9514(14)60626-7. Epub 2014 Mar 27[PubMed][Free full text]
- Edgar MA. The nerve supply of the lumbar intervertebral disc. J Bone Joint Surg Br. 2007 Sep;89(9):1135-9.[PubMed][Free full text]
- Ainpradub K, Sitthipornvorakul E, Janwantanakul P, van der Beek AJ.Effect of education on non-specific neck and low back pain: A meta-analysis of randomized controlled trials. Man Ther. 2016 Apr;22:31-41. doi:10.1016/j.math.2015.10.012. Epub 2015 Nov 2.[PubMed]
- Sylvain Guimond, Wael Massrieh. Intricate Correlation between Body Posture, Personality Trait and Incidence of Body Pain: A Cross-Referential Study Report. 10.1371/journal.pone.0037450 PMCID: PMC3356261[PubMed][Free full text]
- Gerald L. Burke. Backache: From occiput to coccyx. E.G. Macdonald, 1964
- Keith L. Moore, 2007, «Essential clinical anatomy, 3rd
- Marshall LW, McGill SM. The role of axial torque in disc herniation. Clin Biomech (Bristol, Avon). 2010 Jan;25(1):6-9. doi:10.1016/j.clinbiomech.2009.09.003[PubMed]
- Veres SP, Robertson PA, Broom ND. The morphology of acute disc herniation: a clinically relevant model defining the role of flexion. Spine (Phila Pa 1976). 2009 Oct 1;34(21):2288-96. doi: 10.1097/BRS.0b013e3181a49d7e. [PubMed]
- McGill SM, Hughson RL, Parks K. Changes in lumbar lordosis modify the role of the extensor muscles. Clin Biomech (Bristol, Avon). 2000 Dec;15(10):777-80[PubMed]
- Aultman CD, Scannell J, McGill SM. The direction of progressive herniation in porcine spine motion segments is influenced by the orientation of the bending axis. Clin Biomech (Bristol, Avon). 2005 Feb;20(2):126-9.[PubMed]
- Tampier C, Drake JD, Callaghan JP, McGill SM. Progressive disc herniation: an investigation of the mechanism using radiologic, histochemical, and microscopic dissection techniques on a porcine model. Spine (Phila Pa 1976). 2007 Dec 1;32(25):2869-74. doi: 10.1097/BRS.0b013e31815b64f5. [PubMed]
- Wade KR, Robertson PA, Thambyah A, Broom ND. How healthy discs herniate: a biomechanical and microstructural study investigating the combined effects of compression rate and flexion. Spine (Phila Pa 1976). 2014 Jun 1;39(13):1018-28. doi: 10.1097/BRS.0000000000000262.[PubMed]
- Potvin JR, McGill SM, Norman RW. Trunk muscle and lumbar ligament contributions to dynamic lifts with varying degrees of trunk flexion. Spine (Phila Pa 1976). 1991 Sep;16(9):1099-107.[PubMed]
- Gallagher S, Marras WS, Litsky AS, Burr D. Torso flexion loads and the fatigue failure of human lumbosacral motion segments. Spine (Phila Pa 1976). 2005 Oct 15;30(20):2265-73.[PubMed]
- Keith L. Moore, 2007, «Essential clinical anatomy, 3rd
- Rajnics P, Templier A, Skalli W, Lavaste F, Illes T. The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop. 2002;26(2):104-8[PubMed][Free full text]
- Ergün T, Lakadamyalı H, Sahin MS. The relation between sagittal morphology of the lumbosacral spine and the degree of lumbar intervertebral disc degeneration. Acta Orthop Traumatol Turc. 2010;44(4):293-9.doi:10.3944/AOTT.2010.2375[PubMed]
- Skaf GS, Ayoub CM, Domloj NT, Turbay MJ, El-Zein C, Hourani MH. Effect of age and lordotic angle on the level of lumbar disc herniation. Adv Orthop. 2011;2011:950576. doi: 10.4061/2011/950576. Epub 2011 Sep 7. [PubMed][Free full text]
- Chun SW, Lim CY, Kim K, Hwang J, Chung SG. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J. 2017 Aug;17(8):1180-1191. doi: 10.1016/j.spinee.2017.04.034. Epub 2017 May 2.[PubMed]
- Vleeming A, Schuenke MD, Masi AT, Carreiro JE, Danneels L, Willard FH. The sacroiliac joint: an overview of its anatomy, function and potential clinical implications. J Anat. 2012 Dec; 221(6): 537–567. doi: 10.1111/j.1469-7580.2012.01564.x PMCID: PMC3512279[PubMed][Free full text]
- Amonoo-Kuofi HS. Changes in the lumbosacral angle, sacral inclination and the curvature of the lumbar spine during aging. Acta Anat (Basel). 1992;145(4):373-7[PubMed]
- Lee CS, Chung SS, Park SJ, Cho KH, Shin SK. The Association of Lumbosacral Sagittal Alignments and the Patterns of Lumbar Disc Degeneration. J Korean Soc Spine Surg. 2012 Dec;19(4):145-151.[Free full text]https://doi.org/10.4184/jkss.2012.19.4.145
- Parkinson RJ, Callaghan JP. The role of dynamic flexion in spine injury is altered by increasing dynamic load magnitude. Clin Biomech (Bristol, Avon). 2009 Feb;24(2):148-54. doi: 10.1016/j.clinbiomech.2008.11.007. Epub 2009 Jan 3[PubMed]
- Dangaria TR, Naesh O. Changes in cross-sectional area of psoas major muscle in unilateral sciatica caused by disc herniation. Spine (Phila Pa 1976). 1998 Apr 15;23(8):928-31.[PubMed]
- Barker KL, Shamley DR, Jackson D. Changes in the cross-sectional area of multifidus and psoas in patients with unilateral back pain: the relationship to pain and disability. Spine (Phila Pa 1976). 2004 Nov 15;29(22):E515-9. [PubMed]
- Freeman MD, Woodham MA, Woodham AW. The role of the lumbar multifidus in chronic low back pain: a review. PMR. 2010 Feb;2(2):142-6. doi: 10.1016/j.pmrj.2009.11.006.[PubMed]
- Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol. 2000 Feb;55(2):145-9.[PubMed]
- Cooper RG1, St Clair Forbes W, Jayson MI. Radiographic demonstration of paraspinal muscle wasting in patients with chronic low back pain. Br J Rheumatol. 1992 Jun;31(6):389-94.[PubMed]
- Parkkola R, Rytökoski U, Kormano M. Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects. Spine (Phila Pa 1976). 1993 Jun 1;18(7):830-6.[PubMed]
- Lederman E. The fall of the postural-structural-biomechanical model in manual and physical therapies: exemplified by lower back pain. J Bodyw Mov Ther. 2011 Apr;15(2):131-8. doi: 10.1016/j.jbmt.2011.01.011.[PubMed]
- Evan Osar, 2012, Corrective Exercise Solutions to Common Hip and Shoulder Dysfunction 1st Edition.
- Kendall FP, McCreary EK. Muscles, Testing and Function. 3rd ed. Baltimore: Williams and Wilkins; 1983.
- Preece SJ, Willan P, Nester CJ, Graham-Smith P, Herrington L, and Bowker P. Variation in Pelvic Morphology May Prevent the Identification of Anterior Pelvic Tilt. J Man Manip Ther. 2008;16(2):113–117. doi: 10.1179/106698108790818459[PubMed][Free full text]
- Langevin HM, Stevens-Tuttle D, Fox JR, Badger GJ, Bouffard NA, Krag MH, Wu J, et al. Ultrasound evidence of altered lumbar connective tissue structure in human subjects with chronic low back pain. BMC Musculoskelet Disord. 2009 Dec 3;10:151. doi: 10.1186/1471-2474-10-151.[PubMed][Free full text]
- Yang H, Liu H, Li Z, Zhang K, Wang J, Wang H, and Zheng Z. Low back pain associated with lumbar disc herniation: role of moderately degenerative disc and annulus fibrous tears. Int J Clin Exp Med. 2015; 8(2): 1634–1644. [PubMed][Freefull text]